Computer-aided dental implant planning increases the predictability of replacing missing teeth in partially and fully edentulous cases. This article describes how Nobel Biocare’s Procera surgical planning software converts a patient’s double CT scan data into a virtual three-dimensional model of the alveolar bone and overlying prosthesis. Using these images, the practitioner virtually places implants in the bone in precise relation to their position in the final prosthesis. Procera uses this virtual plan to fabricate a customized surgical template that guides the placement of the implants safely, precisely, and accurately. Then the dental laboratory can construct the master cast and provisional restoration before surgery, allowing the restoration to be inserted immediately after placement of the implants. Furthermore, computer-based guided implant surgery is minimally invasive and requires a shorter chair time and fewer appointments than traditional methods.
Advances in implant dentistry over the past 40 years have allowed for the predictable replacement of missing teeth . It is now commonplace to treatment plan partially and fully edentulous areas in the mouth with implant-supported restorations. In the standard planning for a dental implant case, the doctor procures mounted dental models and designs a model-based surgical guide. Conventional dental radiographs and CT scans help the practitioner determine where the underlying bone relates to the final prosthesis . But in most cases, to determine the anatomy of the alveolar ridge, the surgery requires a crestal incision with subperiosteal reflection of the gingiva, a method that can inadvertently displace the model-based surgical guide. Only in those cases that present with excess amounts of alveolar bone can the implant be placed in a flapless manner. Even with a model-based surgical guide, much depends on the skill of the operator in placing the implant in the preplanned position. The use of model-based guides to position dental implants becomes even more demanding in placing multiple implants, as in an edentulous arch with limited bone available.
In the past few years, technologic advances in interactive three-dimensional CT software have enabled the practitioner to treatment plan and place dental implants more predictably . Computer-based planning is used to plan implant placement in partially edentulous (single tooth, multiple teeth) and, more often, fully edentulous cases involving a single arch or both arches. One surgical planning software, Procera Planning Software (Nobel Biocare, Yorba Linda, California), converts the patient’s CT scan data into a three-dimensional model of the patient’s facial bones and generates a three-dimensional representation of the proposed prosthesis in relation to the underlying alveolar ridge. The implants can be virtually placed in optimal sites, taking into account the patient’s bone anatomy and the overlying position of the prosthesis. The computer-based plan is then used to create a customized surgical template that precisely guides the placement of the implants during surgery (NobelGuide). The dental laboratory uses the surgical template to fabricate the master cast and the provisional or final prosthesis.
The computer-based guided implant placement approach has numerous advantages. The presurgical planning and surgery are prosthetically driven and emphasize the team approach among the restorative dentist, surgeon, and dental laboratory. The surgeon can place the implants in their optimal and exact positions more accurately, predictably, and safely, as planned in the virtual software. Vital structures, such as adjacent tooth roots and the inferior alveolar nerve, can be avoided. The surgical template is so precise that the implants can be placed in minimal amounts of available bone, including those cases that would traditionally require bone grafting. In the severely atrophic maxilla, pterygomaxillary implants can be placed accurately with the use of the surgical template . The minimally invasive guided surgery is performed without raising a flap, thereby minimizing postoperative pain and swelling and postoperative recovery time . The chair time and number of appointments are also reduced, facilitating many patients’ busy lifestyles. With the information contained within the surgical template, the dental laboratory can presurgically construct the master cast and the subsequent fabrication of a provisional restoration that can be inserted at the time of surgery (Teeth-in-an-Hour) or soon thereafter. Clinical studies support the long-term success of immediately loaded implants placed in a flapless manner and restored with a fixed complete restoration .
This article describes the process of computer-based guided implant surgery and the placement of an immediate provisional fixed prosthesis using Nobel Biocare’s Procera planning software and the NobelGuide treatment approach, as performed in the author’s office setting.
