Specific alternatives to traditional complete denture therapy have been controversial because of the uncertainties surrounding effectiveness of retention. This article addresses the importance of retention, border molding, diagnosis, and treatment planning, and the meticulous attention to detail required throughout the treatment course of these alternative modalities. Indications, advantages, and limitations are also presented. Although these alternatives are not routinely used in making complete dentures, they have been successfully used for the treatment of the edentulous patient. Alternatives serve as valuable prosthodontic treatment options that greatly enhance denture aesthetics, and should be considered for edentulous patients.
Key points
- •
The flangeless and palateless denture has been a controversial treatment modality because of the uncertainties surrounding its effectiveness on retention.
- •
Retention, border molding, diagnosis, and treatment planning are important in this treatment.
- •
The scrupulous detail and meticulous attention to protocol throughout the course of treatment with the flangeless denture cannot be overemphasized.
- •
Although alternatives to traditional complete dentures are not routinely used to make complete dentures, they have been successfully used for the treatment of edentulous patients.
- •
Alternatives to traditional complete dentures provide valuable prosthodontic treatment that should be considered in treating select edentulous patients.
Introduction
Alternative designs in traditional complete denture therapy have been controversial because of the uncertainties surrounding the effectiveness of retention of the prosthesis. The importance of retention for a maxillary complete denture has been well recognized in the literature. As early as the mid-twentieth century, crucial aspects of retention including atmospheric pressure, intimate tissue contact, and peripheral seal were identified.
Hardy and Kapur and others reported on the posterior palatal seal and its advantages related to placement and location. More recent publications have discussed specifics of the palatal seal such as clinical determination, location, adaptation, anatomic structures, and the value of border molding to create a retentive seal. Border molding in the fabrication of complete dentures has been described by several investigators, but the question remains as to how much a limited flange or a denture flange that is not border molded in the anterior vestibule truly affects the seal.
The purpose of this article is to help answer this question through a literature update on specific alternative prostheses, and to show how these alternatives are effectively used to treat edentulous patients ( Boxes 1 and 2 ).
-
1950s
-
Stamoulis: atmospheric pressure, intimate tissue contact, peripheral seal
-
Hardy: Posterior palatal seal; advantages, placement, location
-
-
1960s
-
Laney, Gonzalez: palatal relief and posterior palatal seal
-
-
1970s
-
Silverman: dimensions and displacement of posterior palatal seal
-
-
1980s
-
Ettinger: posterior palatal seal, a review
-
Calomeni: posterior palatal seal, location and preparation
-
-
1990s
-
Sykora: adaptation and shape
-
-
2000s
-
Kim: relining and dimensional accuracy
-
Rashedi: current concepts for determination
-
-
2010s
-
Perry: anatomy and physiology
-
-
1700s: porcelain teeth
-
1800s: vulcanite
-
1930s: acrylic resin
-
1940s: autopolymerizing acrylic resin
-
Flangeless denture introduced in PubMed: 1965, 1980, 2002
-
Future developments with digital dentures
Introduction
Alternative designs in traditional complete denture therapy have been controversial because of the uncertainties surrounding the effectiveness of retention of the prosthesis. The importance of retention for a maxillary complete denture has been well recognized in the literature. As early as the mid-twentieth century, crucial aspects of retention including atmospheric pressure, intimate tissue contact, and peripheral seal were identified.
Hardy and Kapur and others reported on the posterior palatal seal and its advantages related to placement and location. More recent publications have discussed specifics of the palatal seal such as clinical determination, location, adaptation, anatomic structures, and the value of border molding to create a retentive seal. Border molding in the fabrication of complete dentures has been described by several investigators, but the question remains as to how much a limited flange or a denture flange that is not border molded in the anterior vestibule truly affects the seal.
The purpose of this article is to help answer this question through a literature update on specific alternative prostheses, and to show how these alternatives are effectively used to treat edentulous patients ( Boxes 1 and 2 ).
-
1950s
-
Stamoulis: atmospheric pressure, intimate tissue contact, peripheral seal
-
Hardy: Posterior palatal seal; advantages, placement, location
-
-
1960s
-
Laney, Gonzalez: palatal relief and posterior palatal seal
-
-
1970s
-
Silverman: dimensions and displacement of posterior palatal seal
-
-
1980s
-
Ettinger: posterior palatal seal, a review
-
Calomeni: posterior palatal seal, location and preparation
-
-
1990s
-
Sykora: adaptation and shape
-
-
2000s
-
Kim: relining and dimensional accuracy
-
Rashedi: current concepts for determination
-
-
2010s
-
Perry: anatomy and physiology
-
-
1700s: porcelain teeth
-
1800s: vulcanite
-
1930s: acrylic resin
-
1940s: autopolymerizing acrylic resin
-
Flangeless denture introduced in PubMed: 1965, 1980, 2002
-
Future developments with digital dentures
Modified palateless and flangeless removable prosthesis
After World War II, the evolution of autopolymerizing resins allowed the repair and modification of complete dentures and removable partial dentures without cumbersome processing techniques. Depending on the number and position of remaining teeth, a removable prosthesis can be made palateless. Removable partial dentures (RPDs) have been used for many years with flangeless tooth replacements.
