A 23-year-old Mongolian woman came for a consultation with chief complaints of protrusive lips and a gummy smile. The clinical examination showed a convex profile, a protrusive maxilla, excessively proclined and extruded maxillary incisors, and a Class II Division 1 malocclusion. Temporary anchorage devices (TADs) in the posterior dental region were used as anchorage for the retraction and intrusion of her maxillary anterior teeth. Those appliances, combined with a compensatory curved maxillary archwire, eliminated the severe gummy smile and the protrusive profile, and corrected the molar relationship from Class II to Class I. With no extra temporary anchorage devices in the anterior region for intrusion, the treatment was workable and simple. The patient received a satisfactory occlusion and an attractive smile.
Temporary anchorage devices (TADs) have changed the conventional conception of anchorage control and biomechanics in orthodontics. They have replaced many traditional types of mechanics and simplified orthodontic treatment. In 1983, Creekmore and Eklund reported a patient with a deep overbite corrected with a Vitallium bone screw; it was the first report of the clinical use of TADs. Based upon the extensive applications of TADs, many appliances have been invented to solve orthodontic problems, such as a protrusive alveolus and a significant gummy smile. Gummy smile refers to excessive gingival display during full smile. The current opinion is that less than 2 mm of gingival exposure is more esthetic and youthful. Kim et al and Kim and Freitas introduced a Class II Division 2 patient treated with a segmental arch appliance with TADs, which corrected the excessive vertical growth of the maxillary anterior dentoalveolar complex and alleviated the gummy smile. Lin et al reported on 4 patients with gummy smiles treated by a combination of TADs and periodontal surgery without orthognathic surgery. But there has been no case report of TADs used in the treatment of a Class II Division 1 patient with a significant gummy smile.
In this case report, we aimed to introduce the treatment of a woman with a Class II Division 1 malocclusion. TADs with compensatory curved archwires corrected the patient’s protrusive profile and significant gummy smile.
Diagnosis and etiology
The patient, a 23-year-old Mongolian woman, had a convex profile and a Class II malocclusion. Her chief complaints were protrusive lips and a gummy smile.
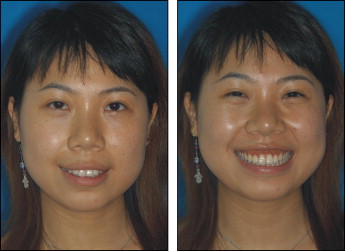
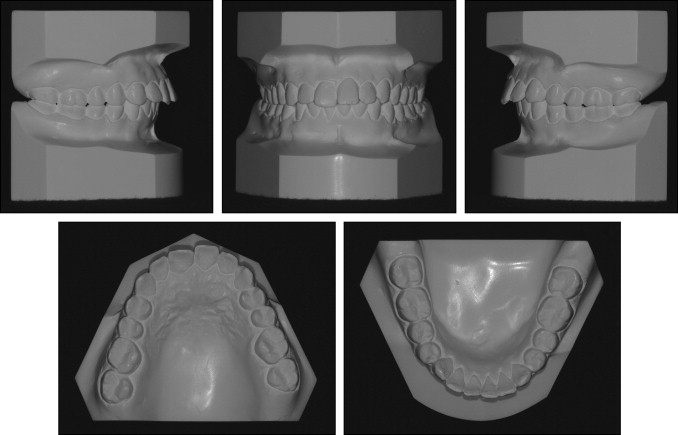
The photographs taken before treatment showed protrusive upper and lower lips, both of which exceeded the E-line and were strained on closure ( Fig 1 ). No anomaly was seen in the frontal facial photos, except that the patient was overly cautious about smiling naturally. When the patient relaxed, we took another smiling image ( Fig 2 ), which showed a significant gummy smile with more than 4 mm of gingival exposure in the incisor region. The photographs and pretreatment study casts ( Fig 3 ) exhibited excessively proclined and extruded maxillary incisors, and cusp-to-cusp canine and molar relationships with a deep overbite and overjet and no apparent crowding. The clinical examination suggested incisal and canine guidance without prematurity and shift. The patient had no temporomandibular joint symptoms. No deviation and pain during the border movement of the mandible were discovered. No short or hyperactive upper lip or vertical maxillary excess was found in our clinical examination that could be the etiology of the gummy smile.

