The purpose of evaluation of a patient with a sensory nerve injury is to obtain information about the circumstances of the injury and its subsequent course, perform an examination of the area containing the sensory dysfunction, complete a series of testing maneuvers that will outline the area of sensory deficit, quantify the magnitude and character of the deficit, and record it in an objective manner that can be used as a basis for comparison with serial examinations, if needed. Accurate and complete records of the evaluation are essential, because they may be important in making decisions regarding treatment of the nerve injury. Good medical records may be helpful in the case of legal action, and they are indispensable in retrospective studies of patient care.
To the clinician inexperienced in the management of sensory nerve injuries in the oral and maxillofacial regions, evaluation of a patient who has sustained an injury to one of the peripheral branches of the trigeminal nerve can be a frustrating or intimidating encounter. Although there are many advanced, sophisticated, and technologically involved methods for evaluating nerve function that are used primarily in laboratory and clinical studies by researchers, the clinical evaluation of an injured sensory nerve can be accurately and adequately done by the simple, straightforward evaluation presented in this article. Such evaluation can be completed by any clinician in less than 30 minutes for most patients. In the authors’ practice, a printed form is completed by the patient before being seen by the clinician, and this provides much essential information about the patient’s complaints, progress of symptoms and their severity, and effect on orofacial function. Various aspects of this form are presented and discussed. The results of the evaluation are easily interpreted, regardless of whether or not the clinician has microneurosurgical skills. In the case of a nonmicrosurgeon, information gained from the nerve injury evaluation will enable the clinician to make an appropriate decision regarding referral for further evaluation and/or possible microsurgical repair of a nerve injury. Alternative methods of nerve evaluation are discussed and can be perused further by the reader by consulting the references listed in Further readings.
The essential elements of the evaluation of the patient with a peripheral sensory nerve injury include the history; the general head, neck, and oral examination; neurosensory testing; imaging studies; diagnosis; and classification of the nerve injury. Each of these is discussed in this article.
History
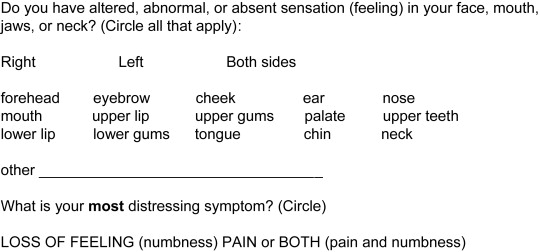
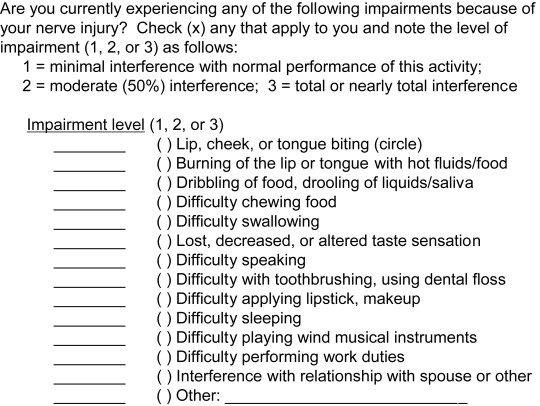
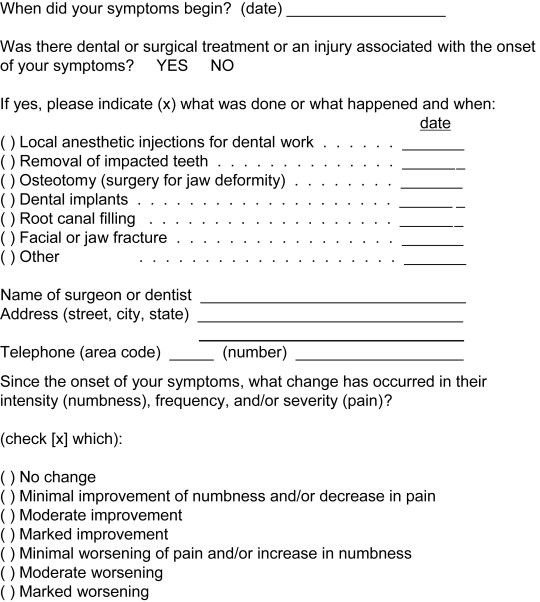
The history of a peripheral trigeminal sensory nerve injury begins with the patient’s chief complaint, or the reason that brought the patient to your attention. It is generally one of decreased or altered sensation (paresthesia), or of painful or unpleasant sensation (dysesthesia). It is important to distinguish between these 2 types of sensory dysfunction because the clinical examination of each is different (see later discussion). Some patients may complain of paresthesia and dysesthesia. Patients often have difficulty expressing themselves with regard to sensory symptoms, so the exact nature of their affliction may be better determined by having the patient complete a printed questionnaire before being seen for evaluation by the clinician ( Box 1 ).