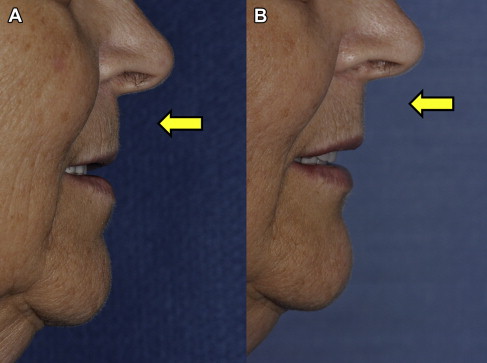
A key indication for a modified extension of prosthesis is when a labial flange is not needed because there is sufficient bone and lip support. In these instances, adding a buccal flange can distort the facial support and muscles of facial expression, limit function, and compromise aesthetics.
RPDs are designed with metal bases and reinforced acrylic pontics, tube teeth, and/or braided posts that typically do not incorporate a denture base flange; the denture teeth are set directly against the residual alveolar ridge or are placed directly on the metal base. In essence, there is no flange because the physiologic function and residual ridge does not require any additional support.
In these scenarios, the length of artificial teeth depends on the amount of existing interocclusal space. The width of artificial teeth varies from the perspective of facial/lip support.
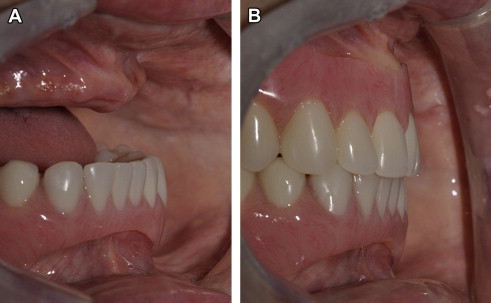
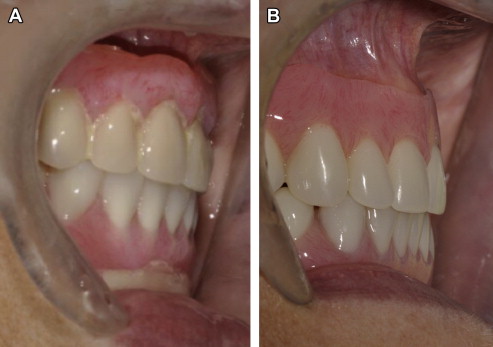
The tooth position must support the movement of the lips and facial muscles during normal movements of facial expression. The basic rules of aesthetics must be followed ( Figs. 1 and 2 ).
Diagnosis and treatment planning
Diagnosis and careful treatment planning is essential and vital to a successful outcome. The American College of Prosthodontists categorizes the severity of different oral entities in the Prosthodontic Diagnostic Index classification system.
Use of a diagnostic-driven evaluation includes the following: psychological classification, frena and muscle attachments, tongue position, sublingual fold, tori, ridge relation, lateral throat form, palatal form, soft-tissue quality of the palate, and bony undercuts.
As standard protocol for complete denture fabrication, the initial interview provides the dentist an opportunity to get to know the patient and identify his or her chief concerns. Treatment expectations can be determined by both patient and dentist.
The health history includes, but is not limited to, review of past medical conditions, systems review, allergies, and current medications, all of which are mandatory elements for each patient needing prosthodontic care. The dental history should include how, why, and when the teeth were lost; whether the patient has had previous experience with a removable partial denture or complete denture prosthesis; and the patient’s prosthetic experience with or without a flange. A preexisting prosthesis allows the dentist to evaluate the denture and flanges, and to assess patient function with the preexisting prosthesis.
As part of standard protocol, a thorough clinical and radiographic examination is also included in the fabrication of complete denture prosthesis to obtain diagnostic data in formulating a treatment plan. Radiographs may show the size and trabecular pattern of the bone and position of the genial tubercles, sinuses, and mental foramen. In addition, any radiographic evidence of abnormality, residual teeth, and root tips is documented and addressed. Clinical examination often reveals anterior bony undercuts that pose unusual difficulties in complete denture construction. In fabrication of a maxillary complete denture, it is not unusual to see a prominent maxillary residual ridge with a severe anterior labial undercut.
The maxilla often presents with a protruding trajectory before any tooth extraction, producing the appearance of a protruding upper lip. The trajectory of the premaxilla is generally due to loss of support of posterior dentition, driving the mandibular incisors against the lingual aspects of the maxillary anterior teeth.
When the mandibular anterior teeth are in stable solid Type 1 bone and the maxillary anterior teeth are surrounded by Type 2 to 3 bone, the maxillary anterior teeth are generally displaced buccal to their original position based on general occlusal function. Aesthetically, on extraction of the buccally displaced maxillary anterior teeth, the residual ridge is already in position to support the upper lip.
In addition, with osseous bone-graft procedures becoming more of a standard of care in immediate extraction sites, loss of the remaining maxillary alveolar ridge is minimized. If a denture base extension is placed in the premaxilla, two-thirds of the upper lip will be severely distorted from the base of the nose to the edge of the upper lip, specifically the wet-dry line.
Assuming the premaxilla buccal undercut does not require preprosthetic surgery, the flangeless maxillary complete denture is indicated to meet aesthetic requirements and ideal support of the upper lip. By maintaining undercuts in the premaxilla, additional retention is potentially available. Undercuts of the residual alveolar maxillary ridge should be scrutinized carefully, and not removed indiscriminately ( Fig. 3 ).