Introduction
Open bites are known to be difficult malocclusions to treat. Generally, with conventional edgewise treatment, incisor extrusion rather than molar intrusion is observed. Recently, the use of miniscrews as anchorage has markedly increased. In this study, orthodontic treatment outcomes after conventional edgewise treatment and implant-anchored treatment were investigated by cephalometric analysis and several occlusal indexes. In addition, the stability of these patients 2 years after the retention phase was also analyzed.
Methods
Thirty adults (15 for nonimplant treatment [non-IA group] and 15 for implant-anchored treatment [IA group]) were our subjects. Cephalometric analysis, peer assessment rating, discrepancy index, and objective grading system were used.
Results
From the cephalometric values in the non-IA group, open-bite patients were generally treated by extrusion of the maxillary and mandibular incisors that resulted in clockwise rotation of the mandibular plane angle. In the IA group, intrusion of the maxillary and mandibular molars that resulted in counterclockwise rotation was noted. Furthermore, in the IA group, the soft-tissue analysis showed decreases in the facial convexity and the inferior labial sulcus angle that resulted in the disappearance of incompetent lips. In the retention phase, extrusion of the mandibular molars was observed in the IA group. From the objective grading system evaluation, significant reductions of overbite in canines and premolars were observed in both groups. Furthermore, less stability was observed in the IA group compared with the non-IA group according to the total objective grading system score.
Conclusions
Ideal occlusion can be achieved in adults with severe open bite with both conventional edgewise and implant-anchored orthodontic treatment. However, absolute intrusion of the molars and improvement in esthetics might be achieved more effectively by using miniscrews as an anchorage device. In addition, since a significant amount of tooth movement occurs with miniscrews, careful attention is required during the retention phase.
Skeletal open bite is known to be one of the most difficult malocclusions to treat in orthodontics. Since the cause of open bite is related to unfavorable growth pattern, tongue posture and function, habits, and nasopharyngeal airway obstructions, an orthopedic approach during the deciduous or mixed dentition periods might result in favorable treatment results. In growing patients, high-pull headgear, habit-breaking appliances, bite-blocks, and vertical chincups are generally used to decrease the vertical dimension of the dentoalveolar process. If there is an increase in growth at the posterior vertical facial height, counterclockwise mandibular rotation occurs, resulting in a decrease in the amount of open bite.
On the other hand, in nongrowing patients, vertical control tends to be difficult without growth. Dental compensations are generally observed with conventional orthodontic treatment such as extrusion of incisors or molars resulting in clockwise rotation of the mandible that leads to unfavorable treatment outcomes. Treatment options for nongrowing patients include the use of elastics combined with the multiloop edgewise archwire technique or nickel-titanium archwires.
The use of titanium miniplates or miniscrews as orthodontic anchorage devices in correcting patients with open bite has been reported. With these miniplates and miniscrews, significant amounts of intrusion of the molars are possible, resulting in counterclockwise rotation of the mandible. Recently, we reported a comparative study on the outcomes between implant-anchored orthodontic treatments and surgically treated patients with open bite. In that report, both treatment methods resulted in acceptable outcomes, such as increased overbite and reduced total facial height. Moreover, in patients treated by implant-anchored orthodontics, an increase in the amount of overbite was achieved by intrusion of the molars rather than via extrusion of the incisors that was the result of surgically corrected patients with open bite. However, no study has compared the treatment outcomes between implant-anchored orthodontics and conventional orthodontics in treating these patients.
In this study, quantitative evaluations of the orthodontic treatment outcomes of skeletal and facial features and soft tissues were undertaken with cephalometric analysis, and of dental (occlusal) features by the peer assessment rating (PAR), the discrepancy index (DI), and the objective grading system (OGS) between implant-anchored and conventional orthodontics in adults with skeletal open bite. In addition, skeletal and dental stabilities after 2 years of retention were also analyzed between the groups.
Material and methods
A total of 30 consecutively finished adult patients (ages, 18 to 46 years; mean ± SD, 24.3 ± 5.9 years) from 2002 to 2005 with an anterior open bite of more than 3.0 mm (range, −3.0 to −7.5 mm; mean ± SD, −4.6 ± 1.4 mm) were analyzed. We excluded patients less than 18 years old at the start of treatment, those without appropriate records, those who transferred from other clinics, and those who had phase 1 treatment.
