Worldwide incidences of degenerative cognitive diseases are increasing as the population ages. This decline in mental function frequently causes behavioral changes that directly affect oral health. The loss of interest and ability to complete the simple tasks of brushing and flossing can cause a rapid development of hard and soft tissue diseases that result in decreased function and increased dental pain. The challenge for the dental community is to understand and to identify the early signs of cognitive dysfunction so as to develop a rational treatment strategy that allows patients to comfortably maintain their teeth for as long as possible.
Key points
- •
Worldwide incidences of degenerative cognitive diseases are increasing as the population ages. This decline in mental function frequently causes behavioral changes that directly affect oral health.
- •
The loss of interest and ability to complete the simple tasks of brushing and flossing can cause a rapid development of hard and soft tissue diseases that result in decreased function and increased dental pain.
- •
The challenge for the dental community is to understand and to identify the early signs of cognitive dysfunction so as to develop a rational treatment strategy that allows patients to comfortably maintain their teeth for as long as possible.
Introduction
Cognitive impairment is a disease or condition that presents in individuals causing them to have trouble remembering, learning new things, concentrating, or making decisions that affect their everyday life. The prevalence of cognitive dysfunction increases as seniors live into their 80s and 90s. The US Census Bureau estimated that the 2013 population of United States was 318,000,000 million people with the older than 65 segment approximately 41 million individuals. The Centers for Disease Control and Prevention (CDC) determined that of this group of 41 million seniors, 16 million suffered a broad spectrum of different cognitive dysfunctions and struggled to perform the basic activities of daily living (ADLs), including the ability to maintain good oral health ( Table 1 ).
| Estimated population of the United States | 318,000,000 |
| Estimated population older than 65 | 41,000,000 |
| Estimated population older than 65 with a cognitive impairment | 16,000,000 |
Cognitive impairment is often first recognized by family and friends when a person begins to struggle with simple daily tasks. Then, as the impairments increase to a more severe level, the problems with reading, writing, and understanding prevent independent living. Fear of “losing one’s mind” and the loss of personal control may be the single greatest worry and concern of the aging and a constant threat for everyone else.
Impairment is often followed by oral health deterioration, characterized by a dramatic and quick progression of periodontal disease, caries, and tooth loss. The process is complicated by the senior’s inability to understand these changes accompanied by a loss of interest in brushing and flossing. The dentist and the dental team are called on to treat these patients in nursing homes and in office situations to maintain the patients’ oral function, diagnose pathology, restore esthetics, and deliver palliative care. These impaired dental patients present to the office with confusion and frustration and unable to understand “why his gums bleed” and “asking why he has cavities.”
This article on cognitive impairment discusses types and causes of cognitive impairments, the demographics of the disease in our aging population, reviews patient management protocols, and stresses the importance of using an interdisciplinary approach to delivering rational patient care.
Introduction
Cognitive impairment is a disease or condition that presents in individuals causing them to have trouble remembering, learning new things, concentrating, or making decisions that affect their everyday life. The prevalence of cognitive dysfunction increases as seniors live into their 80s and 90s. The US Census Bureau estimated that the 2013 population of United States was 318,000,000 million people with the older than 65 segment approximately 41 million individuals. The Centers for Disease Control and Prevention (CDC) determined that of this group of 41 million seniors, 16 million suffered a broad spectrum of different cognitive dysfunctions and struggled to perform the basic activities of daily living (ADLs), including the ability to maintain good oral health ( Table 1 ).
| Estimated population of the United States | 318,000,000 |
| Estimated population older than 65 | 41,000,000 |
| Estimated population older than 65 with a cognitive impairment | 16,000,000 |
Cognitive impairment is often first recognized by family and friends when a person begins to struggle with simple daily tasks. Then, as the impairments increase to a more severe level, the problems with reading, writing, and understanding prevent independent living. Fear of “losing one’s mind” and the loss of personal control may be the single greatest worry and concern of the aging and a constant threat for everyone else.
Impairment is often followed by oral health deterioration, characterized by a dramatic and quick progression of periodontal disease, caries, and tooth loss. The process is complicated by the senior’s inability to understand these changes accompanied by a loss of interest in brushing and flossing. The dentist and the dental team are called on to treat these patients in nursing homes and in office situations to maintain the patients’ oral function, diagnose pathology, restore esthetics, and deliver palliative care. These impaired dental patients present to the office with confusion and frustration and unable to understand “why his gums bleed” and “asking why he has cavities.”
This article on cognitive impairment discusses types and causes of cognitive impairments, the demographics of the disease in our aging population, reviews patient management protocols, and stresses the importance of using an interdisciplinary approach to delivering rational patient care.
Demographics of cognitive impairment
In 2013, more than 70% of seniors older than 65 sought out dental care. Most of these individuals, 70%, have some of their natural teeth compared with 54% of seniors only 20 years ago. They are living in the community and are able to visit the dental office independently. These older patients have successfully participated in a lifetime of prevention and treatment and feel they have “earned” their dentition. Unfortunately, as many of these individuals develop cognitive impairment problems, their motor and cognitive skills greatly diminish, resulting in a rapid progression of oral disease.
