Introduction
Various methods have been proposed to evaluate a patient’s developmental status. However, most of them lacked precision and failed to give a reliable estimate of skeletal maturity. The aims of this study were to evaluate the association between frontal sinus morphology and cervical vertebral maturation for the assessment of skeletal maturity and to determine its validity in assessing the different stages of the adolescent growth spurt.
Methods
A cross-sectional study was performed on the pretreatment lateral cephalograms of 252 subjects aged 8 to 21 years. The sample was divided into 6 groups based on the cervical vertebral maturation stages. The frontal sinus index was calculated by dividing the frontal sinus height and width, and the cervical stages were evaluated on the same radiograph. The Kruskal-Wallis test was applied to compare frontal sinus index values at different cervical stages, and the post hoc Dunnett T3 test was applied to compare frontal sinus index values between adjacent cervical stages for each sex. The Kendall tau-b values were computed to assess the correlation between the cervical stages and the sinus index. A P value of ≤0.05 was considered statistically significant.
Results
The height and width of the frontal sinus were significantly larger in the male subjects than in the females. A significant association was found between the frontal sinus height and width and cervical stages ( P ≤0.001) in both sexes. However, the changes in the frontal sinus index across the different cervical stages were found to be significant ( P ≤0.001) in male subjects only. Similarly, a weak negative correlation was found between the sinus index and the cervical stages in male subjects (tau-b = −0.271; P <0.001), whereas no correlation was found in female subjects (tau-b = −0.006; P <0.928). However, the post hoc analysis showed that the values of the sinus index were comparable between any 2 adjacent cervical stages.
Conclusions
The frontal sinus index cannot be used to identify the prepubertal, pubertal, and postpubertal stages of the adolescent growth spurt. Therefore, it cannot be used as a reliable maturity indicator.
Highlights
- •
A well-defined adolescent growth spurt is shown by frontal sinus enlargement.
- •
Frontal sinus height and width are associated with the cervical stages.
- •
Frontal sinus index failed to differentiate between adolescent growth spurt periods.
Human growth from infancy to maturity involves dynamic changes in body size and shape. The assessment of growth potential during the preadolescent or adolescent growth spurt has considerable influence on orthodontic diagnosis and treatment planning as well as outcome and stability. Similarly, the analysis of growth plays a vital role in the orthodontic decision-making process.
Chronologic age fails to provide an accurate diagnosis of the growth status of a child, since children of the same chronologic age usually have variable degrees of skeletal maturation. In this context, various parameters have been used as maturity indicators for growth assessment in children. The classic parameters include changes in body height and weight, appearance of secondary sexual characteristics, chronologic age, tooth mineralization and calcification, and skeletal maturation.
Skeletal maturity can be assessed by visually inspecting the developing bones, their initial appearance, sequential ossification, and changes in size and shape of the bones of the hand, wrist, and elbow on radiographs. The ossification of bones of the hand and wrist is considered the most accurate method; however, it requires an additional exposure of radiation, leading to ethical limitations. To further reduce this radiation exposure, Lamparski evaluated the maturation of the cervical vertebrae on lateral cephalograms, and it was reported that cervical vertebral maturation correlated with the skeletal maturation of a child.
The cervical vertebral maturation method is currently the most widely used method to assess the growth status of a child. However, it carries certain limitations: eg, difficulty in classifying cervical vertebral bodies 3 and 4 as trapezoidal, rectangular horizontal, square, or rectangular vertical. Moreover, division of the pubertal growth spurt into discrete stages is inappropriate to describe a continuous phenomenon.
Changing morphology of the frontal sinus during the adolescent growth spurt is a new method of assessing the developmental status of a child. Even though there are several reports on the development of the frontal sinus, few studies have investigated the relationship of the frontal sinus with other growth parameters. Ruf and Pancherz evaluated frontal sinus morphology on lateral cephalograms and reported a well-defined pubertal growth spurt in the enlargement of the frontal sinus. However, to assess the clinical relevancy of frontal sinus morphologic variations in assessing the developmental status of a child, we planned this study with an aim to determine the association of frontal sinus height, width, and index with cervical vertebral maturation.
Material and methods
Data were collected retrospectively from the pretreatment lateral cephalograms of orthodontic patients visiting our dental clinics at Aga Khan University Hospital in Karachi, Pakistan. The sample size was calculated in OpenEpi software (version 3.0) using the findings of Patil and Revankar, who showed a mean difference in the frontal sinus index at different skeletal maturation stages of 0.25 ± 0.26. The power was set at 80%, and alpha was taken as 0.05 to calculate the sample size, for a sample of 42 subjects in each cervical stage needed to conduct the study. Thus, the total sample consisted of 252 subjects, uniformly divided into 6 cervical stages having equal numbers of males and females.
Subjects with good-quality standardized pretreatment lateral cephalograms and aged between 8 and 21 years were included in the study. Subjects with a history of sinus-related pathologies; any craniofacial anomaly, syndrome, trauma, or surgery involving the frontal sinus or the cervical vertebrae; or any systemic disease affecting growth and development were excluded from the study.