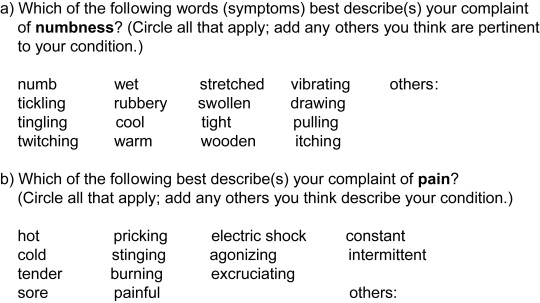
The patient who complains of decreased or altered sensation may state the problem as numbness. However, this is merely a lay term that requires clarification to be meaningful in the clinical sense. The patient who complains of numbness may be implying a level of altered sensation anywhere along a spectrum from minimal sensory loss to total loss of sensation, as well as some component of dysesthesia. To assist the patient in describing the nature of the sensory dysfunction, it is helpful to include a list of descriptive words on the printed form that the patient completes before being seen by the clinician ( Box 2 ). Patients may or may not complain of interference with everyday orofacial activities because of numbness. However, several functions, including speech, chewing food, and playing of wind musical instruments, are frequently found to be compromised when there is decreased or lost sensation.
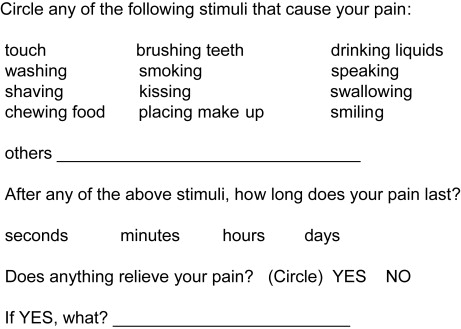
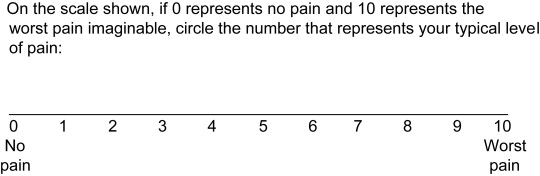
Patients who experience a painful or unpleasant sensation are asked whether it is constant or intermittent. Constant pain is usually seen in patients with long-term well-established dysesthesia. There is frequently a central component as well as that caused by the injured peripheral nerve. For instance, central pain may develop in time secondary to the loss of afferent input to the central nervous system (CNS) from the periphery, so-called deafferentation, caused by failure of transmission of the injured nerve. If the pain is intermittent, it may be spontaneous or stimulus induced. Spontaneous pain may be of brief duration (seconds) or longer (minutes to hours, or constant). Stimulus-induced pain is characteristically brief (seconds), and it is usually associated with the performance of a common, everyday maneuver by the patient. Such pain is usually described by the patient as hypersensitivity ( Box 3 ). The intensity or severity of the pain may be estimated by having the patient select descriptive words from a written list (see Box 2 ) or use a visual analog scale (VAS), in which 0 indicates no pain and 10 implies the worst pain the patient has ever experienced ( Box 4 ). The amount of estimated impairment of orofacial functions in either the patient with decreased altered sensation or unpleasant sensation is determined by having the patient complete the printed form shown in Box 5 .
