Q. 2. Describe the radiolucent and radiopaque anatomic landmarks seen on the IOPA radiographs of mandible.
Ans. Normal anatomical landmarks seen on the mandibularperiapical radiographs are classified as:
A.
Radiolucent Landmarks of Mandible
ix. Periodontal ligament space.
• It is present below the roots of first and second premolars. Usually it is corticated.
• The shape of the foramen may vary from round to oblong and the size may vary from 1mm to 0.5 mm.
• It is only visible in lateral jaw films. As a small rounded or funnel-shaped black shadow over the ramus of mandible.
• It commences from mandibular foramen in the ascending ramus and appears as a radiolucent area covered superiorly and inferiorly by radiopaque margin.
• Position of canal varies, usually it lies below the roots of the molars and little distance below the bicuspids. Sometimes the apices of the molars may appear to be superimposed over the canals. Anatomically, the canal lies buccal to the molars and premolars.
• The mental fossa is a depression found on the labial aspect of the mandible on the anterior region.
• This is seen as a radiolucent area, only in lateral jaw films, as a broad dark area extending vertically on ramus. It is caused by patients swallowing when the film is being exposed.
• The submandibular fossa or the mandibular fossa or submaxillary fossa is a scooped-out, depressed area of bone located on the internal surface of the mandible inferior to the mylohyoid ridge.
• On a mandibular periapical radiograph, the submandibular fossa appears as a radiolucent area in the molar region below the mylohyoid ridge.
vii. Nutrient canals or interdental canals
• The nutrient canals are often seen in mandibular periapical radiographs as tube-like passage ways that carry neurovascular bundle in the jaw bones and supply the teeth and gingival tissues.
• On a mandibular periapical radiograph, nutrient canals appear as vertical radiolucent lines. They are readily seen in areas of thin bone and they may be more prominent in the edentulous mandible.
• Width of nutrient canal may vary from 100 micron to 1mm. Margins of the canal may reveal a thin white cortical plate, which may be slightly irregular.
B. Radiopaque landmarks of mandible
vi. Inferior border of the mandible
• They are usually seen in occlusal films and are four in number, two on either side of the median line on internal surface of mandibular incisors.
• They appear as a white ring with a dark centre immediately beneath and between lower central incisors.
• A dark white ridge extending from symphysis to the bicuspid region. Sometimes superimposed by apices of lower anterior teeth.
• This appears as a white line starting from lower border of symphysis and continuing upwards in the molar region towards ramus. Sometimes overlaps the molar apices.
• The external oblique ridge is a linear prominence of bone located on the external surface of the body of the mandible.
• White line on the anterior portion of ascending ramus. Sometimes it over shadows the roots of the molars.
• The internal oblique ridge is a linear prominence of bone located on the internal surface of the mandible that extends downward and forward from the ramus. It may end in the region of the mandibular third molar or it may continue as the mylohyoid ridge.
• On a mandibular periapical radiograph, it appears as a radiopaque band that extends downward and forward from the ramus.
vi. Inferior border of mandible
• It appears as a heavy white line on the radiograph. This is seen on IOPA whenever increased negative angulation is given in mandibular posterior radiography.
• Enamel is the densest structure found in the human body. It is the outer most radiopaque layer of the crown of a tooth.
• Dentine is found beneath the enamel layer of a tooth surrounding the pulp cavity. It appears radiopaque and makes up most of the tooth structure, but is not as radiopaque as enamel.
• Cementum is found beneath the dentine layer of a root surrounding the pulp cavity. It appears radiopaque and makes up most of the root structure, but is not as radiopaque as dentine.
• The lamina dura is the wall of the tooth socket that surrounds the root of a tooth and is made up of dense cortical bone.
• On a dental radiograph, the lamina dura appears as a dense radiopaque line that surrounds the root of a tooth.
• It is the most coronal portion of the alveolar bone found between the teeth. The alveolar crest is made up of dense cortical bone and is continuous with the lamina dura.
