Introduction
The aim of this prospective clinical study was to evaluate the skeletal, dentoalveolar, and soft-tissue effects of maxillary protraction with miniplates compared with conventional facemask therapy and an untreated Class III control group.
Methods
Forty-five subjects who were in prepubertal or pubertal skeletal growth periods were included in the study and divided into 3 groups of 15 patients each. All subjects had skeletal and dental Class III malocclusions with maxillary deficiency, vertically normal growth pattern, anterior crossbite, Angle Class III molar relationship, normal or increased overbite, and retrusive nasomaxillary complex. Before maxillary protraction, rapid maxillary expansion with a bonded appliance was performed in both treatment groups. In the first group (MP+FM), consisting of 5 girls ande 10 boys (mean age, 10.91 years), facemasks were applied from 2 titanium miniplates surgically placed laterally to the apertura piriformis regions of the maxilla. The second group (FM) of 7 girls and 8 boys (mean age, 10.31 years) received maxillary protraction therapy with conventional facemasks applied from hooks of the rapid maxillary expansion appliance. The third group of 8 girls and 7 boys (mean age, 10.05 years) was the untreated control group. Lateral cephalometric films were obtained at the beginning and end of treatment or observation in all groups and analyzed according to a structural superimposition method. Measurements were evaulated statistically with Wilcoxon and Kruskal-Wallis tests.
Results
Treatment periods were 6.78 and 9.45 months in the MP+FM and FM groups, respectively, and the observation period in the control group was 7.59 months. The differences were significant between the 3 groups ( P <0.05) and the MP+FM and FM groups ( P <0.001). The maxilla moved forward for 2.3 mm in the MP+FM group and 1.83 mm in the FM group with maxillary protraction. The difference was significant between 2 groups ( P <0.001). The protraction rates were 0.45 mm per month in the MP+FM group and 0.24 mm per month in the FM group ( P <0.001). The maxilla showed anterior rotation after facemask therapy in the FM group ( P <0.01); there was no significant rotation in the MP+FM group. Posterior rotation of the mandible and increased facial height were more evident in the FM group compared with the MP+FM group ( P <0.01). Both the maxilla and the mandible moved forward significantly in the control group. Protrusion and mesialization of the maxillary teeth in the FM group were eliminated in the MP+FM group. The maxillomandibular relationships and the soft-tissue profile were improved remarkably in both treatment groups.
Conclusions
The undesired effects of conventional facemask therapy were reduced or eliminated with miniplate anchorage, and efficient maxillary protraction was achieved in a shorter treatment period.
Class III malocclusions are considered to be among the most challenging orthodontic problems to treat. The prevalence of Class III malocclusions is approximately 1% to 5% in white populations. However, in Asian populations, the incidence of this malocclusion is as high as 14%. A Class III malocclusion might be due to mandibular prognathism, maxillary retrognathism, protrusive mandibular dentition, retrusive maxillary dentition, and a combination of these components. It has been reported that two thirds of skeletal Class III malocclusions are due to either maxillary retrognathism or a combination of maxillary retrognathism and mandibular prognathism.
Early treatment is commonly indicated to obtain a more normal jaw relationship. A facemask is thought to be an effective treatment approach for skeletal Class III patients with maxillary deficiency.The results of previous clinical studies have indicated that the application of an orthopedic force with a protraction facemask to the craniofacial complex during the early phase of growth can contribute to the treatment of Class III malocclusion. The principle of maxillary protraction is to apply an anteriorly directed force on the circummaxillary sutures, which are still patent at an early age and thereby stimulate bone apposition in the suture areas.
A tooth-borne device bonded to the maxillary teeth is the point of force application, and the forehead and the chin are the anchorage sources for protraction in facemask theapy. The effects of maxillary protraction include anterior movement of the maxilla and the maxillary dentition, accompanied by counterclockwise rotation, lingual inclination of the mandibular teeth, and clockwise rotation of the mandible, causing the chin to move downward and backward. Lower anterior facial height increases while overbite decreases. These effects tend to turn a Class III malocclusion into a Class I malocclusion and produce an orthognathic profile in a short time. However, indirect application of force limits the potential for orthopedic change and inevitably causes undesirable tooth movements such as mesial movement and extrusion of the maxillary molars and labial tipping of the maxillary incisors.
There is a need for a stable anchorage to transfer the force directly to the circummaxillary sutures, thus eliminating the undesirable dental effects and obtaining major skeletal effects. Orthopedic anchorage for maxillary protraction is a new area of research, and investigations on this subject are limited. Ankylosed tooth, osseointegrated implants, titanium screws, and onplants have been used as stable anchorage in previous case reports. Titanium miniplates have been shown to provide absolute anchorage when orthopedic forces were applied with facemasks in some clinical studies.
To date, however, there is a lack of knowledge on the comparative effects of maxillary protraction with or without skeletal anchorage. Since there is no study in the literature, in this prospective study, we attempted to evaluate the skeletal, dentoalveolar, and soft-tissue effects of maxillary protraction with miniplates compared with conventional facemask therapy and an untreated Class III control group.
