To achieve optimum occlusal and facial results in a patient with high-angle maxillary protrusion, it is important to move Point A back with retraction of the anterior teeth and prevent clockwise rotation of the mandible through good vertical control. A woman, aged 42 years 5 months, with a protrusive profile sought lingual orthodontic treatment. She had a skeletal Class II high-angle pattern with maxillary protrusion and mandibular retrusion. The extraction of the 4 first premolars was indicated to correct the problems. The vertical bowing effect, a side effect known to occur with conventional lingual bracket systems owing to torque loss, would preclude adequate retraction of Point A and compromise the facial results. To prevent this issue, a fully customized lingual bracket system with vertical slots for the anterior teeth using ribbon-wise archwires was selected. A midpalatal miniscrew was used to prevent molar extrusion. As a result, the bodily retraction of the maxillary incisors and Point A was achieved, obtaining an attractive facial profile.
Highlights
- •
Ribbon-wise wire with custom lingual brackets prevented maxillary vertical bowing.
- •
A midpalatal miniscrew prevented molar extrusion.
- •
Palatal arch controlled clockwise rotation of the mandible.
- •
Retraction of maxillary incisors and Point A contributed to an attractive profile.
A main goal in the treatment of maxillary protrusion with a retruded mandible and protruded lips is to improve the facial profile as well as the occlusal functionality. For this purpose, maximum retraction of the anterior teeth is required, which in turn necessitates the prevention of mesial movement of the posterior teeth into the extraction spaces through effective anchorage control and the establishment of proper buccopalatal and lingual torque of the anterior teeth during their retraction. This can be accomplished by fully uprighting the mandibular anterior teeth until there is no residual proclination. This is followed by bodily retraction of the maxillary anterior teeth. When conventional lingual bracket systems are used, there is a tendency for excessive lingual tipping (also referred to as “rabbiting”) of the maxillary anterior teeth.
Furthermore, high-angle patients are prone to molar extrusion and clockwise rotation of the mandible during treatment. These changes are known to cause downward and posterior movements of the chin, compromising facial esthetics. Vertical control therefore holds the key to successful treatment of these patients.
This article describes an adult with high-angle maxillary protrusion and a retruded mandible who was successfully treated with a fully customized lingual bracket system combined with a midpalatal miniscrew for controlling anchorage, anterior torque, and vertical dimensions.
Diagnosis and etiology
A woman, aged 42 years 5 months, was referred from her general dentist with the main complaints of poor facial appearance, protruding maxillary front teeth, and crowded mandibular front teeth.
During the clinical evaluation, no facial asymmetry was noted. The patient had a convex profile, mild maxillary protrusion, pronounced mandibular retrusion, lip incompetence, and severe mentalis strain on lip closure.
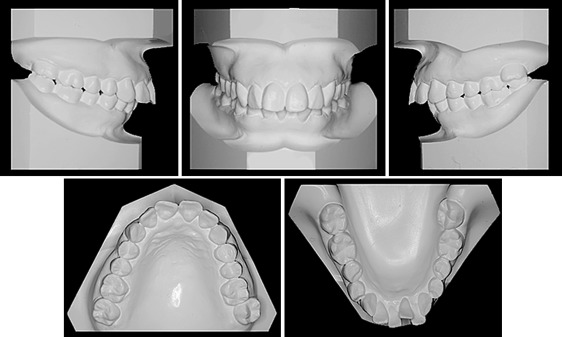
The intraoral findings showed that the maxillary and mandibular anterior teeth were crowded and protruded. A scissors-bite was observed in the left molar area with a buccally inclined maxillary second molar and a lingually inclined mandibular second molar. The maxillary left canine was nonvital with discoloration to the crown. The patient showed an intermediate risk for caries and periodontal disease. The periodontal examination showed 6-mm deep pockets on the distal aspects of the mandibular right and left second molars and bleeding on probing in the maxillary right premolar area. A 5-mm deep pocket was found in the mandibular right lateral incisor, with 2- to 3-mm pockets in the other areas ( Fig 1 ).

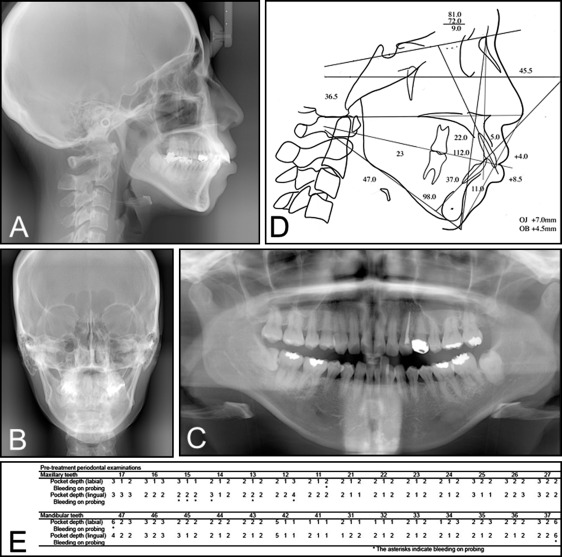
The patient’s molar correlation was Class I on the right side and end-on Class II on the left side. Overjet was 7.0 mm, and overbite was 4.5 mm. The sum of crown widths was 1 SD greater than normal for both arches. The maxillary and mandibular basal arch widths were −1 SD smaller, and the maxillary arch length was 2 SD larger than normal, indicating, from the study model findings, that both arches were constricted ( Fig 2 ).