Patients undergoing conventional edgewise treatment without implants as anchorage (non-IA group) included 15 women (mean age, 22.9 ± 4.9 years; average open bite, −4.6 ± 1.5 mm; range, −3.0 to −7.5 mm). In the non-IA group, 4 patients were skeletal Class I, and 11 patients were Class II. All patients were treated with premolar extractions. The non-IA group was treated with a combination of anterior elastics and either accentuated-curve archwires or the multiloop edgewise archwire technique. High-pull headgear was also used in all patients in this study. In addition, before the start of edgewise treatment, all patients were evaluated with a myofunctional checklist, which included (1) size of the adenoids, (2) the presence of vomiting reflex, (3) size of the tongue, (4) any abnormality in the lingual frenum, (5) position of the tongue at rest, (6) lip condition during rest, (7) any lip or chin (mentalis) strain, (8) whether the patient bites during swallowing, (9) condition of the palate (hard and soft) during rest and swallowing, (10) activity of the masseter muscle, (11) lip strength, (12) maximum opening, and (13) presence of mouth breathing. The subjects also answered a questionnaire including a history of habits.
The other group of 15 female patients (mean age, 25.7 ± 6.4 years; average open bite, −4.4 ± 1.2 mm; range, −3.0 to −7.4 mm) was treated with miniscrews as anchorage (IA group). The IA group also consisted of 5 patients with skeletal Class I and 10 patients with Class II. All were treated with premolar extractions.
In the IA group, miniscrews (Absoanchor, Dentos, Taegu, Korea; diameter, 1.3 mm, length, 6-8 mm; Gebrüder Martin, Tuttlingen, Germany; diameter, 1.5 mm, length, 9 mm) were placed under local anesthesia between either the second premolar and the first molar or the first and second molars in the buccal region by the orthodontist. The miniscrews were loaded 0 to 4 weeks after placement. Before miniscrew placement, sectional archwires of 0.016 × 0.022-in stainless steel were placed from the second premolar to the second molar. Intrusion was performed by using either a power chain or ligature wires from the miniscrew to the sectional archwire. Generally, incisor and canine brackets were bonded after the overbite had in an edge-to-edge relationship.
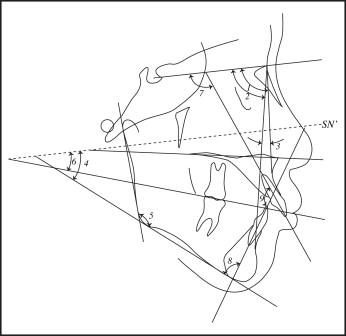
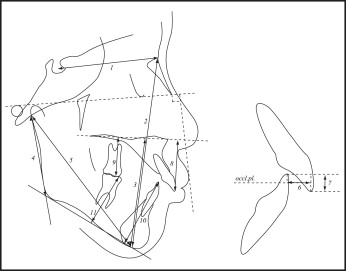
The initial occlusion was evaluated by using the PAR ( Table I ) and the DI ( Table II ). Cephalometric radiographs were taken before and after treatment for cephalometric evaluation ( Figs 1 and 2 ; Table III ) and soft-tissue analysis ( Fig 3 ; Table IV ) in both groups. Soft-tissue measurements were analyzed according to a previous study. Final occlusion was evaluated by using the OGS ( Table V ) and the PAR in both groups. All cephalometric tracings and measurements were made by the same examiner (T.D.). All cephalometric measurements were repeated after 4 weeks, and the method error was calculated from the equation:
where S x is the error of the measurement, D is the difference between duplicated measurements, and N is the number of double measurements. The errors of the measurements were 0.18 mm.