Material and methods
Forty-five subjects from the Department of Orthodontics, Faculty of Dentistry, University of Başkent in Ankara, Turkey, were included in this study. All subjects were between the PP2 = and MP3cap developmental stages at the beginning of the treatment or the control period according to their hand-wrist radiographs. The patients were selected by the following inclusion criteria: (1) skeletal and dental Class III malocclusion with maxillary deficiency (ANB, <0°; Nperp-A, <1 mm; Wits apprasial, <–2 mm); (2) vertically normal growth pattern (SNGoGn, <40°); (3) anterior crossbite and Angle Class III molar relationship; and (4) normal or increased overbite and retrusive nasomaxillary complex. All subjects and parents were informed of the experimental protocols and signed an informed consent form that was previously approved by the ethics committee of the University of Başkent. The selected patients were divided into 3 groups of 15 patients each.
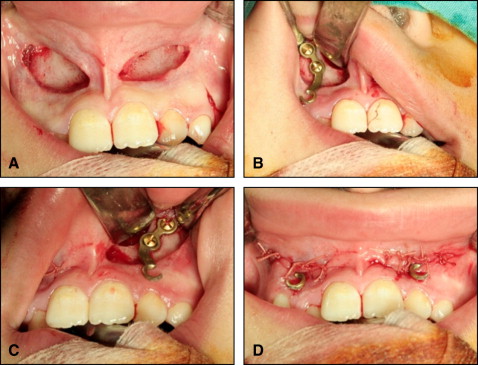
In the first group (MP+FM) consisting of 5 girls and 10 boys (mean age, 10.91 years), facemasks were applied from 2 titanium miniplates (OsteoMed, Addison, Tex) surgically placed laterally to the apertura piriformis regions of the maxilla. Subjects without anchorage teeth for the application of facemask, depending on congenitalIy missing teeth or early removal of posterior deciduous teeth, were given priority for inclusion in this group. I-shaped titanium miniplates, used for fixation in maxillofacial surgery, with 3 holes were placed by the same maxillofacial surgeon (S.U.) under local or general anesthesia. A mucoperiosteal incision was made at the labial vestibule between the maxillary lateral incisors and canines, and a mucoperiosteal flap was elevated to expose the lateral nasal wall of the maxilla on both sides. An appropriate cortical bone area was found to adapt the miniplates around the apertura piriformis, and special care was taken not to damage the erupting canines. Miniplates were then shaped according to the anatomic structures and fixed in position with 2 monocortical miniscrews (diameter, 1.5 mm; length, 7 mm). The incisions were sutured with 3.0 polyglactin 910 exposing the third hole into the oral cavity ( Fig 1 ). After a 1-week period to allow soft-tissue healing, protraction forces were applied with elastics from the hooks of the miniplates to the facemasks ( Fig 2 ).

The second group (FM) of 7 girls and 8 boys (mean age, 10.31 years) received maxillary protraction therapy with conventional facemasks applied from the hooks of the rapid maxillary expansion (RME) appliance.
To distinguish the treatment changes from normal growth changes, the third group of 8 girls and 7 boys (mean age, 10.05 years) was the untreated Class III control group. The subjects of the control group matched those in the treatment groups with regard to chronologic age, skeletal development, and craniofacial morphology.
Before maxillary protraction, a bonded RME appliance with hooks was applied in both treatment groups. The midline expansion screw (1114/10, Lewa, Remchingen, Germany) of the RME appliance was activated twice per day for 7 days until the midpalatal suture was disturbed, and expansion was continued with a semirapid protocol (RME of 7 days, followed by slow maxillary expansion) in patients with continuing maxillary transverse deficiency until the desired expansion was achieved. Immediately after the maxillary sutural system was disrupted, the patients were given Petit-type facemasks (716-0001, Ormco, Glendora, Calif). The facemask protocol was the same for both treatment groups. Elastics, directed 20° to 30° downward from the occlusal plane, delivered a force of 400 g per side, as determined by a force gauge. The patients were instructed to wear their facemasks at least 16 hours per day, and facemask therapy was continued until at least a 4-mm overjet was achieved. Later, all patients had retention treatment with facemasks or chincaps, and some were treated with fixed appliances subsequently.
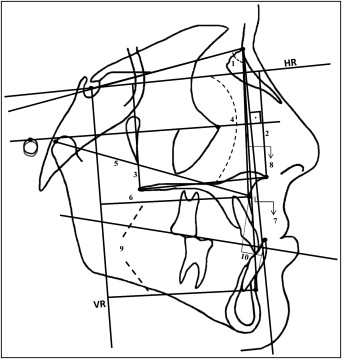
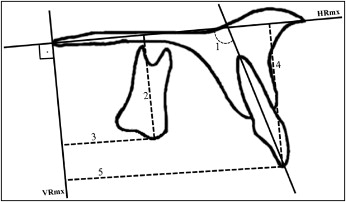
Lateral cephalometric films were obtained at the start of the maxillary protraction or the observation period (T1) and at the end of the active treatment or the observation period (T2) in all groups and were hand-traced on orthodontic tracing paper on a conventional light box by using a 0.3-mm lead pencil and measured by the same investigator (Ç.Ş.) under optimal conditions. For the evaluation of the lateral cephalometric radiographs, in addition to the conventional reference planes, horizontal (HR) and vertical (VR) reference planes were constructed for some linear and angular measurements. A horizontal line constructed by subtracting 7° from the sella-nasion line was used as the HR plane. A vertical line passing through sella and perpendicular to the HR plane was the VR plane ( Figs 3-5 ). The lateral cephalometric radiographs taken at T2 were superimposed on those taken at T1, on stable cranial structures, by using the total structural superimpositioning method. These reference structures were the contours of the anterior wall of sella turcica, the anterior contours of the median cranial fossa, the intersection of the anterior contour of sella and tuberculum sella, the inner surface of the frontal bone, the contours of the cribriform plate, the contours of the bilateral fronto-ethmoidal crests, and the contour of the median border of the cerebral surfaces of the orbital roofs. The HR and VR planes were transferred from the T1 to the T2 radiographs. The sensitivity values of the linear and angular radiographic measurements were 0.5 mm and 0.5°, respectively.