• On a dental radiograph, the alveolar crest appears radiopaque and is typically located 1.5 to 2.0 mm below the junction of the crown and the root surfaces (CEJ).
Q. 3. Radiographic features of fibro-osseous lesions of the jaws.
Ans.
• The fibro-osseous lesions are a diverse group of conditions. A common feature of all these lesions is that, there is replacement of the normal bone by a tissue composed of collagen fibres and fibroblasts that contain varying amounts of mineralized substances that may be either osseous in nature, cementum-like, or combination.
• The radiographic appearance of these lesions is also variable, either as diffuse, ground-glass appearance or well-defined cystic areas that may be radiolucent or containing varying amounts of calcified material.
• There is no acceptable classification for these lesions.
• A simple way of classifying the fibro-osseous lesions is to broadly divide these lesions into two groups based on their site of origin.
A. The fibro-osseous lesions of periodontal ligament origin are:
B. The fibro-osseous lesions originating from the medullary bone are:
Radiographic features of various fibro-osseous lesions of the jaws are as follows:
Fibrous dysplasia
• Fibrous dysplasia is a benign fibro-osseous lesion.
• Two types of fibrous dysplasia have been recognized, the monostotic or the solitary form and the polyostotic form.
• Fibrous dysplasia predominantly involves the maxilla than the mandible and is unilateral. The tumour usually manifests between 10 and 30 years of age. Often the posterior region of the jaw is involved.
• The radiographic appearance varies with the degree of maturation and the stage of the lesion.
• In lesions with more fibrous tissue, it may be radiolucency either unilocular or multilocular.
• Lesions with osseous tissue have a mottled appearance. Lesions with excessive osseous tissue appear radiopaque.
• The typical radiographic appearance is termed as ‘ground-glass’ or ‘orange-peel’ appearance. Usually the lesion is well-circumscribed.
Ossifying fibroma
• Ossifying fibroma, a rare neoplasm, is also called as fibro-osteoma.
• It is an encapsulated lesion within which the highly cellular fibrous tissue undergoes calcification.
• It usually affects young adults. Females have a slightly greater predilection. The lesion is slow-grow i ng and causes displacement of the teeth. Usually it involves the mandible.
• Radiographic findings depend on the stage of development of the lesion. It may either appear radiolucent or multiple radiopaque foci may be seen within the radiolucency.
• Eventually these foci coalesce together. Borders of the lesion are well-defined, often showing radiolucent ring suggestive of fibrous capsule. There may be displacement of the teeth.
Periapical cemental dysplasia
• Periapical cemental dysplasia was earlier called as cementoma.
• It is also variously named as fibro-cementoma, sclerosing cementoma, periapical osteofibrosis, or periapical fibro-osteosis.
• It is considered as a reactive fibro-osseous lesion.
• The lesion usually occurs in the middle age and females are affected more than the males.
• The lesion usually occurs in the periapical region of the mandibular anterior teeth and the lesions may be multiple.
• The affected teeth are vital and it is an asymptom aticlesion and most often is detected during a routine radiographic examination.
• Radiographic appearance of the lesion depends on the stage of development of the lesion. Accordingly, it may be radiolucent (fibrous), mixed radiolucent-radiopaque (fibrous and calcified elements), or radiopaque (calcified stage). The margins of the lesion may be well-defined or ill-defined.
• Usually no treatment is required for periapical cemental dysplasia.
Florid cemento-osseous dysplasia
• Florid osseous dysplasia is also called as gigantiform cementoma, chronic sclerosing osteomyelitis, sclerosing osteitis, multiple enostosis, and sclerotic cemental mass.
• This lesion has a female predilection, usually occurring in the middle age. Both the jaws are usually involved simultaneously. Sometimes it occurs only in the mandible.
• Often the lesion does not cause any symptoms. Occasionally pain or swelling may be noted.
• Radiographically the lesion appears radiolucent with dense radiopaque masses within. It has a similarity to ‘cotton-wool’ appearance of Paget disease. Individual lesions often exhibit a cortical outline.
