Armamentarium
|
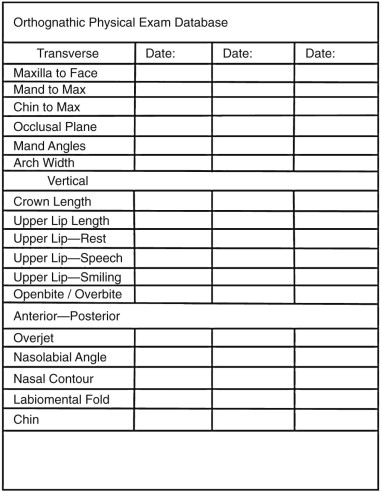
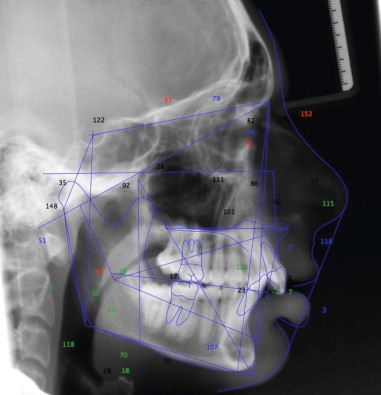
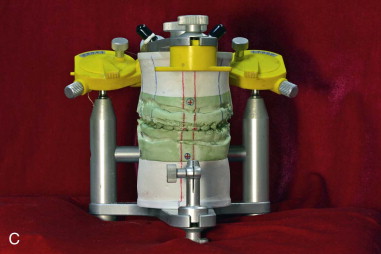
The armamentarium for bimaxillary orthognathic surgery is essentially the combination of the armamentaria for maxillary and mandibular orthognathic procedures. However, the need for precise, accurate preoperative records is magnified by the fact that both jaws are being repositioned at one sitting, and therefore when the second jaw is repositioned it is indexed by the newly positioned other jaw. If the new position of the first operated jaw is slightly off in any of the three planes of space that may not be clearly apparent at the time, this may result in a completely unsatisfactory placement of the second jaw. The preoperative three-dimensional examination ( Figure 42-1 ), cephalometric study ( Figure 42-2 ), bite registration, and articulator mounting ( Figure 42-3 ) all play a more crucial role in completing the two-jaw surgery satisfactorily. A note of caution: Preoperative photos do not take the place of a good, in-person clinical exam ination to evaluate critical areas such as tooth-lip relationship (repose and functioning), cants, and midlines.



History of the Procedure
The history of simultaneous maxillary and mandibular orthognathic surgery is unclear. It is likely that two-jaw surgeries were performed many years before any published reports were made. Subapical segmental surgeries such as that reported by Hullihen in 1849 were probably combined with subapical surgery of the anterior maxilla for the treatment of bimaxillary protrusion and anterior openbite.
History of the Procedure
The history of simultaneous maxillary and mandibular orthognathic surgery is unclear. It is likely that two-jaw surgeries were performed many years before any published reports were made. Subapical segmental surgeries such as that reported by Hullihen in 1849 were probably combined with subapical surgery of the anterior maxilla for the treatment of bimaxillary protrusion and anterior openbite.
Indications for the Use of the Procedure
Bimaxillary orthognathic surgery is indicated under the following conditions:
- •
The magnitude of movement for single jaw orthognathic surgery is unrealistic.
- •
Asymmetries necessitate three-dimensional repositioning of both jaws (generally, maxillary dental midline deviation of 1.5 to 2 mm or less from the facial midline is considered acceptable; however, the decision as to whether or not to operate on the maxilla must be made with the advice and consent of the patient, family, and orthodontist ).
- •
There is a significant cant to one or both jaws.
- •
Telegnathic surgery is being performed for obstructive sleep apnea syndrome.
- •
Mandibular surgery is needed and maxillary transverse dimension requires widening, and surgically assisted rapid maxillary expansion is not indicated.
Limitations and Contraindications
Bimaxillary orthognathic surgery is contraindicated when an acceptable surgical result can be achieved with single-jaw surgery, when medical factors limit the duration of general anesthesia, when a hemorrhagic disorder precludes multiple surgical procedures, and when potential blood transfusions are refused or contraindicated.
Technique: Bimaxillary Orthognathic Surgery
In the initial patient evaluation before any treatment, it is necessary to predict the possible need for two-jaw surgery. If it is obvious that only mandibular surgery is necessary, then no further considerations may be required at this early stage. However, if maxillary surgery is considered, mock surgery is necessary to evaluate the impact of that maxillary surgery on the mandibular autorotation position and subsequently new maxillary position. Although clinical and cephalometric evaluations are important, model surgery or computerized virtual surgery on centric relation mounted models is the only accurate method to determine the autorotation of the mandible after maxillary repositioning. This exercise may reveal that the maxilla will be drawn more posterior than desired or that the maxilla will be deflected laterally when condyles are seated. In such cases, two-jaw surgery may be the only alternative to correct all of the discrepancies. This knowledge is important to properly plan the combined orthodontic-surgical treatment with the orthodontist, to inform the patient of the anticipated treatment plan, and to submit accurate insurance preauthorization.
Step 1:
Presurgical Assessment
Preoperative assessment is vital in all orthognathic surgeries. Preparation for bimaxillary orthognathic surgery needs to be more detailed than that for isolated maxillary or mandibular orthognathic surgery, because mobilizing both jaws provides more freedom in three-dimensional positioning. With more freedom in this positioning, there is greater need for detailed preoperative measurements to achieve the desired outcome position. Standard radiographic assessment includes lateral cephalometric radiographs and analysis, anteroposterior (AP) cephalometric radiographs and analysis, and a panoramic radiograph (see Figure 42-2 ). Facial database gathering must include evaluation of vertical, AP, and transverse dimensions as well as the dental occlusion (see Figure 42-1 ).
Step 2:
Establishment of Rough Movement Goals
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