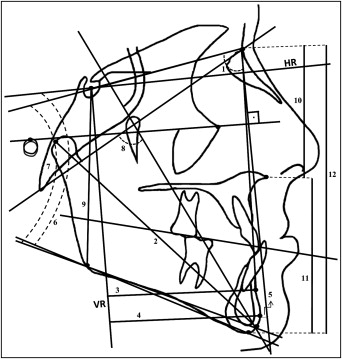
Maxillary regional superimpositions were used to measure the movement of the maxillary dentition relative to the maxillary basal bone. The maxillae were superimposed on the best fit of the lingual curvature of the palatal plate and internal bony structures. To examine the changes in the maxillary dentoalveolar structures, a maxillary HR line (HRmx) was drawn along the ANS-PNS line, and a vertical line passing through PNS and perpendicular to the HRmx was the maxillary VR plane (VRmx) ( Fig 6 ).
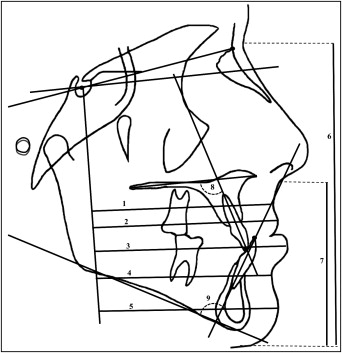
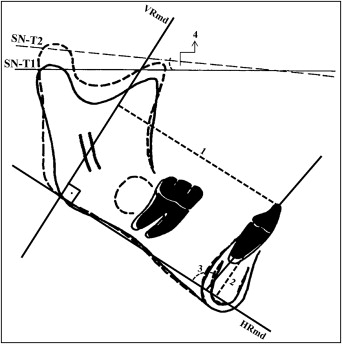
Mandibular regional superimpositions were made on mandibular stable structures, according to the method described by Björk and Skieller. The 2 radiographs were superimposed on the anterior contour of the chin, the inner contour of the cortical plate at the lower border of the symphysis, the trabecular structures inside the symphysis, the contour of the mandibular canal, and the lower contour of a mineralized molar germ before root development begins. To evaluate the changes, a line passing through gonion and gnathion was used as the mandibular HR plane (HRmp), and a vertical line passing through gonion, perpendicular to the HRmp served as the mandibular VR plane (VRmp). The degree of mandibular rotation was assessed by measuring the angle between the sella-nasion lines of the first and second radiographs on the superimposed tracings ( Fig 7 ).
Cephalometric landmarks, reference planes and lines, and measurements are shown in Figures 3 through 7 .
Statistical analysis
Statistical analysis was performed by using the Statistical Package for Social Sciences (version 13.0, SPSS, Chicago, Ill). The normality of the distribution of the variables was checked by using the Shapiro-Wilks test and the homogeneities of the group variances by the Levene test. Since variables were not normally distributed and some groups’ variances were not homogeneous, the Wilcoxon test was used to analyze the changes during the treatment or control periods, and the groups in each period were compared with the Kruskal-Wallis 1-way analysis of variance (ANOVA) by ranks test, and then multiple comparisons between pairs of groups were carried out according to the Dunn test. The results were expressed as means and standard deviations, medians, and minimum and maximum values. P <0.05 was considered to be statistically significant.
Three weeks after the first measurements, the tracings and the measurements were repeated by the same author on 30 lateral cephalograms of 15 randomly selected patients. To assess the reliability of the measurements, the intraclass correlation coefficients (r) were calculated for each variable in the T1 and T2 cephalograms. The intraclass correlation coefficients ranged from 0.989 to 1.000. No significant differences were found between the first and second measurements of those randomly selected cephalograms.
Results
Mobility was noted in 8 of the 30 miniplates at T2; however, only 2 were replaced with additional surgeries during the protraction therapy. The other 6 miniplates showed minimal mobility and were rigid enough to withstand the protraction forces, so they were used until the end of the treatment. Since 2 of the 30 miniplates needed to be replaced, the success rate was 93%.