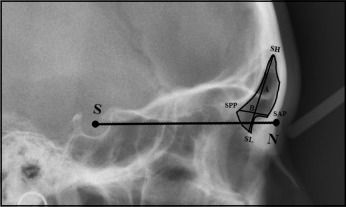
The digital images of the lateral cephalogram were analyzed and measured using View Pro-X (Rogan-Delft, Veenendaal, The Netherlands) software for precise and accurate data collection. The frontal sinus height and width measurements were analyzed using the method of Ertuk. The cephalogram was oriented with the sella-nasion line horizontal. The maximum height and width of the sinus were measured as shown in Figure 1 . The ratio between the frontal sinus height and width was calculated for each patient and was regarded as the sinus index.
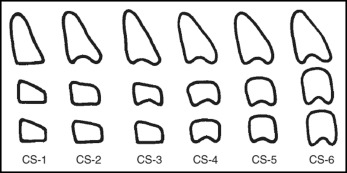
The cervical vertebral maturation stages were assessed on the same lateral cephalogram using the method of Baccetti et al ( Fig 2 ).
The data were double entered and analyzed in SPSS software for Windows (version 19.0; IBM, Armonk, NY). The Shapiro-Wilk test was used to check the normality of the data, which showed a nonnormal distribution; hence, nonparametric tests were applied. The Mann-Whitney U test was used to compare frontal sinus measurements in both sexes. Comparisons between frontal sinus measurements among the different cervical stages were made using the Kruskal-Wallis test. The post hoc Dunnett T3 test was applied to compare frontal sinus index values at adjacent cervical stages. The Kendall tau-b correlation was used to determine the correlation between frontal sinus measurements and cervical stages in the sexes. A P value of ≤0.05 was considered statistically significant.
To rule out any measurement error, 30 cephalograms were randomly selected and reassessed by the principal investigator (H.T.M.). The errors were calculated according to the Dahlberg equation, and the coefficient of reliability was calculated as described by Houston. The measurement errors were found to be small and ranged from 0.002 to 0.36 mm, and the coefficients of reliability varied from 0.97 to 0.98. The intraclass correlation coefficient showed that the repeated measurements were highly reproducible ( Table I ).
| Variable | Reading 1 (n = 30) | Reading 2 (n = 30) | ICC | Dahlberg’s calculation | Houston’s coefficient of reliability |
|---|---|---|---|---|---|
| Frontal sinus height (mm) | 27.80 ± 6.89 | 27.75 ± 6.90 | 0.996 | 0.36 | 0.98 |
| Frontal sinus width (mm) | 10.93 ± 1.27 | 10.97 ± 1.37 | 0.993 | 0.02 | 0.97 |
| Frontal sinus index | 3.02 ± 0.62 | 3.02 ± 0.60 | 0.997 | 0.002 | 0.98 |
Results
The frontal sinus height, width, and index were compared between the sexes; this showed significant differences, with males having greater sinus heights and widths, and females having greater values of the sinus index ( Table II ). Further statistical analyses were performed separately for each sex.
| Frontal sinus parameter | Male (n = 126) (mean ± SD) | Female (n = 126) (mean ± SD) | P value |
|---|---|---|---|
| Frontal sinus height (mm) | 28.80 ± 7.74 | 26.30 ± 6.35 | 0.006 ∗ |
| Frontal sinus width (mm) | 11.92 ± 9.68 | 9.05 ± 2.56 | <0.001 † |
| Frontal sinus index | 2.67 ± 0.51 | 2.98 ± 0.58 | <0.001 † |
Significant differences were found in frontal sinus heights and widths at different cervical stages in each sex, whereas a statistically significant ( P ≤0.001) difference between the frontal sinus index at different cervical stages was found in male subjects only ( Table III ; Fig 3 ).
| Cervical stage (CS) | Sex | CS 1 | CS 2 | CS 3 | CS 4 | CS 5 | CS 6 | P value |
|---|---|---|---|---|---|---|---|---|
| Frontal sinus height (mm) | Male | 19.32 ± 4.03 | 25.23 ± 5.26 | 26.20 ± 6.54 | 31.39 ± 4.51 | 33.51 ± 4.20 | 37.17 ± 5.60 | <0.001 ∗ |
| Female | 19.91 ± 5.38 | 23.22 ± 4.70 | 25.14 ± 4.92 | 28.30 ± 3.55 | 29.92 ± 6.29 | 31.27 ± 5.17 | <0.001 ∗ | |
| Frontal sinus width (mm) | Male | 6.51 ± 1.84 | 9.51 ± 1.85 | 10.34 ± 2.22 | 11.54 ± 2.00 | 13.00 ± 2.17 | 15.88 ± 2.41 | <0.001 ∗ |
| Female | 7.12 ± 1.88 | 7.83 ± 1.99 | 8.23 ± 1.59 | 9.57 ± 2.31 | 10.71 ± 2.50 | 10.85 ± 2.55 | <0.001 ∗ | |
| Frontal sinus index | Male | 3.09 ± 0.67 | 2.67 ± 0.45 | 2.56 ± 0.50 | 2.75 ± 0.41 | 2.60 ± 0.35 | 2.36 ± 0.35 | <0.001 ∗ |
| Female | 2.83 ± 0.54 | 3.06 ± 0.60 | 3.10 ± 0.56 | 3.11 ± 0.83 | 2.83 ± 0.40 | 2.95 ± 0.43 | 0.618 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