Cementoblastoma
• Cementoblastoma is a rare neoplasm originating in the periodontal ligament.
• Males have a greater predilection and usually occurs before 25 years of age.
• Most common in the mandible and it appears as a solitary lesion. The invol v ed tooth is vital.
• Radiographically it appears as a well-defined radiopacity at the apex of a premolar or molar. Usually the calcified mass shows radiolucent halo.
Cherubism
• Cherubism is characterized by bilateral benign, firm, painless swellings in the mandible, usually in the angle region.
• The lesion usually develops in the infancy and continues to grow causing greatest expansion in the first and second years after the onset. As the age advances the deformity becomes less obvious. The lesion has a familial tendency.
• The lesion has derived the name as the affected children have characteristic chubby, cherubic facial appearance.
• Typically, the affected individuals have ‘eyes raised to the heaven’ appearance, if the lesion involves the maxilla. The characteristic radiographic appearance is multiple cyst-like radiolucencies in the mandible. The lesions have multilocular appearance and the borders are well-defined.
• Cortical plate expansion is seen in the occlusal or PA views. Maxillary lesions project into the maxillary sinus.The developing tooth buds are usually displaced. There is usually premature exfoliation of the deciduous teeth.
Paget disease (Osteitis deformans)
• Paget disease was described as a clinical entity by Sir James Paget in 1877 and is characterized by abnormal bone destruction followed by bone formation involving several bones.
• Though this disease mainly affects the skull, the femur, the sacrum, and the pelvis, jaw involvement is rarely seen bilaterally.
• The disease usually occurs above 50 years of age. Males are affected more than the females.
• Symptoms of the lesion are bone pain, increased temperature, curvature of the spine, enlargement of the skull and facial bones and bone deformity. In dentulous patients there can be drifting of the teeth and malocclusion. Edentulous patients often complain of ill-fitting dentures.
• Serum alkaline phosphatase level is increased in these patients.
• Radiographic appearance of this lesion depends on the stage of formation. Accordingly, it may be radiolucency of granular or ‘ground-glass’ appearance or dense radiopaque or the so-called ‘cotton-wool’ appearance. In the skull, the early lesions are lytic and appear as multiple radiolucencies called osteoporosis circumscripta.
• The management of this lesion is done with calcitonin or sodium etidronate therapy. Surgery is indicated for cosmetic purposes.
Q. 4. Discuss the differential diagnosis of periapical radiolucencies.
Or
Describe in detail periapical radiolucent areas.
Ans.
Various periapical radiolucencies
• Periapical granulomas, cysts, and abscesses are common periapical radiolucencies that can be seen on dental radiographs.
• Because it is impossible to distinguish between these three periapical lesions based on their radiographic appearance, hence they should be referred to simply as ‘periapical radiolucencies.’
Periapical granuloma
• A periapical granuloma is a localized mass of chronically inflamed granulation tissue at the apex of a nonvital tooth.
• The periapical granuloma results from pulpal death and necrosis and is the most common sequelae of pulpitis (inflammation of the pulp).
• A periapical granuloma may give rise to a periapical cyst or periapical abscess.
• A tooth with a periapical granuloma is typically asymptomatic but has a previous history of prolonged sensitivity to heat or cold.
• On a dental radiograph, a periapical g ranuloma is initially seen as a widened periodontal ligament space at the root apex.
• With time, the widened periodontal ligament space enlarges and appears as a round or ovoid radiolucency.
• The lamina dura is not visible between the root apex and the apical lesion.
• Treatment for a periapical granuloma may include endodontic therapy or remo v al of the tooth with curetta g e of the apical region.
Periapical cyst
• A periapical cyst also known as a radicular cyst is a lesion that develops over a prolonged period.
• Cystic degeneration takes place within a periapical granuloma and results in a periapical cyst. The periapical cyst results from pulpal death and necrosis.
