Armamentarium
|
History of the Procedure
Anterior iliac crest bone grafting (AICBG) has been part of oral and maxillofacial surgery reconstruction for close to a hundred years. Its use was initially noted during the First World War by German surgeons, Lindemann of Dusseldorf and Klapp of Berlin. By 1917, the use of iliac crest bone grafts for mandibular reconstruction had become widespread practice. The ilium was firmly established as a source of bone for defects of the jaw in July, 1920, when Gilbert Chubb reported on 60 cases of bone grafting in the mandible. Original reconstructive methods for the facial bones relied on free bone graft blocks, which often are dense and have little cellularity.
In 1944, Rainsford Mowlem used cancellous chip grafts for reconstruction, noting increased cellularity and satisfactory healing within weeks. With further refinement of fixation techniques, corticocancellous blocks or particulate bone chips from the ilium were used for mandibular reconstruction, with good success. The technique for harvesting bone from the anterior ilium has largely gone unchanged. The soft tissue surgical approach is universally accepted by patients. Minor modifications in the bone harvesting techniques are mostly attempts to reduce postoperative pain and gait disturbances. Minimally invasive outpatient techniques also are available for harvesting cancellous bone from the anterior ilium with trephines and reamers.
History of the Procedure
Anterior iliac crest bone grafting (AICBG) has been part of oral and maxillofacial surgery reconstruction for close to a hundred years. Its use was initially noted during the First World War by German surgeons, Lindemann of Dusseldorf and Klapp of Berlin. By 1917, the use of iliac crest bone grafts for mandibular reconstruction had become widespread practice. The ilium was firmly established as a source of bone for defects of the jaw in July, 1920, when Gilbert Chubb reported on 60 cases of bone grafting in the mandible. Original reconstructive methods for the facial bones relied on free bone graft blocks, which often are dense and have little cellularity.
In 1944, Rainsford Mowlem used cancellous chip grafts for reconstruction, noting increased cellularity and satisfactory healing within weeks. With further refinement of fixation techniques, corticocancellous blocks or particulate bone chips from the ilium were used for mandibular reconstruction, with good success. The technique for harvesting bone from the anterior ilium has largely gone unchanged. The soft tissue surgical approach is universally accepted by patients. Minor modifications in the bone harvesting techniques are mostly attempts to reduce postoperative pain and gait disturbances. Minimally invasive outpatient techniques also are available for harvesting cancellous bone from the anterior ilium with trephines and reamers.
Indications for the Use of the Procedure
The anterior ilium can be a source for bone grafting in most facial reconstruction cases that can be managed by a free nonvascularized autograft. The ilium, once considered the gold standard as a donor site, allows transplantation of a large concentration of osteocompetent cells. However, with free tissue transfer, use of the ilium is changing. A discussion of the indications for free tissue transfer versus nonvascularized bone grafts is beyond the scope of this chapter.
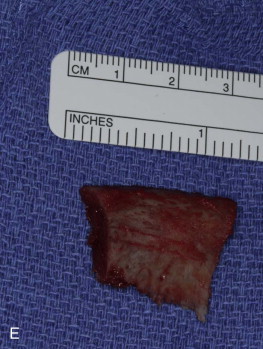
The anterior ilium, unlike other sites such as the calvaria or tibia, can provide both corticocancellous blocks and just cancellous marrow for use in grafting. Most reconstructive cases that require 50 cc or less of bone can be managed with a single anterior ilium. This amount of bone can reconstruct a 5-cm defect, assuming each centimeter of defect requires 10 cc of bone. Another indication is based on the ability to harvest the anterior ilium in a two-team approach for a free bone graft; this can shorten operating room and anesthesia time.
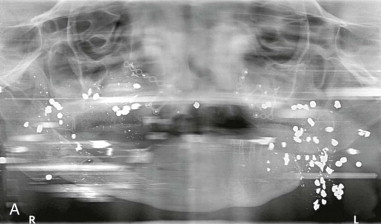
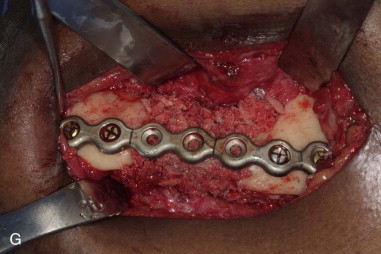
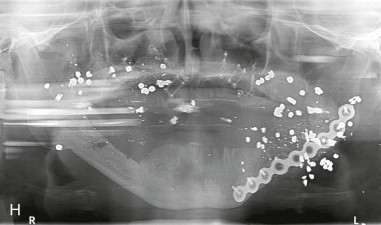
The most common procedures that use the anterior ilium include correction of post-traumatic deformities (malunion, nonunion), postablative reconstruction of the jaws (odontogenic cysts, small benign tumors), orthognathic procedures, alveolar cleft grafts, and reconstruction of atrophic jaws for future dental implants (sinus augmentation, ridge augmentation) ( Figure 121-1 ).


Limitations and Contraindications
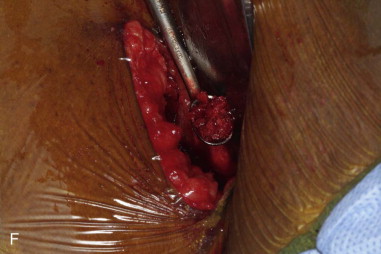
Use of the anterior ilium requires strict sterile technique, often necessitating general anesthesia in the operating room. On average, the region of bone harvest in the anterior ilium yields 15 to 20 cc of noncompressed bone, with a maximum of 50 cc in some individuals. Consequently, defects larger than 4 to 5 cm cannot be reconstructed from a single harvest site. Another limitation is obesity, which can distort the anatomy and make the surgical approach more difficult. Patients with a history of hernia repairs can be at risk for inadvertent abdominal penetration. In patients with hip prostheses, the anterior ilium should not be harvested on the affected side, to avoid any confusion of symptoms and to reduce the risks of hardware failure and infection.
Contraindications to anterior ilium harvest include previous trauma or infection of the surgical site. Systemic factors, such as metabolic bone diseases, also should be taken into consideration. Relative contraindications include bisphosphonate use, chemotherapy, irradiation of the site, and/or long-term steroid use.
Technique: Medial Approach
Step 1:
Patient Preparation and Positioning
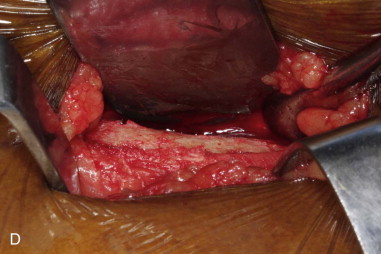
General anesthesia is obtained using endotracheal intubation, and the patient is placed in the standard supine position. A soft roll or saline bag wrapped in a towel is used as a bump under the gluteal region on the side of harvest to elevate and rotate the hip, making it more accessible. More often, the bone harvest involves a two-team approach, and the second surgical site should be separately draped in anticipation. In prolonged procedures, the bump should be removed from underneath the gluteal region once the bone graft has been obtained. Keeping the lower spine rotated for an extended period may add to the postoperative discomfort of the patient ( Figure 121-2, A ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