Table I gives initial values of the 3 groups. There were no significant differences between the groups at T1. The differences between the changes through T2 to T1 in the MP+FM, FM, and control groups are shown in Table II .
| MP + FM | FM | Control | ||
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | ||
| Parameter | Median (range) | Median (range) | Median (range) | P |
| Chronologic age (y) | 10.91 ± 1.22 | 10.31 ± 1.52 | 10.05 ± 1.14 | NS |
| 11.30 (9.00-12.30) | 10.50 (8.50-13.10) | 10.08 (8.50-12.08) | ||
| Maxillary skeletal parameters | ||||
| SNA (°) | 77.86 ± 3.14 | 77.86 ± 2.72 | 78.63 ± 2.43 | NS |
| 77.50 (73.00-82.50) | 79.00 (71.50-81.00) | 78.50 (75.00-82.50) | ||
| A-VR (mm) | 60.60 ± 3.19 | 60.40 ± 3.60 | 60.83 ± 2.49 | NS |
| 60.50 (55.00-66.50) | 59.50 (52.00-66.00) | 60.50 (57.00-65.00) | ||
| Cd-A (mm) | 80.80 ± 3.86 | 79.50 ± 3.87 | 78.90 ± 4.12 | NS |
| 80.50 (72.50-87.50) | 80.00 (72.50-86.50) | 78.00 (70.50-84.00) | ||
| NPerp-A (mm) | −4.36 ± 3.44 | −4.53 ± 2.92 | −3.56 ± 2.27 | NS |
| −4.50 (−11-1.50) | −5.00 (−10-0.50) | −3.50 (−7.00-0) | ||
| HR-ANS (mm) | 43.13 ± 3.57 | 41.36 ± 2.53 | 41.80 ± 2.92 | NS |
| 42.00 (38.50-50.50) | 42.00 (37.00-45.00) | 42.00 (36.00-46.00) | ||
| HR-PNS (mm) | 41.90 ± 3.31 | 40.43 ± 2.28 | 40.90 ± 2.29 | NS |
| 41.50 (36.00-49.00) | 40.00 (37.00-45.00) | 40.00 (38.50-45.50) | ||
| HR.PP (°) | −1.53 ± 4.18 | −1.13 ± 3.55 | −1.03 ± 2.68 | NS |
| −2.00 (−10.00-6.50) | −1.00 (−6.00-8.00) | −2.00 (−4.00-5.00) | ||
| Mandibular skeletal parameters | ||||
| SNB (°) | 81.13 ± 3.45 | 81.26 ± 2.36 | 82.14 ± 2.78 | NS |
| 80.50 (75.50-87.50) | 82.00 (75.50-85.00) | 82.00 (78.00-87.50) | ||
| B-VR (mm) | 62.93 ± 5.39 | 62.50 ± 4.48 | 63.86 ± 4.18 | NS |
| 63.00 (52.00-72.00) | 63.50 (49.50-67.00) | 63.00 (57.00-71.50) | ||
| Cd-Gn (mm) | 111.96 ± 5.64 | 107.76 ± 5.30 | 108.30 ± 6.30 | NS |
| 114.00 (100.0-120.0) | 108.00 (101.0-116.5) | 107.50 (99.0-118.0) | ||
| NPerp-Pg (mm) | 0.53 ± 6.50 | −1.90 ± 3.48 | 0.63 ± 5.09 | NS |
| 1.50 (−17.00-11.00) | −2.00 (−7.50-3.00) | 0.50 (−12.50-8.00) | ||
| Pg-VR (mm) | 63.90 ± 6.21 | 63.23 ± 5.59 | 64.30 ± 4.88 | NS |
| 63.00 (53.50-74.00) | 65.00 (48.00-69.50) | 65.00 (56.50-72.00) | ||
| SN.GoGn (°) | 31.33 ± 4.78 | 30.63 ± 4.98 | 31.23 ± 4.59 | NS |
| 32.00 (22.00-38.00) | 30.00 (23.00-38.00) | 31.00 (24.50-38.50) | ||
| HR.GoMe (°) | 26.80 ± 4.68 | 26.00 ± 4.98 | 26.46 ± 4.73 | NS |
| 28.00 (18.00-34.00) | 26.00 (18.00-33.00) | 26.00 (19.00-34.00) | ||
| BaNa.PtGn (°) | 91.33 ± 4.17 | 91.86 ± 4.84 | 91.40 ± 4.26 | NS |
| 91.50 (84.00-99.00) | 92.00 (83.00-101.5) | 93.00 (81.50-96.00) | ||
| Facial heights | ||||
| S-Go (mm) | 71.36 ± 4.84 | 69.53 ± 4.03 | 68.96 ± 3.35 | NS |