A cephalogram ( Fig 4 , A ) and a panoramic radiograph ( Fig 4 , C ) were taken before treatment. The cephalometric analysis ( Table ) and the tracing ( Fig 4 , B ) demonstrated a Class II skeletal relationship (ANB, 6°) as a result of the retruded mandible. The A-point was in the normal range (SNA, 80°), and B-point was retruded (SNB, 74°). The angle between the maxillary incisors and the S-N plane was 112°, and the IMPA was 101°, which indicated that the protrusive profile was mainly caused by the proclined maxillary anterior teeth.

| Norm | Pretreatment | Posttreatment | Δ | |
|---|---|---|---|---|
| SNA (°) | 83.13 ± 3.6 | 80 | 79 | −1 |
| SNB (°) | 79.65 ± 3.2 | 74 | 74 | 0 |
| ANB (°) | 3.48 ± 1.69 | 6 | 5 | −1 |
| FMA (°) | 29 ± 5 | 34 | 36 | 2 |
| U1 to SN (°) | 102 ± 5.4 | 112 | 99 | −13 |
| IMPA (°) | 97 ± 6 | 101 | 92 | −9 |
| Interincisal angle (°) | 126.96 ± 8.54 | 105 | 124 | 19 |
Treatment objectives
The treatment objectives were to create a satisfactory occlusion with a Class I molar relationship and normalize overjet and overbite. Retraction and intrusion of the maxillary anterior teeth were indicated to reduce the exposure of the gingiva and the protrusive profile. Simultaneously, extrusion of the posterior teeth would be limited to prevent a clockwise rotation of the mandible and an increase in lower facial height.
Treatment objectives
The treatment objectives were to create a satisfactory occlusion with a Class I molar relationship and normalize overjet and overbite. Retraction and intrusion of the maxillary anterior teeth were indicated to reduce the exposure of the gingiva and the protrusive profile. Simultaneously, extrusion of the posterior teeth would be limited to prevent a clockwise rotation of the mandible and an increase in lower facial height.
Treatment alternatives
Three alternatives were presented to the patient.
- 1.
Combined surgical and orthodontic treatment to harmonize the molar relationship with extraction of premolars in both the maxilla and the mandible. Orthognathic surgery could be used to elevate and retrude the anterior maxillary dentoalveolar part to eliminate the gummy smile and improve the profile. Advancement genioplasty could be used to camouflage the retruded mandible and improve the profile.
- 2.
Harmonize the molar relationship and retract the anterior teeth by extracting the maxillary first premolars and the mandibular second premolars. Use TADs to provide absolute anchorage for maximum retraction of the proclined maxillary teeth and maxillary incisor intrusion to eliminate the gummy smile. The disadvantage was that the retruded mandible would not be corrected.
- 3.
Extract the maxillary first premolars and the mandibular second premolars, and use J-hook headgear as anchorage for retraction and intrusion. The disadvantage was that the effect of this treatment depended on the patient’s cooperation.
After we discussed these alternatives with the patient, she chose the second option. She considered the improvement from orthognathic surgery not worth the additional cost and risk, and the headgear was unacceptable.
Treatment progress
Orthodontic treatment began on February 28, 2006, and lasted for 38 months. Before bracket bonding, the maxillary first premolars and mandibular second premolars were extracted. Two mini-implants (1.6 × 9 mm, Aarhus, Medicon, Tuttlingen, Germany) were placed between the roots of the maxillary second premolars and first molars, 3 mm occlusally to the buccal frenum.
Preadjusted 0.022-in brackets (Shiye, Hangzhou, China) were bonded to all teeth. With sequential nickel-titanium archwires, alignment and leveling were achieved in 9 months. Then, 0.018 × 0.025-in stainless steel wires were placed in both dental arches. The maxillary wire had a 5-mm compensating curve of Spee. Nickel-titanium closed-coil springs and Class II elastics were used for space closure and mesial mandibular molar movement ( Fig 5 , A ). In the 20th month of treatment, the mandibular space was closed, and the first molars were in a Class I relationship. Further maxillary retraction was achieved by nickel-titanium closed coil springs on the TADs ( Fig 5 , B ). After 4 months of retraction of the maxilla, both overbite and overjet were reduced. No Class II elastics were used during the final maxillary retraction. At the third stage, the second molars were bonded, and intermaxillary elastics were applied with 0.018-in stainless steel wires in the brackets for better interdigitation of the occlusion ( Fig 5 , C ).