Patients who have sustained a lingual nerve injury often complain of altered taste sensation (parageusia). The degree of taste impairment is estimated by the patient as part of the history of the present illness (see Box 5 ). Rarely, if ever, is altered taste the chief complaint of a patient with a lingual nerve injury.
The patient is asked whether there is anything that has relieved the pain (medications, application of heat or cold, rest, and so forth). In some patients with pain of long duration, there is a history of misuse or abuse of medications, and the patient may request prescription medications on the first visit. In most cases, this is inappropriate and should not be provided. Consultation with all the patient’s other practitioners may reveal multiple inappropriate prescriptions for medications with high addictive potential.
The history of the present illness includes the incident or operation (eg, lower third molar removal, mandibular osteotomy, placement of dental implant, maxillofacial fracture) that preceded the onset of the chief complaint, the date of its occurrence, the symptoms, and their progress or change in the time since onset, and any perceived orofacial functional impairments of which the patient complains. This information can best be determined by asking the following preliminary screening questions: (1) What happened to initiate the onset of your symptoms? (2) When (date) did it happen? (3) When did your primary symptom (numbness and/or pain) begin? (4) What is the progress or change in your symptom(s) since onset (getting worse, getting better, staying the same)? ( Box 6 ).
The incident or operation that initiated the onset of sensory symptoms is often helpful in locating the site of nerve injury. For example, if, after removal of the mandibular right third molar, a patient complains of right tongue numbness, there has most likely been an injury to the right lingual nerve (LN) in its location on the medial surface of the right mandible adjacent to the site of tooth removal; the patient who complains of right lower lip and chin numbness probably sustained an injury to the right inferior alveolar nerve (IAN) adjacent to the third molar socket. If, after a facial fracture involving the left inferior orbital rim, the patient complains of left midfacial and upper lip numbness, most likely the left infraorbital nerve (IFN) has been injured within the inferior orbital canal at or near its exit from the left infraorbital foramen. Sensory changes in the lower lip or chin following placement of dental implants are generally caused by direct contact of the IAN or mental nerve (MN) with a drill or the implant itself. Special notice is taken of the patient whose onset of altered sensation is without an associated incident or injury. Such a patient requires the evaluation presented here to rule out the presence of problems in the oral and maxillofacial regions. Failing to find a cause there, the patient should be referred to a neurologist for further evaluation of a central cause (tumor, vascular anomaly, infection, metabolic disorder, and so forth).
The date of the incident or onset of sensory changes is important because there is a timetable for the pathophysiologic response of a peripheral nerve to injury (Wallerian degeneration). In time, the axons distal to the injury site undergo necrosis and phagocytosis. Repair is attempted by outgrowth of axonal sprouts from the proximal nerve stump. If the distal nerve is not spontaneously recannulated by new axons within a critical period of time, its superstructure is replaced by scar tissue and becomes incapable of repair, either spontaneously or by surgical intervention. There is a well-known window of opportunity of approximately 6 months from the time of injury when surgical repair of a nerve gives the best chance of a favorable result. After that, success rates decrease greatly with each passing month until a critical mass of distal nerve tissue is replaced by scar and is no longer capable of repair. In humans, this time has been estimated to be between 9 and 15 months, depending on the age and general health of the patient, and other individual characteristics not yet fully appreciated. Therefore, it behooves the clinician who initially evaluates the patient with a sensory nerve injury to note the date of the injury as accurately as possible, so that surgical intervention that might be indicated for a nerve injury that is not resolving spontaneously can be done in a timely fashion.