| 72.00 (64.00-80.00) | 70.00 (62.50-76.50) | 69.00 (63.00-74.50) | ||
| N-Me (mm) | 111.03 ± 6.64 | 108.50 ± 6.10 | 108.83 ± 5.96 | NS |
| 111.00 (100.0-122.5) | 108.00 (100.0-118.5) | 110.00 (99.0-117.0) | ||
| ANS-Me (mm) | 59.83 ± 4.55 | 58.63 ± 4.20 | 58.66 ± 4.02 | NS |
| 61.00 (52.00-69.00) | 58.00 (52.00-65.00) | 60.00 (53.00-67.00) | ||
| N-ANS (mm) | 51.20 ± 3.64 | 49.86 ± 2.91 | 50.16 ± 3.06 | NS |
| 50.00 (46.50-59.50) | 50.50 (45.00-54.00) | 50.50 (44.00-54.00) | ||
| S-Go/N-Me | 0.63 ± 0.03 | 0.63 ± 0.04 | 0.63 ± 0.03 | NS |
| 0.63 (0.56-0.71) | 0.63 (0.54-0.70) | 0.62 (0.56-0.70) | ||
| Maxillomandibular parameters | ||||
| ANB (°) | −3.26 ± 2.17 | −3.40 ± 2.35 | −3.51 ± 2.05 | NS |
| −3.5 (−8.00- −1.00) | −2.50 (−8.00-0.00) | −3.50 (−7.00- −0.50) | ||
| (A-VR)-(B-VR) (mm) | −2.33 ± 3.20 | −2.10 ± 3.02 | −3.03 ± 3.33 | NS |
| −1.50 (7.00-3.00) | −1.50 (−6.50-2.50) | −3.50 (−7.50-2.00) | ||
| Wits (mm) | −8.50 ± 3.25 | −7.36 ± 2.08 | −8.83 ± 3.09 | NS |
| −9.00 (−13.00- −3.00) | −8.00 (−10.00- −2.50) | −8.00 (−16.50- −5.50) | ||
| Dentoalveolar parameters | ||||
| Overjet (mm) | −3.06 ± 1.42 | −3.63 ± 0.89 | −3.63 ± 1.80 | NS |
| −3.50 (−6.00- −1.00) | −3.50 (−5.00- −2.50) | −3.00 (−9.00- −2.00) | ||
| Overbite (mm) | 2.73 ± 1.70 | 3.93 ± 1.88 | 3.06 ± 1.82 | NS |
| 2.50 (0.00-5.50) | 4.00 (0.50-7.00) | 3.00 (0.00-7.00) | ||
| U1i-VRmx (mm) | 43.80 ± 3.08 | 41.66 ± 3.81 | 43.73 ± 5.21 | NS |
| 42.50 (40.00-51.00) | 41.00 (34.50-50.00) | 44.50 (31.00-51.00) | ||
| U1i-HRmx (mm) | 25.50 ± 2.73 | 25.70 ± 2.08 | 24.63 ± 3.07 | NS |
| 25.50 (20.00-31.00) | 25.00 (23.00-29.50) | 25.00 (17.50-29.00) | ||
| U1.HRmx (°) | 114.60 ± 5.87 | 110.83 ± 6.44 | 113.20 ± 7.13 | NS |
| 115.00 (105.0-126.0) | 110.00 (102.0-126.0) | 112.00 (102.50-128) | ||
| U1.PP (°) | 113.70 ± 6.32 | 110.36 ± 6.01 | 114.23 ± 8.33 | NS |
| 114.00 (104.0-125.0) | 110.00 (102.0-124.5) | 112.00 (101.0-128.0) | ||
| L1i-VRmd (mm) | 62.16 ± 3.98 | 61.73 ± 3.46 | 62.50 ± 4.40 | NS |
| 62.00 (54.50-68.50) | 62.00 (53.00-67.00) | 63.50 (54.00-68.50) | ||
| L1.HR (°) | 87.63 ± 6.48 | 88.03 ± 7.32 | 87.66 ± 8.26 | NS |
| 87.00 (76.00-101.00) | 87.00 (78.00-103.50) | 87.50 (73.00-100.00) | ||
| L1.MP (°) | 84.96 ± 6.97 | 85.43 ± 8.50 | 84.93 ± 7.58 | NS |
| 85.00 (72.00-100.00) | 82.50 (74.00-103.50) | 85.00 (73.00-97.00) | ||
| U6-VRmx (mm) | 16.80 ± 4.40 | 14.70 ± 2.78 | 17.40 ± 3.23 | NS |
| 16.50 (11.00-24.50) | 14.00 (10.50-20.00) | 18.50 (10.00-22.00) | ||
| U6-HRmx (mm) | 18.46 ± 3.73 | 19.50 ± 2.29 | 18.83 ± 2.15 | NS |
| 18.00 (11.00-23.00) | 19.00 (16.00-24.00) | 18.50 (15.50-23.00) | ||
| Soft-tissue parameters | ||||
| N′-Me′ (mm) | 118.46 ± 7.50 | 115.40 ± 5.73 | 116.80 ± 6.80 | NS |
| 119.00 (108.0-132.0) | 114.00 (106.0-127.0) | 116.00 (106.5-132.0) | ||
