Before any definitive treatment of mandibular fractures, the patient needs to be evaluated for more potentially life-threatening injuries. Complications can and do occur with treatment of mandibular fractures and can occur during any of the phases of treatment. The development of an accurate diagnosis and appropriate treatment plan is vital in achieving optimal success and decreasing complications. Knowledge of the anatomy and the principles of bone healing is also an important factor in preventing complications. To limit long-term untoward effects, complications should be recognized early and the appropriate treatment should be started before a minor complication becomes a complex one that is more difficult to manage.
A complication is a problem that arises as a consequence of an initial condition or as a result of treatment. Because of its prominent position in the facial skeleton and the complex nature of the anatomy and environment in which it resides, the mandible is extremely susceptible, and thus frequently fractured when a traumatic insult is directed at the face. In addition, the anatomic architecture and presence of teeth create inherent areas of weakness and place the mandible at further risk for fracture. Complications involving mandibular fractures are a consequence of a myriad of factors. As such, they may be secondary to the original injury, a result of the subsequent treatment, or, in some cases, a result of failure to render treatment. Complications of mandibular fractures have an increased relevance because of the important role that the mandible plays in the establishment of occlusion, function, and facial esthetics.
Complications can present as an immediate problem at the time of injury, or they can become manifest during the operative or postoperative phase of treatment. Postoperative complications can become evident early on or some time after treatment has been instituted. In fact, some problems may not become evident for months or years after the injury. Complications of mandibular fractures can involve the entire spectrum, ranging from minor complications with little residual consequence to those having dire consequences with long-term deficits and even death.
Immediate complications
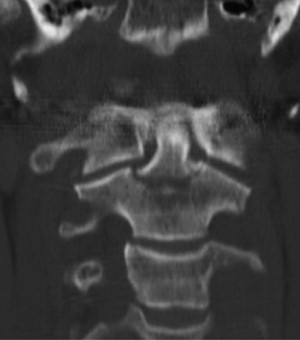
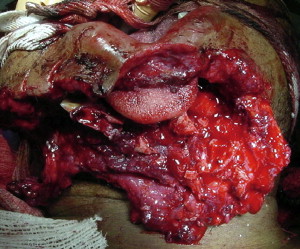
Because of the size, shape, and thickness of the mandible, any insult sufficient enough to cause a fracture of the mandible can readily result in concomitant intra-abdominal, intrathoracic, intracranial, or cervical injury ( Fig. 1 ). In addition, it is not unusual to have simultaneous significant soft tissue injury resulting in significant edema and copious hemorrhage with the potential for airway compromise or hypovolemic shock ( Fig. 2 ). Although in many instances of mandibular fracture, the oral and maxillofacial surgeon is consulted after the patient has been evaluated and stabilized by the trauma team or emergency department staff, it still behooves the sagacious practitioner to evaluate the patient appropriately for problems that may be life threatening, and thus take priority over the maxillofacial injury. Appropriate consultation with suitable imaging should be obtained if any of these more imperative injuries are suspected.
Airway compromise
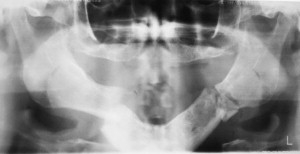
Airway compromise may be a direct result of the mandibular fracture attributable to swelling, bleeding, foreign body aspiration, or amount of displacement, in addition to the nature of the fracture. The amount of swelling is a consequence of the severity of the injury and the degree of soft tissue involvement. Swelling can be decreased by the use of steroids immediately after trauma unless contraindicated by the patient’s medical history or current condition. Preliminary reduction and immobilization may be necessary in severely displaced fractures or in the situation of bilateral body fractures because of the lack of anterior support for the tongue with prolapse to the posterior pharynx and subsequent airway compromise ( Fig. 3 ). The use of an oropharyngeal airway in the unconscious patient or bilateral nasopharyngeal airways in the conscious patient may help to alleviate airway compromise. In cases of severe compromise, intubation or tracheotomy may be required. Airway problems associated with concomitant intrathoracic or intracranial causes should be addressed by the appropriate surgical specialty before attempting any treatment of the mandibular fracture.
Bleeding
Although soft tissue or osseous bleeding is not uncommon, significant hemorrhage after mandibular fractures is a rare occurrence. If the trauma results in transection of a major vessel within the bone or the surrounding soft tissue, hemorrhage can be severe with life-threatening consequences because of the potential for hypovolemic shock or hematoma leading to airway compromise. Arrest of bleeding should be attempted by local measures initially; if such measures are unsuccessful, isolation and ligation of the offending vessel should be entertained. The application of initial reduction and temporary fixation may be helpful in stopping or decreasing bleeding because of its resulting tamponade effect. In rare cases, embolization of the offending vessel or external carotid artery ligation may be required.
