Chapter 9
Surgical vs. Non-surgical Treatment of Periodontitis
INTRODUCTION
The goal of periodontal therapy can be defined as “to arrest the inflammatory disease process by removal of the subgingival biofilm and establish a local environment and microflora compatible with periodontal health” (Heitz-Mayfield, 2005). Biofilm can be removed and a favorable local environment can be established with non-surgical mechanical debridement and/or surgical debridement. This may be supplemented by local or systemic antibiotic or antiseptic modalities. Non-surgical and surgical therapies as well as adjunctive pharmacotherapies are described elsewhere in this volume. This chapter focuses on the issues relating to the relative effectiveness of non-surgical vs. surgical periodontal therapy.
It is generally accepted that mechanical debridement is at the core of any periodontal therapy (Van Dyke and Serhan, 2003). However, it should be noted that this view has been challenged (Mombelli, 2006), and may well change in the future as we gain a better understanding of the mechanisms underpinning the pathogenesis of periodontitis. (Van Dyke, 2007). Nevertheless, the question of whether mechanical debridement should be carried out using non-surgical or surgical techniques is obviously a very important one in clinical periodontology, and consequently has been studied and debated for decades. To date, a total of three systematic reviews/meta-analyses evaluating the relative effectiveness of non-surgical vs. surgical periodontal therapy have been published. This illustrates the importance of the clinical question and is also a reflection of the fact that a relatively large number of clinical trials have been conducted to investigate it.
EVIDENCE-BASED OUTCOMES
One of the first systematic reviews/meta-analyses published in the periodontal literature addressed the question of the relative effectiveness of surgical vs. non-surgical methods of treatment for periodontal disease (Antczak-Bouckoms et al., 1993). This review identified five studies that described similar treatment comparisons that were suitable for meta-analysis. The main conclusions of the study were that the relative effectiveness of surgical vs. non-surgical therapy depends on the initial, pre-surgical level of disease severity as measured by probing depth and on the outcome measure chosen (probing depth reduction vs. clinical attachment levels). For all levels of initial disease, surgical therapy results in greater pocket depth reduction compared to non-surgical therapy. However, the differences between surgical and non-surgical therapy in terms of mean probing depth reductions were generally around 0.5 mm or less. Furthermore, there was some evidence that the advantages of surgical therapy with regard to probing depth reduction became smaller with increased length of follow-up time (up to six years). For initially shallow and moderately deep pockets (up to 6 mm), non-surgical therapy results in better average outcomes in terms of clinical attachment levels, while surgical therapy performs better in initially deep pockets (greater than 6 mm probing depth). Again, the mean differences between treatment modalities were relatively small.
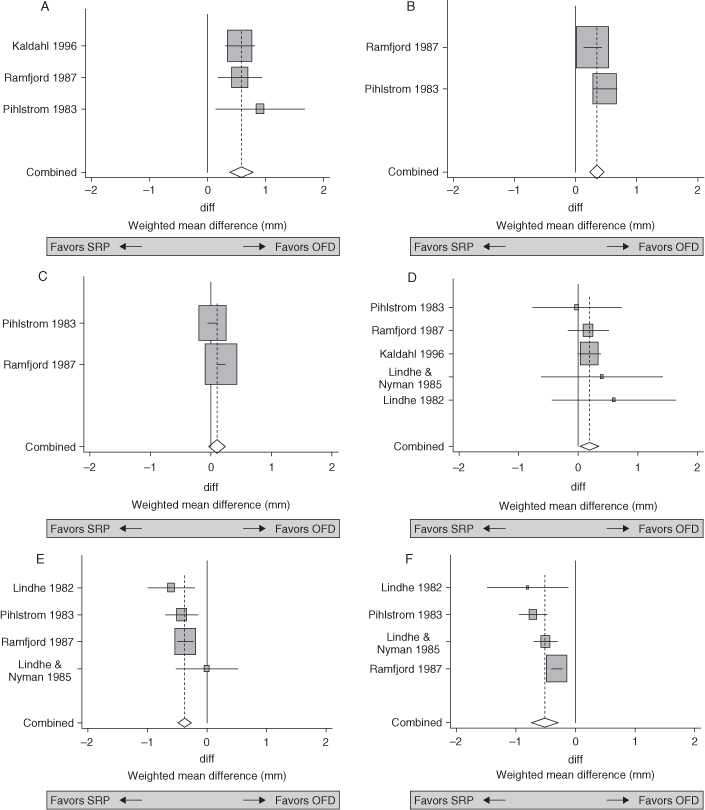
