After approximately 10 years of clinical practice, alveolar distraction osteogenesis has evolved in reconstruction of the jaw and alveolus into three options: (1) definitive alveolar distraction osteogenesis—used to finalize reconstruction and establish an ideal alveolar ridge (orthoalveolar form), (2) adjunctive alveolar distraction osteogenesis—used as part of a bone grafting scheme for gaining increased bone mass, and (3) orthognathic alveolar distraction—used to obtain alveolar alignment and obtain a class I arch relation (orthoalveolar relation).
Each case is evaluated considering the defect that is present and the overall osteogenic potential of the remaining bone segments. With small defects, when there is plentiful bone stock available, definitive alveolar distraction is ideal. When the bone is atrophic or there is low volume bone stock in a scarred or ablated soft tissue bed, distraction is not as successful. The same factors that make bone grafting difficult make alveolar distraction difficult. Understanding the biomechanical factors present in each case allows the correct protocol to reconstruct the jaws based on what is biologically feasible. Because few clinicians do alveolar distraction, they must rely on the experiences of others as found in the literature. There are few published prospective studies, however, on alveolar distraction. Most of the protocols that are available were done when technology was in the developmental phase. The purpose of this article is to establish diagnostic and treatment planning criteria including presentation of a site classification to help establish treatment. When and how to use various distraction devices are only one part of the equation. It is perhaps more important that clinicians conceptualize what is achievable, by distraction or bone grafting, in the effort to recover orthoalveolar form.
Invenio quod defectio (discover what is missing) has become the dictum of restorative oral and maxillofacial surgeons. Previous efforts to place dental implants for support of prostheses, without regard to alveolar shape and projection, no longer are acceptable treatment in the vast majority of partially edentulous patients. Even in fully edentulous cases, efforts are made to regain a natural prosthetic restoration.
Diagnostic treatment planning
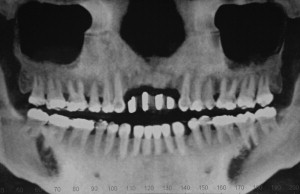
A cone beam CT scan or standard tomographic image helps establish the extent of alveolar deficiency in terms of quantity and quality of remaining bone ( Fig. 1 ). Clinically, restorative dentists determine the restorative scheme estimating the need for alveolar augmentation. In some cases, the alveolar bone may even need to be reduced. Study casts are placed on an articulator and a diagnostic wax-up is done ( Figs. 2 and 3 ). From the wax-up, a surgical template is made to help a surgeon reconstruct the alveolus. The clinical (benchtop) diagnostic work-up, therefore, is more important than a radiographic evaluation.


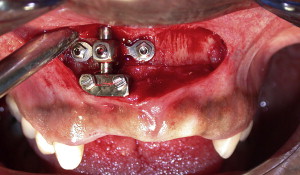
After clinical and radiographic evaluation, a decision is made regarding the augmentation requirement, implant placement locations, and the need for distraction osteogenesis. Depending on the size of the defect, reconstruction may require grafting, distraction, or a combination of the two. After reconstruction of the ridge and after the augmented (restored area) has healed, a conservative number of implants should be placed. Too many implants, placed too close together, can disrupt a viable augmentation and lead to late-term resorption and remodeling. Hence, the final prosthetic treatment plan must have surgical and restorative input with regard to the extent of augmentation and the number and width of implants to be placed in the augmented area.
When distracting segments, restorative needs should decide the endpoint of the active distraction. Modifications of a temporary appliance to accommodate the volume of bone and soft tissue are done as needed. The decision of when to stop active distraction is part of the planning process done in conjunction with model planning. In general, an overdistracted position of approximately 2 or 3 millimeters is recommended to allow for remodeling and future surgical-prosthetic modification at the time of implant placement ( Figs. 4–8 ).




Defect assessment
Conceptually, an ideal edentulous alveolar osseous morphology (orthoalveolar form) should be recreated in 3-D. This means that the facial and palatal marginal bone height and adjacent supporting bone are present. After a dental extraction, these dimensions can be lost unless socket preservation grafting is done. The pattern of loss is highly variable and somewhat dependent on the trauma of extraction and concurrent infection. Postextraction studies have demonstrated significant facial plate resorption within 6 weeks of dental extraction, especially evident in the postorthodontic anterior maxillary dentition. Postextraction findings can range from mild to severe facial plate loss ( Figs. 9–11 ). When the lingual plate of bone is lost, the site becomes a vertical alveolar defect, which is much more difficult to treat without distraction osteogenesis. Finally, if bone is lost next to an adjacent tooth leaving an exposed root surface, the defect is a difficult lesion to treat. This is true especially if the involved teeth are retained ( Figs. 12–14 ).