| Sn-Me′ (mm) | 63.46 ± 5.65 | 61.86 ± 3.58 | 63.00 ± 4.75 | NS |
| 64.00 (54.00-74.00) | 61.00 (55.00-68.00) | 63.00 (56.50-74.00) | ||
| A′-VR (mm) | 75.93 ± 3.90 | 75.26 ± 3.46 | 76.06 ± 3.05 | NS |
| 77.00 (67.50-82.00) | 74.50 (66.50-81.00) | 74.50 (72.00-81.00) | ||
| B′-VR (mm) | 73.70 ± 5.74 | 72.66 ± 5.05 | 74.86 ± 4.47 | NS |
| 73.00 (62.50-82.50) | 74.00 (58.00-78.50) | 73.50 (68.00-82.50) | ||
| UL-VR (mm) | 78.60 ± 4.87 | 77.90 ± 3.89 | 78.93 ± 3.76 | NS |
| 78.50 (69.00-86.00) | 78.00 (69.00-83.50) | 78.50 (73.00-85.00) | ||
| LL-VR (mm) | 80.20 ± 5.57 | 79.56 ± 4.47 | 80.90 ± 4.13 | NS |
| 80.00 (69.50-90.00) | 80.00 (68.00-84.50) | 80.50 (74.50-87.50) | ||
| Pg′-VR (mm) | 75.66 ± 6.62 | 74.76 ± 6.42 | 76.76 ± 5.58 | NS |
| 75.00 (64.00-85.50) | 76.50 (57.50-82.00) | 79.00 (67.00-83.50) | ||
| MP + FM (1) | FM (2) | Control (3) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | ||||||||
| Parameter | Median (range) | P | Median (range) | P | Median (range) | P | H | 1-2 | 2-3 | 1-3 |
| Treatment duration(y) | 0.56 ± 0.16 | ‡ | 0.78 ± 0.26 | ‡ | 0.63 ± 0.10 | ‡ | ||||
| 0.50 (0.30-0.80) | 0.80 (0.40-1.30) | 0.60 (0.50-0.80) | ||||||||
| Protraction rate(mm/mo) | 0.45 ± 0.20 | 0.24 ± 0.18 | 0.05 ± 0.08 | ‡ | ‡ | ‡ | ||||
| 0.41 (0.17-0.83) | 0.20 (0.00-0.62) | 0.05 (−0.08-0.27) | ||||||||
| Maxillary skeletal parameters | ||||||||||
| SNA (°) | 2.53 ± 1.24 | † | 1.83 ± 1.33 | † | 0.26 ± 0.53 | NS | ‡ | ‡ | ‡ | |
| 2.00 (1.00-5.50) | 2.00 (0.00-4.00) | 0.00 (−1.00-1.00) | ||||||||
| A-VR (mm) | 2.83 ± 0.93 | † | 2.16 ± 1.38 | † | 0.44 ± 0.69 | ∗ | ‡ | ‡ | ‡ | |
| 3.00 (1.50-5.00) | 2.00 (0.00-5.00) | 0.50 (−0.50-2.00) | ||||||||
| Cd-A (mm) | 3.26 ± 1.82 | † | 1.80 ± 1.70 | † | 0.80 ± 0.95 | † | ‡ | ‡ | ‡ | |
| 3.00 (1.00-8.50) | 1.50 (−1.50-6.00) | 1.00 (−0.50-3.50) | ||||||||
| NPerp-A (mm) | 2.53 ± 1.31 | † | 1.76 ± 1.36 | † | 0.30 ± 0.59 | NS | ‡ | ‡ | ‡ | |
| 2.00 (0.50-4.50) | 1.50 (0.00-4.00) | 0.00 (−1.00-1.50) | ||||||||
| HR-ANS (mm) | 0.66 ± 1.24 | ∗ | 1.00 ± 0.98 | † | 0.94 ± 0.91 | † | NS | |||
| 0.50 (−1.00-4.00) | 1.00 (−1.50-2.00) | 0.50 (−0.50-2.50) | ||||||||
| HR-PNS (mm) | 1.50 ± 0.65 | † | 2.24 ± 1.19 | † | 0.80 ± 0.84 | † | ‡ | ‡ | ‡ | |
| 1.50 (0.50-3.00) | 2.00 (0.00-4.00) | 0.50 (0.00-2.50) | ||||||||
| HR.PP (°) | 0.91 ± 1.82 | NS | 1.63 ± 1.51 | † | −0.20 ± 1.19 | NS | ‡ | ‡ | ‡ | |
| 1.00 (−3.00-4.00) | 1.00 (−1.00-5.00) | 0.00 (−2.50-1.50) | ||||||||
| Mandibular skeletal parameters | ||||||||||
| SNB (°) | −1.93 ± 2.19 | ∗ | −2.30 ± 1.23 | † | 0.65 ± 0.65 | † | ∗ | ‡ | ‡ | |
| −2.50 (−5.00-2.50) | −2.50 (−4.00-0.50) | 0.50 (0.00-2.00) | ||||||||
| B-VR (mm) | −2.76 ± 2.01 | † | −3.03 ± 1.92 | † | 1.23 ± 1.27 | † | NS | ‡ | ‡ | |