In 2008, census information estimated that more than 14.5 million seniors, representing 95% of elders with cognitive impairment, live at home or in an alternate form of a living assistance program. Another 1.4 million (5%) seniors live in nursing facilities. Cognitive impairment is the primary diagnosis for more than 68% of patients in the nursing home with an estimated 27% of the residents with mild dementia and another 41% diagnosed with severe cognitive dementia. It is also estimated that more than 75% of the nursing home population needs daily assistance with all the ADLs, including oral health care. These individuals cannot adequately clean their teeth and often have trouble even remembering how to brush. Older adults with dementia uniformly demonstrate high levels of plaque and calculus, increased rates of caries, increased denture sores, decreased denture use, and decreased salivary gland function. Additionally, any oral problems that are present before admission to the long-term care (LTC) facility tend to exacerbate once the senior is settled into the new living environment.
What is a healthy brain and good cognitive health?
The CDC defines a healthy brain as one that can perform the mental processes that are collectively known as cognition. Examples of cognition are the ability to learn new things, intuition, judgment, language, and remembering. Most people think of cognitive health as staying sharp, being right in the mind, and having good genes. People from different ethnic and racial populations tend to share a core set of beliefs when they convey their thoughts on a healthy brain. Most cultures describe the activities of independent living, driving, having a good memory, and solving puzzles as a sign brain health.
Public health’s awareness in maintaining cognitive health is playing an important role in redefining the concept of healthy aging in today’s world. Scientific studies reinforce ways to minimize risky behaviors that are related to cognitive deterioration; for example, lack of physical activity and uncontrolled high blood pressure. Even with these new lifestyle changes, normal aging, illness, and hospitalization still contribute to the decline in the ability of seniors. If cognitive dysfunction can be prevented and better treated, many older adults will enjoy a life of health and activity.
Basic self-care tasks are known as the ADLs, whereas the more complex tasks that are needed to live independently are described as instrumental ADLs (IADLs). When these tasks are considered together, they help determine whether an older person can live independently ( Box 1 ).
-
Activities of daily living (ADLs) are basic self-care tasks that people usually learn in early childhood.
- •
Feeding
- •
Toileting
- •
Selecting proper attire
- •
Grooming and brushing teeth
- •
Maintaining continence
- •
Putting on clothes and bathing
- •
-
Instrumental activities of daily living (IADLs) are complex skills needed to successfully live independently.
- •
Managing finances
- •
Handling transportation (driving or navigating public transit)
- •
Shopping
- •
Preparing meals
- •
Using the telephone and other communication devices
- •
Managing medications
- •
Housework and basic home maintenance
- •
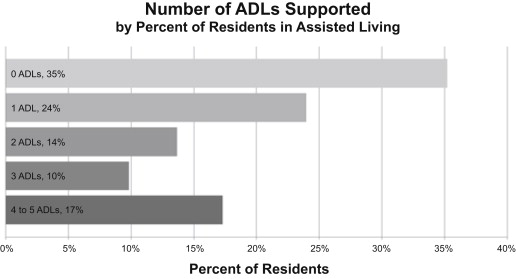
Although more than 75% of residents in assisted living receive support with 1 or more ADL, 25% of the residents do not, according to a 2001 survey of assisted living communities conducted by the National Center for Assisted Living. Most residents need help with oral care.
As patients with impairments progress into LTC, their ability to perform these activities continuously decreases with resulting negative behavioral changes. The prevalence of pain, mouth odor, bleeding tissues, and edentulism all increase. Studies show that the oral care that residents receive in a nursing home is poor because of the lack of staff training, time constraints, and staff turnover. The overall yearly retention rate in 2009 for assisted living employees was 51%. Retention rates among resident caregivers (noncertified), certified nurse assistants, and medication aides ranged from 44% to 55%. By the time the caregivers are trained in the minimal basics of oral care management, many leave the facilities. Additionally, the LTC staffs are frequently asked to help manage the oral care of residents who are uncooperative, combative, and lack the ability to understand why people are invading their personal space. Rarely do these residents receive an adequate cleaning and seldom on a daily basis. Unfortunately, most senior residents rely on caregivers to help maintain their oral health ( Fig. 1 ).
Cognitive impairment in older adults
Reversible Cognitive Impairment
For older adults with cognitive difficulties, especially if this represents an abrupt change in mental status, a medical workup is always indicated to rule out a potential organic cause for this change. It is unlikely that a sudden mental status change represents a conversion to dementia. Particularly in a setting such as a hospital or a nursing home, a sudden mental status change is often the result of a delirium. Elders with delirium are characterized by inattentiveness and a fluctuating mental status. Delirious individuals may develop frightening hallucinations and become quite frightened and agitated. Delirium is most often caused by infections, electrolyte disturbances, dehydration, and medication effects and improves when the offender is treated or removed. Older adults with dementia are more vulnerable to developing delirium, and delirium is a risk factor for Alzheimer disease (AD).
