Alloplastic chin implants have been a valuable treatment modality for the correction of microgenia. Their use has provided satisfactory esthetic results by improving facial balance. However, bone resorption under these implants can occur. Case reports of 4 patients with the incidental radiographic finding of the presence of chin implants are presented. All 4 subjects had lateral cephalograms and panoramic x-rays taken as part of their orthodontic evaluation. One had a normal mandibular symphyseal contour, and 3 had bone resorption under the implants. One subject had severe resorption. In addition to panoramic and cephalometric x-rays, the subject with severe resorption also had magnetic resonance imaging and computerized tomography as part of the evaluation workup.
Highlights
- •
Bone erosion can occur under chin implants.
- •
A patient may be unaware of it.
- •
An orthodontist could radiographically diagnose it in the initial evaluation.
Microgenia is often called chin retrusion or recessive chin, and it is the most frequently found type of chin deformity, occurring mostly in the sagittal plane. Chin retrusion can be determined cephalometrically or clinically by evaluation of the patient’s facial profile or lateral facial photos.
In 1934, Aufricht reported the use of autogenous nasal hump bone for chin augmentation. Hofer performed an externally approached osseous genioplasty with a horizontal osteotomy to advance a receding chin on cadavers in 1942. Converse used intraorally inserted bone grafting in the 1950s to advance the chin, and in 1957 Trauner and Obwegeser developed an intraoral approach for a sliding osteotomy of the chin.
Alloplastic biomaterials have been used for implant prostheses. Silicone (polydimethylsiloxane) was first used for chin augmentation procedures in the early 1950s by Brown et al and by Millard. Proplast (Vitek, Houston, Tex) was introduced in 1977 by Dann and Epker but was later recalled from the market because it was associated with potential complications. Other alloplastic materials later introduced include Mersilene mesh, a polyester fiber sheeting (Ethicon, Somerville, NJ); Gore-Tex, expanded polytetrafluoroethylene (W. L. Gore & Associates, Flagstaff, Ariz); Medpor, porous high-density polyethylene (Porex Surgical, College Park, Ga); and Silastic, a medical-grade silicone rubber (Dow Corning, Midland, Mich).
Although silicone has been reported to be widely used among surgeons treating this condition, the use of diced polyethylene in a surgicel oxidized cellulose mesh (Johnson & Johnson, Somerville, NJ) was advocated by Gurlek et al, whereas Mersilene mesh has been the option for others.
Bone resorption, at times also called bone erosion, is a risk associated with the use of allopastic chin implants. It was first described by Robinson and Shuken in 1969. Bone resorption under the implant’s surface in contact with the mandible is a high risk and occurs quite often. Despite this fact, chin implant placement by plastic, facial, and maxillofacial surgeons is frequent. According to the American Society of Plastic Surgeons, 18,136 alloplastic chin augmentation procedures were performed in the United States during 2014. Procedural data and statistics have been gathered by the American Society of Plastic Surgeons for several years and reported to the public since 2005.
Possible etiologies of bone resorption are inadequate implant positioning, soft tissue pressure on the implant, subperiosteal placement, oversized prosthesis selection, implant compactness and firmness, sex, and age. Hypercontraction of the mentalis muscle to overcome lip incompetence has been shown by Matarasso et al as a possible etiologic factor and lip incompetence as a marker for progressive bone resorption under chin implants. According to them, patients with obtuse labiomental angles have greater resorption than do those with acute angles.
Classification and prevalence of bone resorption (erosion) have been addressed in the past. In 1972, Robinson introduced a classification for chin implant bone erosion based on the amount of resorption (depth) compared with the size of the implant used, as observed on lateral skull radiographic views ( Table I ). An alternate classification method was later introduced by Guyuron et al based solely on the depth of bone invaded ( Table II ).
|
|
In a retrospective study, Friedland et al used lateral cephalograms to determine the incidence of bone resorption under chin implants. Over 50% of their sample had bony erosion. A dental computed tomography (CT) software program (DentaScan; General Electric, Milwaukee, Wis) has been recently used for the evaluation of mandibular erosion arising from silastic implants.
The purpose of this report was to create awareness among orthodontists about the existence of chin implant-related bone erosion among adults seeking our services. It will also benefit readers by suggesting management alternatives once diagnosed. Four patients were used to describe the cephalometric and panoramic radiographic findings of varying degrees of bone erosion induced by surgically positioned chin implants.
Lateral cephalograms and panoramic x-rays of 4 subjects with incidental findings of alloplastic chin implants are presented, and magnetic resonance images and CT scans were also available for 1 subject. The images were evaluated for implant position related to the anatomy of the chin, presence and size of the bone defect, and relationship of the defect to the root apices. Four surgeons placed the implants, and the implants’ compositions varied in the sample. Consent to use the radiographs and images was obtained from all 4 subjects.