| −2.50 (−5.50-0.50) | −3.50 (−6.00-1.00) | 1.50 (−1.00-3.50) | ||||||||
| Cd-Gn (mm) | −0.30 ± 2.15 | NS | 0.43 ± 2.15 | NS | 1.86 ± 1.12 | † | † | ‡ | ‡ | |
| 0.00 (−5.00-3.00) | 0.50 (−3.00-4.00) | 2.00 (0.50-4.50) | ||||||||
| NPerp-Pg (mm) | −2.80 ± 2.67 | † | −2.90 ± 3.97 | ∗ | 0.96 ± 1.66 | ∗ | NS | ‡ | ‡ | |
| −3.00 (−7.00-2.50) | −2.50 (−9.00-4.00) | 0.50 (−2.00-5.00) | ||||||||
| Pg-VR (mm) | −2.53 ± 2.10 | † | −3.36 ± 2.51 | † | 1.93 ± 1.32 | † | † | ‡ | ‡ | |
| −2.50 (−6.00-2.00) | −3.50 (−7.00-1.00) | 2.00 (0.00-4.50) | ||||||||
| SN.GoGn (°) | 1.46 ± 2.78 | ∗ | 3.06 ± 2.07 | † | −0.40 ± 0.87 | NS | ‡ | ‡ | ‡ | |
| 2.00 (−6.00-4.50) | 3.00 (−1.00-6.00) | 0.00 (−2.00-1.00) | ||||||||
| HR.GoMe (°) | 1.86 ± 2.10 | † | 2.76 ± 1.98 | † | −0.03 ± 0.83 | NS | † | ‡ | ‡ | |
| 2.50 (−3.00-5.00) | 2.50 (0.00-7.50) | 0.00 (−1.00-2.00) | ||||||||
| BaNa.PtGn (°) | −1.90 ± 2.14 | ∗ | −3.13 ± 2.48 | † | 0.53 ± 0.81 | ∗ | † | ‡ | ‡ | |
| −2.50 (−4.00-5.00) | −3.00 (−7.00-2.00) | 0.00 (0.00-2.50) | ||||||||
| Mandibular rotation (°) | 1.83 ± 2.19 | 2.80 ± 2.23 | −0.20 ± 1.42 | † | ‡ | ‡ | ||||
| 3.00 (−4.00-4.00) | 3.00 (−3.00-6.00) | 0.00 (−3.00-2.00) | ||||||||
| Facial heights | ||||||||||
| S-Go (mm) | 0.36 ± 1.26 | NS | 1.23 ± 1.98 | ∗ | 1.06 ± 1.29 | † | NS | |||
| 0.00 (−1.50-3.00) | 1.00 (−2.00-6.00) | 1.00 (−1.00-3.50) | ||||||||
| N-Me (mm) | 2.73 ± 2.76 | ∗ | 4.63 ± 1.96 | † | 0.83 ± 1.01 | ∗ | ‡ | ‡ | ‡ | |
| 3.50 (−5.50-5.00) | 4.00 (2.00-9.00) | 1.00 (−1.50-3.00) | ||||||||
| ANS-Me (mm) | 2.10 ± 1.79 | † | 3.96 ± 1.74 | † | 0.10 ± 0.91 | NS | ‡ | ‡ | ‡ | |
| 2.00 (−2.00-5.00) | 4.00 (0.50-7.00) | 0.00 (−2.00-1.50) | ||||||||
| N-ANS (mm) | 0.56 ± 2.29 | NS | 0.70 ± 1.29 | NS | 0.76 ± 0.86 | † | NS | |||
| 1.00 (−3.50-4.00) | 0.50 (−1.00-3.00) | 0.50 (−0.50-2.50) | ||||||||
| S-Go/N-Me | −0.01 ± 0.02 | ∗ | −0.01 ± 0.01 | † | 0.00 ± 0.01 | NS | NS | ‡ | ‡ | |
| −0.02 (−0.05-0.03) | −0.01 (−0.04-0.01) | −0.01 (−0.05-0.03) | ||||||||
| Maxillomandibular parameters | ||||||||||
| ANB (°) | 4.46 ± 1.95 | † | 4.20 ± 1.96 | † | −0.38 ± 0.71 | NS | NS | ‡ | ‡ | |
| 4.00 (1.00-9.00) | 5.00 (0.00-7.50) | −0.30 (−1.50-0.50) | ||||||||
| (A-VR)-(B-VR) (mm) | 5.66 ± 2.24 | † | 5.06 ± 2.16 | † | −0.78 ± 1.22 | ∗ | NS | ‡ | ‡ | |
| 5.50 (1.50-10.00) | 5.00 (0.50-8.50) | −0.50 (−3.50-1.20) | ||||||||
| Wits (mm) | 5.43 ± 1.69 | † | 6.56 ± 2.88 | † | −0.53 ± 1.14 | NS | † | ‡ | ‡ | |
| 5.00 (3.00-9.00) | 7.00 (1.00-11.50) | −0.50 (−2.00-1.50) | ||||||||
| Dentoalveolar parameters | ||||||||||
| Overjet (mm) | 7.66 ± 1.61 | † | 7.93 ± 1.65 | † | −0.33 ± 0.72 | NS | NS | ‡ | ‡ | |
| 8.00 (4.00-10.00) | 7.50 (5.00-11.50) | −0.50 (−2.00-1.00) | ||||||||