Specific medical etiologies of reversible cognitive impairment may be neurologic or non-neurologic. Neurologic causes of reversible cognitive impairment can include brain lesions (ie, tumors) and normal pressure hydrocephalus, which is caused by the accumulation of cerebrospinal fluid enlarging spaces within the brain. Other medical, non-neurologic causes of reversible cognitive impairment include vitamin deficiencies (most commonly B12 deficiency), thyroid abnormalities, and neurosyphilis. All individuals receiving a workup for a change in their mental status should have vitamin B12, thyroid functioning, and rapid plasma reagin (antibodies to the organism causing syphilis) in addition to routine physical examination and laboratory work to check for these potentially reversible causes of cognitive impairment ( Table 2 ).
| Reversible | Irreversible |
|---|---|
| Drugs | Alzheimer disease |
| Nutritional deficiencies | Multi-infarct |
| Normal-pressure hydrocephalous | Huntington chorea |
| Brain tumors | Pick disease |
| Hypothyroidism, hyperthyroidism | Creutzfeldt-Jakob |
| Neurosyphilis | Kuru |
| Depression | Wernicke-Korsakoff |
Depression is a widespread concern in older adults, many of whom are struggling with numerous losses and life changes. Although many depressive symptoms are similar in older adults and younger adults, such as suicidal thinking, psychomotor retardation, and sleep and appetite difficulties, older adults with depression may also appear to be more withdrawn and cognitively impaired than their nondepressed counterparts. Depression in older adults may be treated with antidepressant medications and/or psychotherapy ( Box 2 ).
- •
Persistent sadness and loss of interest in the pleasures of life
- •
Withdrawal from society
- •
Weight change, insomnia, loss of appetite and energy
- •
Feeling of worthlessness
- •
Thoughts of death or suicide
Mild Cognitive Impairment
What differentiates mild cognitive impairment (MCI) from dementia is that the older adult experiences cognitive difficulties without a significant functional decline or impact on quality of life. Overall prevalence of MCI in the elderly is 15% to 20%, with an increased prevalence depending on age. Individuals with mild cognitive impairment do not need assistance with their ADLs, such as brushing their teeth, eating, or bathing, and at most require minimal assistance with IADLs, such as taking medications, shopping for groceries, or managing finances. MCI can be classified as being amnestic, nonamnestic, or of multiple domains (both amnestic and nonamnestic). Elders with amnestic MCI have particular struggles with memory and are more likely to develop Alzheimer dementia than older adults without cognitive impairment (10%–12% per year vs 1%–2% per year). Older adults with nonamnestic MCI struggle with other cognitive functions, such as executive functioning and aphasia. Nonamnestic MCI does not appear to reliably progress to Alzheimer dementia or other dementias. Elders with multiple-domain MCI are more likely to develop Alzheimer dementia and vascular dementia than cognitively intact peers.
Dementia
Although some of these older adults have reversible etiologies to their significant cognitive impairment, as previously stated, a vast majority of these individuals have irreversible cognitive impairment termed dementia. As noted, cognitive impairment becomes dementia when the elder develops significant functional impairment, requiring significant assistance with ADLs and IADLs. Older adults with dementia are generally unable to brush or floss. Dementia is quite common in older adults and is becoming an epidemic. Approximately 8% of all adults older than 65, 20% of individuals older than 80, and 40% of elders older than 90 have a diagnosis of dementia. Although there are a great many etiologies of dementia, this article focuses on 4 of the most common causes: Alzheimer dementia, vascular dementia (VD), dementia with Lewy bodies (DLB), and frontotemporal dementia (FTD).
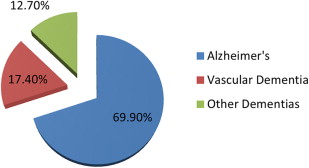
AD is by far the most common cause of dementia, both in the United States and worldwide. The prevalence of AD is approximately 2% in individuals who are 65, with prevalence doubling every 5 years to a prevalence of more than 30% in adults who are 85 and older. There is a clear genetic predisposition to AD in approximately 5% of cases, and these individuals are more likely to develop AD earlier in life. Compared with other types of dementias, AD has an insidious onset, affecting memory, language, spatial relations, attention, and orientation, over the course of years. It is generally not until later on in the illness that personal hygiene is significantly affected.
VD is the second most commonly diagnosed form of dementia in older adults in the United States. Because their cognitive impairment is related to 1 or more cerebrovascular accidents (CVAs), individuals with VD have sensory, motor, and/or gait difficulties in addition to struggles with their memory and other cognitive functions. Cognitive decline is less common in individuals with vascular dementia, occurring only with additional CVAs or the development of comorbid AD ( Fig. 2 ).