Case reports
Patient 1
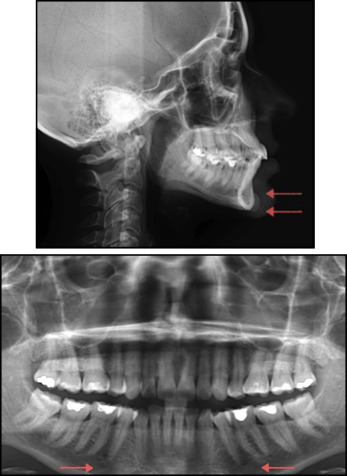
A 39-year-old woman, whose lateral cephalogram showed a small 0.45-cm silicone chin implant, had a normal mandibular symphyseal bony contour. The mandible and chin area as observed in her panoramic dental x-ray were also unremarkable. When the radiograph was obtained, the implant had been in place for 10 years and had been placed by surgeon 1. The patient was asymptomatic. A normal bone pattern was observed, with no radiographic evidence suggesting possible mandibular bone erosion under the implant ( Fig 1 ).
Patient 2
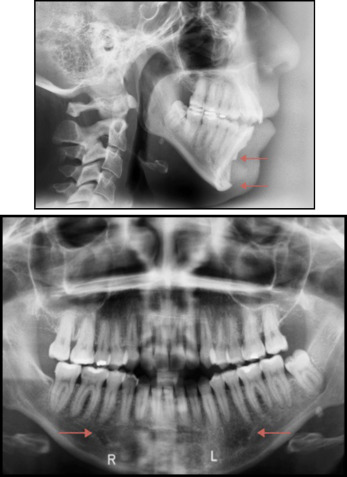
A 32-year-old woman had a medium-sized implant of approximately 0.7 cm. The type of biomaterial used was unknown. When the radiograph was taken, the implant placed by surgeon 2 had been in place for 17 years. An elongated, C-shaped concavity superior, posterior, and inferior to the implant of approximately 3.0 mm and penetrating deeper than the cortex was observed in her initial lateral cephalogram (Robinson grade I, Guyuron grade 2). Her panoramic radiograph showed a subtle symmetric radiolucency in the parasymphyseal region of the mandible ( Fig 2 ).
Patient 3
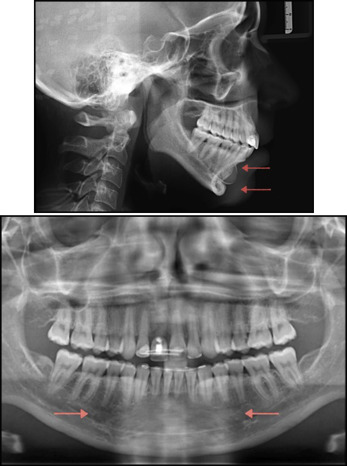
A 32-year-old woman had a large, 0.9-cm silicone implant. When the radiograph was obtained, the implant placed by surgeon 3 had been in place for 10 years. A rounded C-shaped concavity mostly posterior and inferior to the implant of approximately 0.5 cm and penetrating almost into the internal portion of the lingual symphyseal cortex was observed in her routine initial lateral cephalogram (Robinson grade II, Guyuron grade 3). Her panoramic radiograph showed a mild radiolucency in the mandibular body, elliptical in shape, which included the parasymphyseal region and extended from the right to the left premolar areas ( Fig 3 ).
Patient 4
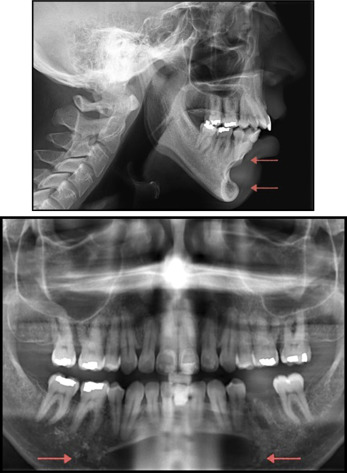
A 33-year-old man had an extra-large Mersilene mesh chin implant, measuring approximately 5.0 cm in length and with 1.4 cm in the anterior projection. The implant placed by surgeon 4 had been in place for 10 years. A rounded C-shaped concavity located posterior to the implant, measuring approximately 0.7 cm in depth, and with significant intrasymphyseal penetration, was observed in his routine initial lateral cephalogram (bone erosion: Robinson grade III, Guyuron grade 4). The erosive area was close to the apices of the teeth. His panoramic radiograph showed a large elliptical lucent lesion with well-defined, thin, sclerotic borders. The lesion was located in the right and left bodies of the mandible and in the parasymphyseal mandibular region, and was close to the anterior dentition ( Fig 4 ). His anteroposterior cephalogram showed a radiolucent spherical area in the parasymphyseal region of the mandible. The patient underwent axial and coronal magnetic resonance imaging ( Fig 5 ) and a CT scan of the head ( Fig 6 ). Axial magnetic resonance images showed the implant as an oblong T1 and T2 hypointense structure resulting in erosion of the buccal cortex of the mandible and marked thinning of the medullar space. The accompanying CT image through the same level, using bone window settings, demonstrated how the buccal cortex and medullar space were completely eroded at this level. The lingual cortex was severely thinned. Endodontic evaluation of the mandibular incisors, canines, and premolars was performed. All teeth were vital. The surgeon who placed the implant was consulted. Removing the implant was considered but not performed because the procedure had a high risk of soft tissue disfigurement at the chin. Six months after orthodontic treatment was started on this patient in preparation for a mandibular advancing osteotomy, he sustained a mandibular fracture, and several mandibular teeth were completely avulsed as a result of trauma to the mandible in a car accident. The orthognathic correction for this patient is on hold, pending prosthetic rehabilitation.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