Presurgical evaluation and planning
The surgeon initially evaluates the patient with a thorough clinical and radiograph examination, including a preliminary cone-beam CT scan (also known as cone-beam volumetric tomography scan), digital photographs, and mounted dental models. The amount of available bone is assessed and nonrestorable teeth are identified. The nonrestorable teeth are removed and extraction sockets are bone grafted along with areas that have insufficient bone volume to place implants. The extraction sockets and bone grafts are allowed to consolidate completely. The patient must be able to open his/her mouth sufficiently to accommodate the additional 10-mm length of the burs used with the surgical template to prepare the implant sites.
The restorative dentist then fabricates dentures with the teeth in the ideal centric occlusion and in appropriate position for phonetics, aesthetics, and vertical dimension. The position of the teeth will be duplicated in the final fixed restoration, so the patient and practitioner must agree to the set-up. The prosthesis is made of acrylic and should not include a radiopaque liner. The denture should have exceptional soft tissue adaptation with an exact fit to the underlying mucosa. The flanges should be a minimum of 3-mm thick and overextended into the buccal and labial vestibules. In partially edentulous cases, once the ideal occlusion is established, an additional 3-mm thickness of acrylic is added to cover the occlusal surfaces of the existing teeth, and inspection windows are placed. The palate is also covered with acrylic to stabilize the denture further. In mandibular cases, the denture is extended to cover the retromolar area. All the features of the denture are reproduced in the surgical template.
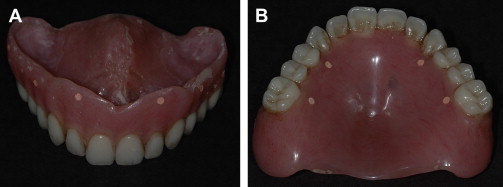
The denture, or an exact duplicate, is then prepared as the radiographic guide. Ten to twelve fiducial markers are placed in a staggered pattern and at different levels to the occlusal plane on the buccal flanges and palatal and lingual surfaces. Each site is prepared with a #4 round bur to approximately 2-mm wide and 1.5-mm deep and filled with gutta percha (Coltene-Whaledent, Cuyahoga Falls, Ohio) ( Fig. 1 ). A rigid vinyl polysiloxane bite registration, taken in centric occlusion, will be used to stabilize the radiographic guide against the opposing dentition during the CT scanning procedure.
Two cone-beam CT scans are made, with acquisition slices of 0.4 mm: the first, of the patient wearing the radiographic guide while occluding into the bite registration, and the second, of the radiographic guide alone, positioned in approximately the same orientation as in the first scan. These two Digital Imaging and Communication in Medicine (DICOM)-3 formatted files are then imported into the Procera planning software and the data are converted into three-dimensional representations of the patient’s alveolar bone and of the radiographic guide. The radiographic markers allow for the fusion of these two scans, thereby showing the relationship of the denture teeth to the underlying bone.
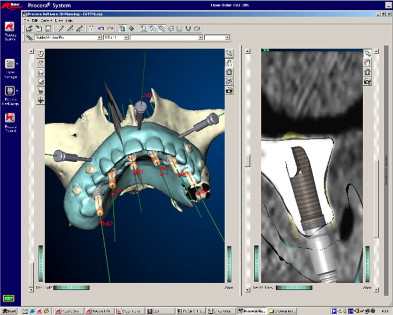
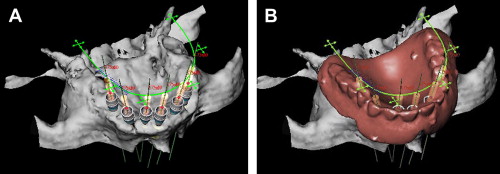
The virtual placement of the implants can now be performed. The Procera planning software uses a three-dimensional screen and a two-dimensional panel ( Fig. 2 ). Both screens interrelate, so changes shown in one screen are visualized in the other. The two-dimensional view allows for visualization of cross-sections of the alveolar bone along a slice curve in the three-dimensional screen. Using three-dimensional and cross-sectional views of the alveolar bone, along with an image of the overlying virtual prosthesis in exact relationship to the underlying bone, the implants can be virtually placed in the bone in relation to the position of the teeth in the final prosthesis. The three-dimensional image can be rotated in all spatial planes to assess the bony anatomy. The implant abutment and guide sleeve of the surgical template can be placed with each implant. The internal diameter of the guide sleeves corresponds precisely to the diameters of the drill guides and implants. Depending on which details need to be visualized, certain features of the virtual plan can be displayed or hidden (eg, the prosthesis, cross-sectional reslices, bone, or implant abutments) ( Fig. 3 ). Additionally, horizontal stabilization pins (a minimum of one in partially edentulous cases and up to four in edentulous cases) are virtually placed through the labial denture flange to anchor the surgical template during surgery. After the restorative dentist and surgeon approve the virtual treatment plan, the three-dimensional computer planning files are digitally sent through the Internet to the Procera manufacturing facility (Nobel Biocare) for fabrication of the stereolithically constructed surgical template ( Fig. 4 ). A map is printed from the planning software, depicting the size and location of each implant within the surgical template.