Two further systematic reviews/meta-analyses have been published since then (Heitz-Mayfield et al., 2002; Hung and Douglass, 2002), and the overall results are, perhaps not surprisingly, consistent with the first meta-analysis published by Antczak-Bouckoms et al. (Antczak-Bouckoms et al. 1993). A further review paper attempts to reconcile the minor differences between the results of the three published systematic reviews (Heitz-Mayfield, 2005). Figure 9.1 shows the results of the systematic review by Heitz-Mayfield (Heitz-Mayfield et al., 2002) for both probing depth reduction and clinical attachment levels as a function of initial probing depth. Although studies have suggested that non-surgical therapy has better outcomes in anterior teeth, this systematic review found similar relative effectiveness of non-surgical vs. surgical therapy in molar vs. non-molar teeth (Heitz-Mayfield et al., 2002).
Notwithstanding these limitations, the conclusions to be drawn from the available evidence are seemingly straightforward in that surgical therapy is the therapy of choice in severe disease (initial probing depths 7+ mm) or if the goal is probing depth reduction.
AUTHOR’S VIEWS/COMMENTS
As stated above, the goal of periodontal therapy may be defined as “to arrest the inflammatory disease process by removal of the subgingival biofilm and establish a local environment and microflora compatible with periodontal health” (Heitz-Mayfield, 2005). While this is a sensible definition in light of our current understanding of the pathogenesis of periodontitis, it does not lend itself to the assessment of success or failure of any periodontal intervention.
Figure 9.1. A, Forest plot of studies investigating the difference in probing depth change between open flap debridement (OFD) and scaling and root planing (SRP) at sites with initial PPD >6 mm. The rectangles represent the individual results for each study, in this case the weighted mean difference (WMD) in mm between open flap debridement vs. scaling and root planing. The size of the rectangle represents the weighting given to the study in the meta-analysis and is directly related to the precision of the study. The horizontal line extending from each square represents the 95% confidence interval (95% CI). The diamond at the bottom is the pooled value from the meta-analysis. The center of the diamond is the summary value and the horizontal points represent the 95% CI. When the diamond is to the left of the zero line the outcome is in favor of scaling and root planing. When the diamond is to the right of the zero line the outcome is in favor of open flap surgery. This analysis shows a 0.58-mm greater pocket depth reduction for surgery than scaling and root planing (95% CI: 0.38, 0.79, P < 0.001). B, Difference in the PPD change between OFD and SRP at sites with initial PPD: 4 mm to 6 mm. Fixed effects forest plot. C, Difference in the PPD change between OFD and SRP at sites with initial PPD 1 mm to 3 mm. Random effects forest plot. D, Difference in the CAL change between OFD and SRP at sites with initial PPD: >6 mm. Fixed effects forest plot. E, Difference in the CAL change between OFD and SRP at sites with initial PPD 4 mm to 6 mm. Fixed effects forest plot. F, Difference in the CAL change between OFD and SRP at sites with initial PPD 1 mm to 3 mm. Random effects forest plot. Reprinted from Heitz-Mayfield, 2005 with permission.
In terms of objective clinical periodontal outcomes, we may define the goals of periodontal therapy to be—at least in the short-term—the reduction or elimination of periodontal pockets and the pr/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