| PAR | Non-IA group | IA group | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pretreatment | Posttreatment | Retention | Pretreatment | Posttreatment | Retention | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Mx. ant. | 3.6 | 2.2 | 0.0 ∗ | 0.0 | 0.2 | 0.4 | 3.0 | 2.2 | 0.0 ∗ | 0.0 | 0 | 0 |
| Mx. post. | 5.9 | 3.5 | 1.0 ∗ | 1.4 | 1.7 | 1.8 | 4.9 | 3.7 | 1.3 ∗ | 1.0 | 1.6 | 1.8 |
| Md. ant. | 2.1 | 2.6 | 0.4 ∗ | 0.7 | 0.3 | 0.6 | 1.9 | 2.2 | 0.1 ∗ | 0.4 | 0.3 | 0.9 |
| Md. post. | 5.7 | 3.5 | 0.7 ∗ | 0.6 | 1.6 | 1.5 | 4.0 | 2.9 | 0.8 ∗ | 1.0 | 1.1 | 1.2 |
| AP | 1.8 | 1.6 | 0.3 ∗ | 0.6 | 0.6 | 0.9 | 1.3 | 0.9 | 0.1 ∗ | 0.4 | 0.3 | 0.5 |
| Vertical | 1.1 | 1.5 | 0.2 ∗ | 0.4 | 0.1 | 0.3 | 1.1 | 0.8 | 0.2 ∗ | 0.6 | 0.2 | 0.4 |
| Transverse | 2.2 | 1.8 | 0.1 ∗ | 0.4 | 0.2 | 0.6 | 2.1 | 1.6 | 0.1 ∗ | 0.4 | 0.5 | 1.2 |
| Overjet | 2.3 | 1.3 | 0.1 ∗ | 0.4 | 0.6 | 0.8 | 2.3 | 1.3 | 0.3 ∗ | 0.5 | 0.4 | 0.5 |
| Overbite | 2.9 | 1.2 | 0.1 ∗ | 0.3 | 0.2 | 0.4 | 2.5 | 0.9 | 0.1 ∗ | 0.4 | 0.1 | 0.3 |
| Midline | 0.3 | 0.5 | 0.1 | 0.3 | 0 | 0 | 0.4 | 0.5 | 0.1 | 0.4 | 0 | 0 |
| Total | 28.0 | 9.4 | 3.0 ∗ | 2.9 | 5.5 | 2.8 | 23.5 | 8.6 | 3.5 ∗ | 2.2 | 4.4 | 2.9 |
∗ Significant difference compared with pretreatment ( P <0.05).
| DI | Non-IA | IA | Significance | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| OJ | 2.9 | 1.8 | 3.5 | 1.9 | NS |
| OB | 0 | 0 | 0 | 0 | NS |
| AOB | 26.4 | 12.8 | 32.9 | 12.7 | NS |
| LOB | 6.8 | 8.3 | 7.3 | 11.4 | NS |
| Crowd | 2.9 | 2.7 | 2.3 | 2.6 | NS |
| Occl | 3.4 | 2.3 | 2.5 | 2.2 | NS |
| LPX | 2.1 | 2.2 | 1.7 | 2.0 | NS |
| BPX | 0.7 | 1.0 | 0.7 | 1.2 | NS |
| ANB | 5.1 | 3.4 | 5.3 | 3.2 | NS |
| SNMp | 13.3 | 8.3 | 17.5 | 11.4 | NS |
| IMPA | 1.3 | 2.7 | 1.2 | 2.7 | NS |
| Total | 62.4 | 26.7 | 76.9 | 30.1 | NS |
| Variables | Non-IA group | IA group | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pretreatment | Posttreatment | Difference | Retention | Difference | Pretreatment | Posttreatment | Difference | Retention | Difference | |||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Angular (°) | ||||||||||||||||||||
| SNA | 82.0 | 3.1 | 81.8 | 2.9 | −0.3 | 1.0 | 82.2 | 2.8 | 0.4 | 0.5 | 81.1 | 4.2 | 80.8 | 4.5 | −0.2 | 0.9 | 81.1 | 4.5 | 0.3 | 0.5 |
| SNB | 76.6 | 3.4 | 76.4 | 3.4 | −0.2 | 1.0 | 77.1 | 3.3 | 0.7 | 1.1 | 75.3 | 6.0 | 76.7 | 6.6 | 1.4 † | 1.1 | 76.8 | 6.9 | 0.1 | 1.2 |
| ANB | 5.4 | 2.4 | 5.4 | 2.4 | 0.0 | 1.5 | 5.1 | 2.2 | −0.3 | 1.1 | 5.7 | 3.6 | 4.2 | 4.1 | −1.6 † | 1.0 | 4.3 | 4.2 | 0.2 | 1.3 |