The lateral cephalometric analysis showed skeletal maxillary protrusion and mandibular retrusion with SNA, SNB, and ANB angles of 81.0°, 72.0°, and 9.0°, respectively. The FMA was 36.5°, indicating a high-angle skeletal pattern. The maxillary incisors were protruded, and the mandibular incisors were proclined, with U1 to NA at 5.0 mm and 22.0°, L1 to NB at 11.0 mm and 37.0°, and an interincisal angle of 112.0° dentally. The upper and lower lips were at +4.0 and +8.5 mm, respectively, to the E-line from the soft tissue findings. The mandible was deviated to the right side relative to the facial midline, and the occlusal plane was canted, with the left side slightly lower than the right side. The maxillary and mandibular dental midlines were deviated by 1 and 2 mm, respectively, to the left side relative to the facial midline.
The roots of the 4 maxillary incisors appeared slightly shorter than normal. Eight teeth had fillings. The maxillary left canine was nonvital and had been treated endodontically. Both mandibular third molars were impacted; the right one was horizontally impacted. The maxillary third molars had previously been extracted ( Fig 3 ; Table ).
| Measurement | Pretreatment (age, 42 y 5 mo) | Posttreatment (age, 45 y 6 mo) | Retention 2 y 1 mo (age, 47 y 7 mo) |
|---|---|---|---|
| Skeletal | |||
| SNA (°) | 81.0 | 77.5 | 77.5 |
| SNB (°) | 72.0 | 71.5 | 71.5 |
| ANB (°) | 9.0 | 6.0 | 6.0 |
| Facial angle (°) | 83.0 | 82.5 | 81.0 |
| Y-axis (°) | 79.0 | 79.5 | 80.0 |
| FMA (°) | 36.5 | 37.0 | 37.0 |
| SN-MP (°) | 47.0 | 47.5 | 47.5 |
| Gonial angle (°) | 129.0 | 129.0 | 129.0 |
| NB to Pog (mm) | −1.0 | 0.0 | 0.0 |
| AO-BO (°) | 5.0 | 0.0 | 0.0 |
| Dental | |||
| OCC plane to SN (°) | 23.0 | 26.5 | 26.5 |
| U1 to SN (°) | 103.0 | 95.0 | 95.0 |
| IMPA (L1 to MP) | 98.0 | 84.0 | 82.0 |
| FMIA (°) | 45.5 | 59.0 | 61.0 |
| Interincisal angle (°) | 112.0 | 133.5 | 136.0 |
| Overjet (mm) | 7.0 | 3.0 | 5.0 |
| Overbite (mm) | 4.5 | 2.5 | 4.0 |
| U1 to NA (mm) | 5.0 | 3.0 | 3.0 |
| U1 to NA (°) | 22.0 | 18.5 | 18.0 |
| L1 to NB (mm) | 11.0 | 8.0 | 8.0 |
| L1 to NB (°) | 37.0 | 22.0 | 20.0 |
| Soft tissue | |||
| E-line: upper (mm) | 4.0 | −2.5 | −2.0 |
| E-line: lower (mm) | 8.5 | 1.0 | 1.0 |
| Z angle (°) | 47.0 | 62.0 | 63.0 |
Treatment objectives
The patient was diagnosed with skeletal high-angle maxillary protrusion and mandibular retrusion with an Angle Class II Division 1 molar relationship, a scissors-bite involving the maxillary and mandibular left second molars, labioversion of the maxillary anterior teeth, and proclination and crowding of the mandibular incisors.
The level anchorage system, developed by Root, was used to set treatment targets, and a treatment plan and orthodontic mechanics were established based on the targets. Specific targets included reducing the ANB angle from +9.0° to +6.0°, U1 to NA from 5.0 to 2.0 mm, and L1 to NB from 11.0 to 8.0 mm. Premolar extraction alone was considered inadequate to achieve these targets.
Addressing the periodontal disease required the periodontist to provide oral hygiene instructions with motivation to maintain her oral hygiene as well as scaling and root planing of all teeth.
The final treatment plan included use of a midpalatal miniscrew and a customized lingual bracket appliance. Mandibular third molar extraction was required for anchorage preparation ( Fig 4 ).
Treatment objectives
The patient was diagnosed with skeletal high-angle maxillary protrusion and mandibular retrusion with an Angle Class II Division 1 molar relationship, a scissors-bite involving the maxillary and mandibular left second molars, labioversion of the maxillary anterior teeth, and proclination and crowding of the mandibular incisors.
The level anchorage system, developed by Root, was used to set treatment targets, and a treatment plan and orthodontic mechanics were established based on the targets. Specific targets included reducing the ANB angle from +9.0° to +6.0°, U1 to NA from 5.0 to 2.0 mm, and L1 to NB from 11.0 to 8.0 mm. Premolar extraction alone was considered inadequate to achieve these targets.
Addressing the periodontal disease required the periodontist to provide oral hygiene instructions with motivation to maintain her oral hygiene as well as scaling and root planing of all teeth.
The final treatment plan included use of a midpalatal miniscrew and a customized lingual bracket appliance. Mandibular third molar extraction was required for anchorage preparation ( Fig 4 ).

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


