Abstract
Autotransplantation is often performed to replace a missing tooth, but tooth autotransplantation has been reported in fewer teeth with complete root formation than those with incomplete root formation. The aim of this prospective study was to evaluate the factors that affect the prognosis of autotransplantation of teeth with complete root formation. 109 patients with 117 transplants were studied. Of the 117 transplants investigated, 14 (12%) failed during the observation period. The overall 1-year survival rate was 96%; the 5-year survival rate was 84%. The major causes of failure were unsuccessful initial healing and replacement root resorption with periodontal inflammation. Factors significantly associated with unsuccessful transplantation, in single factor analysis, were age 40 years or more, molar tooth as donor, probing pocket depth to 4 mm or more, history of root canal treatment, multi-rooted teeth and fixation with sutures. Pocket depth of 4 mm or more and history of root canal treatment appeared to increase the risk of unsuccessful transplantation in multivariate analysis. It is suggested that the pocket depth of the donor tooth and history of root canal treatment are related to the healing of paratransplantal tissue and root resorption.
Tooth autotransplantation is a viable option for replacing a missing tooth because the transplanted tooth can function as a normal tooth when tooth transplantation is successful. The prognosis of an autotransplanted tooth is influenced by pre- and per-operative conditions, which are recognized as prognostic factors. A large number of clinical studies on tooth autotransplantation have been conducted, but most of them reported the transplantation of teeth with incomplete roots and focused on factors such as the developmental and eruption stage of the donor tooth, root development, pulpal healing and root resorption of the transplanted tooth .
The autotransplantation of teeth with complete root formation necessitates endodontic treatment within 3–4 weeks to avoid pulp infection followed by periradicular inflammation and subsequent inflammatory root resorption because revascularization of the pulp is not normally expected after tooth transplantation . The prognostic factors for the autotransplantation of teeth with complete root formation should be investigated differently from those associated with autotransplantation of teeth with incomplete root formation. Recent studies have reported the autotransplantation of teeth with complete root formation , but in only three of these reports was the prognostic value of the pre- and per-operative conditions statistically analyzed . The authors have carried out more than 50 cases of tooth transplantation annually since 1994. In 2001, they began carrying out tooth autotransplantation supported by a multidisciplinary team, consisting of oral surgeons, endodontists, periodontists, prosthodontists and orthodontists, in order to study tooth autotransplantation prospectively. The aim of the present prospective study was to evaluate the prognostic factors for autotransplantation of teeth with complete root formation carried out at the authors’ institution from December 2001 to March 2004.
Materials and methods
109 patients were studied in whom 117 teeth with complete roots were transplanted from December 2001 to March 2004. All patients provided informed consent. The study was approved by the institutional review board of the Dental School at Niigata. The patients were followed up until 31 October 2007.
The patients consisted of 68 females and 41 males, ranging in age from 11 to 75 years (mean age 39.0 years) at the time of surgery. None of the patients had previous or present general conditions that contraindicated surgical treatment in the oral region. The mean duration of the follow-up period for all teeth was 40.9 months, ranging from 12.0 to 71.2 months. Patients who were followed up for less than a year because of transfer or because they lived far away were excluded from this study.
The transplanted donor teeth comprised 90 molars (77%), 26 premolars (22%), and one incisor (1%). Molar positions were transplanted in 89 cases (76%) and premolar positions in 21 cases (18%). In 27 cases (23%), a lower third molar tooth was transplanted to the lower second molar position ( Table 1 ).
| Recipient site | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Molars | Premolars | Incisors | |||||||||||
| Upper first | Lower first | Upper second | Lower second | Lower third | Lower first | Upper second | Lower second | Upper central | Upper lateral | Upper canine | Sum | ||
| Molars | |||||||||||||
| Upper second | 1 | 2 | 1 | 1 | 5 | 90 (76.9%) | |||||||
| Lower second | 2 | 2 | |||||||||||
| Upper third | 4 | 9 | 3 | 12 | 1 | 1 | 5 | 35 | |||||
| Lower third | 1 | 15 | 4 | 27 | 1 | 48 | |||||||
| Premolars | |||||||||||||
| Upper first | 2 | 1 | 1 | 4 | 1 | 9 | 26 (22.2%) | ||||||
| Lower first | 2 | 2 | 3 | 2 | 3 | 12 | |||||||
| Upper second | 1 | 1 | 2 | ||||||||||
| Lower second | 1 | 1 | 1 | 3 | |||||||||
| Incisors | |||||||||||||
| Upper canine | 1 | 1 | 1 (0.9%) | ||||||||||
| Sum | 6 | 32 | 10 | 40 | 1 | 2 | 6 | 13 | 5 | 1 | 1 | ||
| 89 (76.1%) | 21 (17.9%) | 7 (6.0%) | 117 | ||||||||||
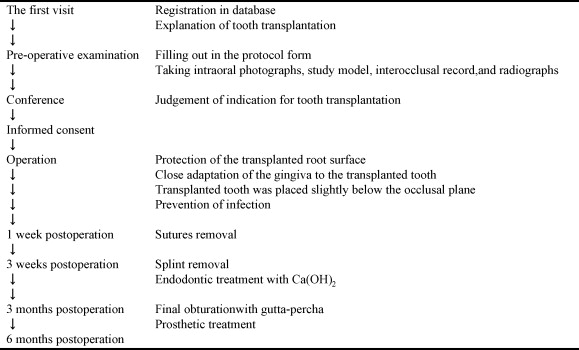
The treatment protocol for tooth autotransplantation in the authors’ hospital is outlined in Fig. 1 . All patients who visited the outpatient clinic for tooth autotransplantation were registered in the study database and the treatment protocol was explained at the first visit. The protocol for tooth transplantation was designed to evaluate the data concerning patient information, treatment and outcome without bias ( Table 2 ). The preoperative examination of the donor and recipient sites was carried out according to the protocol. The patients were allowed to discuss the treatment options with the medical team and decide whether autotransplantation should be performed.