| Overbite (mm) | 0.33 ± 2.17 | NS | −0.90 ± 1.64 | NS | 0.26 ± 0.62 | NS | NS | |||
| −0.50 (−2.00-5.50) | −0.50 (−5.00-1.50) | 0.00 (−1.00-1.50) | ||||||||
| U1i-VRmx (mm) | −0.30 ± 1.37 | NS | 1.86 ± 1.32 | † | 0.53 ± 0.85 | ∗ | ‡ | ‡ | ‡ | |
| 0.00 (−4.00-1.00) | −2.00 (−1.00-4.00) | 0.00 (0.00-2.50) | ||||||||
| U1i-HRmx (mm) | 0.66 ± 0.97 | ∗ | 0.43 ± 0.86 | NS | 0.33 ± 0.44 | ∗ | NS | |||
| 0.50 (−1.00-2.50) | 0.50 (−1.00-2.00) | 0.00 (0.00-1.50) | ||||||||
| U1.HRmx (°) | −2.36 ± 3.54 | ∗ | 2.73 ± 4.46 | ∗ | 0.90 ± 1.15 | † | ‡ | † | ‡ | |
| −1.50 (−10.00-2.00) | 2.00 (−6.00-11.00) | 0.50 (0.00-3.00) | ||||||||
| U1.PP (°) | −0.83 ± 3.95 | NS | 2.36 ± 3.14 | ∗ | 0.80 ± 1.85 | NS | ‡ | ‡ | ∗ | |
| 1.00 (-12.00-4.00) | 3.00 (−3.50-8.00) | 0.00 (−3.50-4.00) | ||||||||
| L1i-VRmd (mm) | −3.93 ± 2.59 | † | −2.96 ± 1.45 | † | −0.13 ± 0.63 | NS | ∗ | ‡ | ‡ | |
| −3.50 (−10.00- −1.00) | −3.00 (−6.00- −1.00) | 0.00 (−1.50-1.50) | ||||||||
| L1.HRmd (°) | −7.16 ± 3.12 | † | −7.06 ± 3.86 | † | −0.43 ± 1.51 | NS | NS | ‡ | ‡ | |
| −7.00 (−13.00-0.00) | −7.50 (−13.00-2.00) | 0.00 (−4.00-3.50) | ||||||||
| L1.MP (°) | −7.83 ± 3.51 | † | −5.40 ± 4.03 | † | −0.83 ± 1.43 | NS | ‡ | ‡ | ‡ | |
| −7.00 (−14.00- −2.00) | −4.50 (−16.50-2.00) | −0.50 (−3.50-1.00) | ||||||||
| U6-VRmx (mm) | −0.03 ± 0.63 | NS | 1.93 ± 2.35 | ∗ | −0.20 ± 0.64 | NS | ‡ | ‡ | NS | |
| 0.00 (−1.50-1.00) | 2.50 (−4.00-5.00) | 0.00 (−2.50-0.00) | ||||||||
| U6-HRmx (mm) | 0.16 ± 0.67 | NS | 0.60 ± 1.12 | ∗ | 0.00 ± 0.00 | NS | NS | |||
| 0.00 (−1.00-1.50) | 0.50 (−1.00-4.00) | 0.00 (0.00-0.00) | ||||||||
| Soft-tissue parameters | ||||||||||
| N′-Me′ (mm) | 1.66 ± 3.79 | NS | 3.86 ± 2.59 | † | 0.46 ± 1.39 | NS | ‡ | ‡ | ‡ | |
| 2.00 (−6.00-8.00) | 4.00 (0.00-10.00) | 0.00 (−2.00-4.00) | ||||||||
| Sn-Me′ (mm) | 2.43 ± 2.08 | † | 3.86 ± 2.23 | † | 0.30 ± 1.46 | NS | ‡ | ‡ | ‡ | |
| 2.00 (−3.00-5.00) | 4.00 (0.00-9.00) | 0.00 (−2.00-3.00) | ||||||||
| A′-VR (mm) | 3.36 ± 1.20 | † | 2.66 ± 2.17 | † | 0.90 ± 0.91 | † | ‡ | ‡ | ‡ | |
| 3.50 (1.00-5.50) | 2.00 (0.00-6.50) | 1.00 (−1.00-2.50) | ||||||||
| B′-VR (mm) | −2.86 ± 1.88 | † | −2.90 ± 3.29 | † | 1.66 ± 1.35 | † | NS | ‡ | ‡ | |
| −2.50 (−6.00-0.00) | −2.50 (−13.00-0.50) | 2.00 (−0.50-4.00) | ||||||||
| UL-VR (mm) | 3.43 ± 1.76 | † | 2.63 ± 2.74 | † | 0.83 ± 1.09 | ∗ | ‡ | ‡ | ‡ | |
| 3.00 (1.00-7.00) | 2.00 (−2.00-7.00) | 1.00 (−1.00-3.00) | ||||||||
| LL-VR (mm) | −1.33 ± 2.12 | ∗ | −1.16 ± 2.41 | NS | 1.60 ± 1.05 | † | NS | ‡ | ‡ | |
| −1.00 (−5.50-2.00) | −1.00 (−5.00-3.50) | 2.00 (0.00-3.50) | ||||||||
| Pg′-VR (mm) | −2.66 ± 2.34 | † | −2.53 ± 2.23 | † | 1.76 ± 1.37 | † | NS | ‡ | ‡ | |
| −2.00 (−6.00-0.50) | −3.00 (−6.50-1.00) | 2.00 (−0.50-4.00) | ||||||||
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