Approximately 2 weeks later, the surgical template is delivered to the office and a try-in is scheduled to confirm the accuracy of its fit. Thin and undersupported areas of the surgical template are reinforced with light-cured Triad gel (Dentsply International, York, Pennsylvania). In cases where an immediate provisional restoration is not planned, the patient can now be scheduled for surgery. For those cases in which an immediate provisional prosthesis will be inserted at the time of surgery or soon thereafter, the surgical template is sent to the dental laboratory, along with an opposing dental model, duplicate denture, and the interocclusal index used with the radiographic guide during the CT scan. The exactness of the surgical template allows for the presurgical construction of the master cast ( Fig. 5 ) and the subsequent presurgical fabrication of a provisional restoration ( Fig. 6 ) . The dental laboratory uses the duplicate denture and interocclusal index to mount the master cast anatomically against the opposing dentition. A surgical index of rigid vinyl polysiloxane is prepared of the surgical template positioned on the articulated master cast occluding with the opposing dentition. The provisional restoration, surgical index, articulated models, and abutment components are delivered to the office and the patient is scheduled for surgery.


Surgical procedure
Once the patient is prepared and draped and, if necessary, sedated, local anesthesia is injected, and the surgical template is placed and positioned with the surgical index. The patient is instructed to occlude into the index for 10 minutes to dissipate the local anesthesia, thereby ensuring that the surgical template is exactly seated on the underlying mucosa ( Fig. 7 ). Then, with the patient biting firmly into the surgical index, a 1.5-mm twist drill is used to prepare the stabilization pin sites, the pins are placed ( Fig. 8 ), and the surgical index is removed. A tissue punch ( Fig. 9 ) is used to remove a core of gingiva from each guide sleeve and the initial implant preparation is begun with the counterbore starter drill ( Fig. 10 ). Successive-sized twist drills with drill-stops are used with corresponding twist drill sleeves to prepare each implant site to the exact position and depth as determined in the virtual plan ( Fig. 11 ). The preparation is undersized in diameter in soft bone, and in dense bone, a bone tap is used after the final width of the implant site is prepared. All burs are externally irrigated with copious amounts of cold saline, and the burs are used in a “pumping” fashion to allow the irrigant to flow to the apex of the preparation to prevent overheating of the bone. The implant is connected to a guided implant mount ( Fig. 12 ) and inserted into the prepared osteotomy site with the torque wrench or implant drill. The implant is inserted to the depth at which the implant mount contacts the drill guide sleeve in the surgical template. Overtightening the implant can displace, and possibly fracture, the surgical template. In softer bone, overtightening can cause the implant threads to strip the preparation, and the implant will “spin,” losing its initial stability in bone. In edentulous cases, after the initial two implants are placed, the guided implant mounts are removed and template abutments with expanding sidewalls that contact the inner aspect of the guide sleeves are placed on the initial two implants. These abutments further stabilize the surgical template while the additional implant sites are prepared ( Fig. 13 ). For a partially edentulous case, usually only one template abutment is needed.