| Variable factors | Examination | ||
|---|---|---|---|
| Pre-operation | Patient | Age | Intraoral photographs |
| Gender | Study model | ||
| Past disease | Interocclusal record | ||
| Smoking habit | Radiographs (panoramic and periapical) | ||
| Donor tooth | Source | ||
| Type | |||
| Pocket depth | |||
| State of eruption | |||
| Contact with oppositing tooth | |||
| History of having dental caries | |||
| History of restoration | |||
| History of root canal treatment | |||
| Recipient site | Position | ||
| Duration of the absence of teeth | |||
| Operation | Number of roots of the donor tooth | ||
| Root fracture of donor tooth at removal | |||
| Number of socket bone walls | |||
| Positional relation of donor tooth and recipient site | |||
| Need to adjust the donor tooth to fit the recipient site | |||
| Fixation (orthodontic wire and resin, or sutures) | |||
| Post-operation | 1, 2, and 3 weeks | Initial healing | Periapical radiograph |
| 3, 6, 9, and 12 months | Duration of endodontic treatment | Periapical radiograph | |
| Pocket depth | |||
| Root resorption | |||
| Delay of bone regeneration | |||
All surgery was performed under local anaesthesia, sometimes combined with sedation of the patient at the outpatient clinic. The surgical procedure was based on the technique described by A ndreasen et al. A standardized surgical technique was followed by 14 oral surgeons. The donor tooth was removed carefully, taking precautions not to injure the root surface. The labial, mesial, lingual or palatal, and distal surfaces of the donor tooth were sketched and photographed and the condition of the periodontal ligament was recorded after removal. The tooth was placed in a tooth storage solution or sterile saline while the recipient site was prepared. The donor tooth was positioned in the new socket and flaps were sutured back carefully adapting to the transplanted crown. The transplanted teeth were splinted with an orthodontic wire and resin or with 4–0 silk sutures if the occlusal clearance was not sufficient for the wire splint. Transplanted teeth were always placed slightly below the occlusal plane. All patients received antibiotic coverage with cefditoren pivoxil for 5 days and benzethonium chloride mouthwash for 1 week. The sutures were removed after 7 days and the wire splint was removed 3 weeks postoperatively. Throughout the surgical process, the variable factors were recorded as listed in Table 2 .
Endodontic treatment was carried out by an endodontist 3 weeks postoperatively. The treatment included debridement of the root canal system followed by an interim root canal filling with calcium hydroxide, which was replaced at 2-week to 3-month intervals. The condition of the root canal was monitored with radiographs, tactile sensation and a surgical operating microscope. All cases were obturated with thermoplasticized gutta-percha when no sign of failure was seen clinically and radiographically .
The prosthetic treatment was completed by the dentists who had recommended tooth transplantation for their patient or by dentists in the hospital.
The patients were clinically and radiographically reviewed at 1, 2, and 3 weeks and 3, 6, 9, and 12 months postoperatively, according to the protocol ( Table 2 ). Thereafter, the patients were followed up at intervals of 6–12 months.
All transplants were evaluated clinically and radiographically by two oral surgeons and were classified into 2 groups according to the postoperative results. The unsuccessful group included cases of transplant loss and cases in which the transplants had severe problems. The successful group included cases in which the transplants healed well in the recipient site ( Fig. 2 ) and those with only stable minor problems. The transplants in the unsuccessful group were judged based on the causes of failure, such as failure of initial healing ( Fig. 3 ), root resorption ( Fig. 4 ), periodontal inflammation ( Fig. 4 ), delay of bone regeneration ( Fig. 5 ), maxillary sinusitis caused by periodontal and/or periapical infection of the transplant or root fracture. Root resorption was diagnosed and classified into three types clinically and radiographically: inflammation resorption observed with periradicular radiolucency; replacement resorption observed with no clinical mobility, high tone of percussion, and disappearance of the periodontal space radiographically; and cervical root resorption observed with a radiolucency extending over the cemento-enamel junction.