• Periapical cysts are the most common of all tooth-related cysts and comprise 50-70% of all cysts in the oral region.
• Periapical cysts are typically asymptomatic. On a dental radiograph, the typical periapical cyst appears as a round or ovoid radiolucency.
• Treatment may include endodontic therapy or extraction of the tooth as well as curettage of the apical region.
Periapical abscess
• The periapical abscess is a localized collection of pus in the periapical region of a tooth that results from pulpal death.
• Periapical abscesses may be acute or chronic. An acute periapical abscess has features of an acute pus-producing process and inflammation. The periapical abscess refers to a tooth with an infection in the pulp.
• An acute abscess may result from an acute inflammation of the pulp or an area of chronic infection, such as a periapical granuloma.
• A chronic periapical abscess has features of a long-standing, low-grade, pus-producing process.
• A chronic abscess may develop from an acute abscess or a periapical granuloma.
• An acute periapical abscess is painful; the pain may be intense, throbbing, and constant. The tooth is nonvital and is sensitive to pressure, percussion, and heat.
• Chronic periapical abscesses are usually asymptomatic because the pus drains through bone or the periodontal ligament space.
• With an acute periapical abscess, no radiographic change may be evident.
• Early radiographic changes include an increased widening of the periodontal ligament space.
• A chronic periapical abscess appears as a round or ovoid apical radiolucency with poorly defined margins.
• The lamina dura cannot be seen between the root apex and the radiolucent lesion.
• Treatment of the periapical abscess includes drainage and endodontic therapy or extraction.
Q. 5. Describe various radiopaque lesions at the root of mandibular premolar.
Ans.
Commonly occurring radiopaque lesions
B. Conditions of Variable Radiopacity Affecting the Bone
• Developmental exostoses including tori mandibular or palatal
• Inflammatory low-grade infections, sclerosing osteitis, and osteomyelitis
Periapical radiopacities
Condensing osteitis, sclerotic bone, and hypercementosis are a few of the common periapical radiopacities that can be seen on dental radiographs.
Condensing osteitis
• Condensing osteitis is also known as chronic focal sclerosing osteomyelitis and is a well-defined radiopacity that is seen below the apex of a nonvital tooth with a history of long-standing pulpitis.
• It is the most common periapical radiopacity observed in adults.
• The opacity represents a proliferation of periapical bone that is a result of a low-grade inflammation or mild irritation.
• The inflammation that stimulates condensing osteitis occurs in response to pulpal necrosis.
• The tooth most frequently involved is the mandibular first molar.
• It may vary in size and shape and does not appear to be attached to the tooth root.
• Teeth associated with condensing osteitis are non-vital and typically have a large carious lesion or large restoration.
• No treatment is necessary, because condensing osteitis is believed to represent a physiologic reaction of bone to inflammation.
Sclerotic bone
• Sclerotic bone also known as osteosclerosis or idiopathic periapical osteosclerosis is a well-defined radiopacity that is seen below the apices of vital, noncarious teeth.
• The cause of sclerotic bone is unknown; however, it is not believed to be associated with inflammation.
• The lesion is not attached to a tooth and varies in size and shape.
• The margins may appear smooth or irregular and diffuse. The borders are continuous with adjacent normal bone, and no radiolucent outline is seen.
• Sclerotic bone is asymptomatic and is usually discovered during routine radiographic examination.
Hypercementosis
• Hypercementosis is the excess deposition of cementum on root surfaces. Hypercementosis results from supraeruption, inflammation, or trauma; sometimes there is no obvious cause.
• On dental radiographs, hypercementosis is visible as an excess amount of cementum along all or part of a root surface.
• The apical area is most often affected and appears enlarged and bulbous.
• Root areas affected by hypercementosis are separated from periapical bone by a normal-appearing periodontal ligament space, the surrounding lamina dura appears normal as well.
• No signs or symptoms are associated with hypercementosis; most cases are discovered during routine radiographic examination.