| Mp-SN | 43.0 | 4.3 | 45.7 | 4.5 | 2.7 ∗ | 3.2 | 46.0 | 4.6 | 0.3 | 1.6 | 45.8 | 6.0 | 42.2 | 6.7 | −3.6 ∗ † | 2.1 | 43.8 | 6.5 | 1.6 | 2.7 |
| Go.A | 127.3 | 5.5 | 128.0 | 4.8 | 0.7 | 1.5 | 128.1 | 3.8 | 0.1 | 1.8 | 127.3 | 5.1 | 126.8 | 5.0 | −0.5 † | 1.4 | 126.8 | 5.1 | 0.1 | 1.6 |
| Occl Pl | 22.7 | 5.8 | 24.5 | 5.0 | 1.8 | 2.9 | 24.4 | 4.2 | −0.2 | 1.7 | 20.9 | 5.1 | 19.5 | 4.7 | −1.4 † | 1.6 | 20.3 | 5.1 | 0.8 | 0.9 |
| SN-U1 | 109.7 | 11.2 | 104.4 | 10.4 | −5.3 | 3.2 | 105.3 | 10.1 | 0.9 | 1.8 | 110.7 | 8.0 | 105.4 | 9.8 | −5.3 | 4.2 | 105.0 | 9.8 | −0.4 | 1.4 |
| L1-Mp | 94.9 | 7.9 | 93.2 | 6.2 | −1.7 | 3.9 | 94.9 | 5.6 | 1.7 | 2.0 | 94.3 | 5.6 | 92.6 | 5.7 | −1.7 | 2.4 | 93.4 | 5.0 | 0.8 | 2.2 |
| IIA | 117.7 | 7.0 | 123.6 | 5.6 | 5.9 ∗ | 4.4 | 121.8 | 6.1 | −1.9 | 2.5 | 111.6 | 8.4 | 118.3 | 6.5 | 6.7 ∗ | 5.8 | 118.3 | 6.5 | 0 | 1.1 |
| Linear (mm) | ||||||||||||||||||||
| S-N | 70.1 | 4.1 | 70.7 | 4.0 | 0.5 | 0.9 | 71.0 | 3.9 | 0.3 | 0.7 | 70.1 | 2.8 | 70.3 | 2.9 | 0.2 | 0.3 | 70.6 | 2.9 | 0.3 | 0.6 |
| N-Me | 132.8 | 7.4 | 135.7 | 6.7 | 2.9 | 1.7 | 136.7 | 7.0 | 1.0 | 1.0 | 134.6 | 6.7 | 131.0 | 6.7 | −3.6 † | 3.8 | 131.2 | 6.5 | 0.2 | 0.5 |
| Me/NF | 75.3 | 5.4 | 78.0 | 5.5 | 2.7 | 0.9 | 78.8 | 5.4 | 0.8 | 0.6 | 74.7 | 5.9 | 72.2 | 5.1 | −2.6 † | 2.5 | 72.2 | 5.1 | 0.8 | 1.1 |
| Ar-Go | 46.5 | 3.6 | 46.6 | 4.0 | 0.1 | 1.9 | 47.0 | 3.1 | 0.4 | 2.0 | 44.1 | 6.0 | 44.5 | 6.6 | 0.4 | 2.7 | 45.4 | 6.5 | 0.9 | 0.9 |
| Ar-Me | 106.7 | 5.1 | 107.0 | 5.6 | 0.3 | 1.6 | 107.5 | 5.3 | 0.4 | 1.4 | 106.5 | 7.9 | 106.1 | 7.7 | −0.3 | 2.1 | 107.0 | 7.5 | 0.9 | 0.9 |
| OJ | 5.5 | 2.6 | 2.3 | 0.6 | −3.1 ∗ | 2.4 | 2.0 | 0.6 | −0.3 | 0.6 | 4.9 | 3.4 | 1.9 | 1.0 | −3.0 ∗ | 2.9 | 2.2 | 1.0 | 0.3 | 0.5 |
| OB | −4.6 | 1.5 | 1.9 | 1.1 | 6.5 ∗ | 2.2 | 1.4 | 0.9 | −0.5 | 1.4 | −4.4 | 1.2 | 1.8 | 1.1 | 6.2 ∗ | 1.7 | 1.0 | 0.9 | −0.8 | 1.1 |
| PP-U1 | 31.9 | 3.0 | 35.4 | 2.6 | 3.5 ∗ | 1.9 | 35.2 | 3.1 | −0.2 | 1.4 | 32.4 | 2.3 | 33.4 | 2.3 | 1.0 † | 1.6 | 33.4 | 2.3 | 0.1 † | 1.2 |
| PP-U6 | 25.5 | 3.3 | 26.9 | 3.4 | 1.5 | 1.3 | 27.6 | 3.1 | 0.6 | 1.4 | 26.9 | 3.0 | 24.6 | 2.5 | −2.3 ∗ † | 1.3 | 25.1 | 2.8 | 0.5 | 0.9 |
| Mp-L1 | 47.2 | 3.7 | 49.0 | 4.3 | 1.8 ∗ | 1.8 | 49.1 | 4.5 | 0.1 | 0.8 | 46.3 | 3.4 | 46.6 | 2.8 | 0.3 | 2.3 | 46.3 | 3.1 | −0.3 | 1.3 |
| Mp-L6 | 37.0 | 2.9 | 38.5 | 2.9 | 1.5 | 0.6 | 39.0 | 3.1 | 0.6 | 2.1 | 36.0 | 2.5 | 35.2 | 1.9 | −0.8 † | 1.3 | 37.0 | 1.9 | 1.7 ∗ | 1.0 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