Numbness or painful sensations may not begin at the same time as the incident or operation associated with the nerve injury. For instance, seepage of root canal medicaments from the tooth apex following an endodontic procedure may take 1 or more days to reach the adjacent inferior alveolar canal (IAC) and cause a chemical burn of the IAN. Or, after bone preparation for dental implant placement, edema secondary to heat generated by the drill may develop slowly with delayed compression of the IAN and the onset of lower lip numbness and pain not noted by the patient for up to 24 hours after the procedure. If the IAN is not directly injured but the bony wall of the IAC is disrupted during elevation and removal of a mandibular third molar, excessive bone may be regenerated during the healing process, causing narrowing of the canal diameter and delayed compression of the IAN from 1 to several months after tooth removal. Such examples serve to explain why, although most sensory nerve injuries result in immediate onset of symptoms, onset of sensory dysfunction is delayed in some patients.
The progress of sensory symptoms is important because, in a period of days, weeks, or months following the nerve injury, the patient may show improvement or deterioration in sensory status or undergo no change. The patient may also exhibit these changes in a period of repeated evaluations. In patients who are improving, an expectant course is followed, in which serial evaluations are done at regular intervals (weekly, biweekly, or monthly) as long as they continue to show documented subjective and objective improvement at each subsequent visit. A patient who fails to show improvement of neurosensory status from one evaluation to the next will not resume improvement sometime in the future. Therefore, this patient has reached a plateau, and a decision regarding surgical intervention should be considered at that time, rather than following the patient further in the vain hope of resumption of improvement. Whether or not a patient is improving is based not only on subjective information (the patient’s history) but also on objective evidence (discussed later). In the course of recovery from a sensory nerve injury, new symptoms may occur. Most commonly, persistent numbness is the patient’s first complaint. Although pain may be present initially as well, it often develops days or weeks later, and it may increase in frequency and duration, become episodic or constant, and be spontaneous or associated with orofacial maneuvers (discussed earlier).
Equipment
The well-equipped clinician’s office should already contain the instruments and supplies needed for examination of the patient with a sensory nerve injury. Sterile gloves, cotton swabs, tongue blades, or mouth mirror and calipers, as well as local anesthetic needles, carpules, and syringes are sufficient for most patients ( Fig. 1 ). A vitalometer (pulp tester) is sometimes helpful as an alternative method of assessing response to pain.

Equipment
The well-equipped clinician’s office should already contain the instruments and supplies needed for examination of the patient with a sensory nerve injury. Sterile gloves, cotton swabs, tongue blades, or mouth mirror and calipers, as well as local anesthetic needles, carpules, and syringes are sufficient for most patients ( Fig. 1 ). A vitalometer (pulp tester) is sometimes helpful as an alternative method of assessing response to pain.

Head, neck, and oral examination
An examination is completed on all patients to include eyes, ears, nose, face, temporomandibular joints, neck, oral cavity, and pharynx. The components of the screening examination specific for the patient with sensory nerve injury are outlined in Fig. 2 . The first step is inspection. On the patient who has sustained acute trauma, the examiner looks for evidence of an acute injury (missile wound, laceration, facial bone fracture, other trauma). A nerve transsection, avulsion, partial tear, compression, or crushing may be able to be directly visualized through a wound or laceration. In other patients, the clinician looks for evidence of recent or past injury or surgery (eg, lacerations or incisions, or scars from previous wounds), or neurotrophic changes of the skin (edema, erythema, ulcerations, hypohydrosis, loss of hair, hypokeratosis) that may occur following sensory loss in that area. The patient with long-standing sensory nerve dysfunction may subject the affected soft tissues to repeated factitious (self-induced) habits ( Fig. 3 ). In the neck, scars from past injury or incision in response to stimulation (gentle stroking with the examining finger or a cotton swab) may exhibit symptoms and signs of sympathetic nervous system hyperactivity (hyperesthesia, sweating, blanching, flushing, skin temperature changes) in the skin area supplied by the injured nerve. Such signs may indicate so-called sympathetic-mediated pain (SMP; also known as reflex sympathetic dystrophy [RSD]) ( Fig. 4 ).