Loss of or damage to teeth or bone
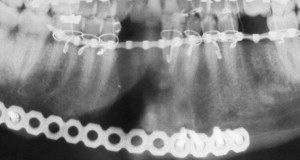
Because of the vulnerable position of the teeth, a fracture of the mandible is frequently associated with concomitant injury to the teeth or alveolar bone ( Fig. 4 ). Teeth can be fractured, mobilized, or avulsed when a mandibular fracture occurs. This may require debridement, fixation, extraction, or endodontic therapy. Because establishment of correct occlusion is the sine qua non to treating mandibular fractures successfully, the loss of teeth or alveolar bone fracture may compromise reduction of the mandibular fracture and may necessitate an open rather than closed procedure or construction of a surgical stent. Teeth that become nonvital during the healing phase can cause infection and interfere with fracture healing. It is suggested that all compromised teeth be treated early to lessen the chance of this occurring ( Fig. 5 ). Questionable teeth in the line of fracture have special relevance and are addressed in another article in this issue.

Delayed complications
Nonunion
A nonunion is the lack of osseous union by two or more fracture segments after the usual 6- to 8-week healing period. Fortunately, nonunion of mandibular fractures is not a common occurrence. In some instances, no additional treatment is required because the nonunion responds to conservative management consisting only of an increased period of immobilization. This is particularly evident when there is limited bone volume or the patient has a decreased healing capacity attributable to age or concomitant medical conditions or medications. If conservative management is not successful, a second surgical intervention for correction may be required. There are many reasons why a fracture does not go on to bony union, including interference in the reduction or immobilization of the fracture and the development of infection with a resultant loss of bone ( Fig. 6 ). Inadequate reduction with a gap between fracture segments or the interposition of soft tissue that prevents bone-to-bone contact can cause a nonunion. Excessive mobility has the propensity to prevent the initial callus formation necessary for subsequent bone formation and maturation that may go on to develop a fibrous union. In the case of closed reduction, this may result from inadequate or loose intermaxillary fixation causing macromovement of the fracture segments. For complete or partial edentulism, an insufficient number of teeth may be available for adequate immobilization and a surgical stent may be necessary for to prevent or minimize mobility. In contaminated cases or those treated by means of an open approach, infection may act as the causative agent in causing a nonunion. When rigid fixation is used, infection can result from screw loosening with subsequent fracture site mobility. Infection can also result in the destruction and loss of bone at the fracture site with a lack of bony contact, and thus the inability to form an osseous union. In addition to infection, large gaps can be caused by loss of bone because of the nature of the injury, as is frequently seen with high-energy wounds.
Additional causes of mandibular complications are impacted teeth present at the fracture site that require removal for adequate reduction and pathologic entities, such as cysts or neoplasm. The patient’s age and systemic health may also play a role in the development of a nonunion. The elderly patient has a greater chance of a nonunion for two reasons. An elderly patient’s reduced ability to form a bony union may attributable to a decrease in age-related healing factors, and there is often a decrease in bone height and width ( Fig. 7 ) attributable to the normal resorptive process that occurs with loss of teeth and aging. This lack of bone quality and quantity compromises the vascularity of the bone, further complicating healing. Any concomitant medical or systemic condition or medications that the patient may be taking can result in a nonunion by altering or interfering with the natural healing potential of the body.

The treatment of nonunion depends on the cause and the resultant deformity or defect. In most cases, an open procedure is required to visualize the fracture and to remove any tissue present between segments. After all soft tissue or infected material is removed, the patient is placed in occlusion with maxillomandibular fixation while the fracture is reduced. If there is good bone-to-bone contact, the fracture segments are rigidly fixated. In the event that bone has been lost because of infection or loss of vascularity, the ends of the fracture segments are freshened to reveal vital bleeding bone and a bone graft is placed between the segments if infection has resolved with the placement of a bicortical reconstruction plate.
Malunion
Malunion occurs when fracture segments are not properly reduced or fixated, and bony union takes place in a less than ideal position. An important way to decrease this complication is to place the patient carefully in the appropriate occlusion before any surgical intervention; at that time, the fracture is reduced and fixated. Many times, a malunion manifests clinically as a malocclusion, an inability to function normally, and, in some cases, an obvious facial deformity ( Fig. 8 ). A malunion can occur because of a poor treatment plan; surgical error; or when there are missing or carious teeth, multiple fractures, or concomitant alveolar fractures that prevent the establishment of the proper occlusion. The correct treatment plan (ie, open versus closed reduction), external appliances, or stent construction should be based on the degree of fracture displacement, the location, the amount of bone loss or comminution, and the lack or presence of a sufficient number of teeth to establish adequate occlusion.