• Teeth affected by hypercementosis are vital and do not require treatment.
Q. 6. Describe the radiographic appearance of different types of osteomyelitis of jaws.
Ans.
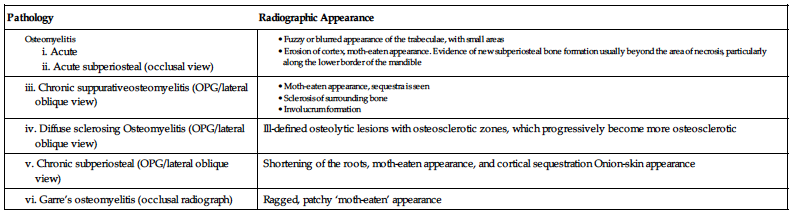
| Pathology | Radiographic Appearance |
| Ill-defined osteolytic lesions with osteosclerotic zones, which progressively become more osteosclerotic | |
| Shortening of the roots, moth-eaten appearance, and cortical sequestration Onion-skin appearance | |
| Ragged, patchy ‘moth-eaten’ appearance |
Q. 7. Name the malignant tumours of the jaws. Describe the radiographic appearance of carcinomas and sarcomas of the jaws.
Or
Describe briefly the characteristics of the malignant tumours of the jaws. Describe the radiographic appearance of the same.
Ans.
Characteristics of malignant lesion
• As a result of change in the nature of the lesion, the lesion grows and disrupts the normal anatomy there by causing obvious changes in the anatomic and radiographic picture of the tissue and the surrounding structures.
• The nature of the lesion, rate of its growth, and surrounding tissues are the factors, which ultimately elicit a radiographic picture specific to some extent to a particular lesion.
• The various features to be analysed and the reasons for those features being so specific have been discussed below in comparison to benign lesions.
• Benign lesions characteristically have well-defined borders, which is because of their inherent nature of being nonaggressive and slow growth.
• They grow gradually and hence have a rounded or oval extent.
• On the other hand, malignant lesions are aggressively expanding outwards and cause virtual erosion of the surrounding tissues. As a result of this the borders are irregular, ragged, and ill-defined. They have a mosaic form and blend with the normal tissue; for this reason radiographic extent of the lesion is difficult to define.
• Acute infection causes bony destruction, hence, results in sclerosing osteitis and a conforming radiographic picture of well-defined radiopaque margin.
• It is not only the radiograph or the clinical picture alone, which always is diagnostic of a pathology, but both act as adjuncts to each other.
• The benign lesions are slow growing and hence result in displacement of the surrounding structures like the cortical bone.
• With the elevation of the periosteum there is a stimulated formation of layers of reactive bone termed as onion-skin appearance as it appears like peels of onion on a radiograph.
• The growth pattern of malignant lesion is by destruction and invasion of the adjacent structures. Hence, the expansion of the lesion causes destruction of the cortex and drags the bony material along its path of expansion. It forms a trail of bone, hence, giving a typical picture of sunburst appearance.
• Depending upon the tissue involved, the radiodensity of the lesion is variable, e.g., an osteoma is a radiopaque lesion while a central haemangioma is radiolucent, both are benign.
• Malignant lesions such as carcinomas are radiolucent except in case of metastatic lesion, e.g., carcinoma of the prostrate gland.
• There is simultaneous resorption and deposition of bone in case of sarcomas, a feature diagnostic of sarcomas.
• Teeth are more calcified than the bone.
• When the lesion is expanding the response of the teeth is recorded in the following two ways:
• Usually the benign lesions are slow growing and they put slight persistent pressure on the teeth resulting in gradual displacement of the teeth.
• In malignant lesion, the rate of expansion of the lesion is reasonably high for the teeth to respond to the pressure.
• The roots are well within the border of the lesion, therefore, in malignant lesions there is a typical picture of floating teeth, more so, the teeth lie in their actual position.
• As far as resorption of roots is concerned, benign lesions cause resorption.
• In a malignant lesion, the contact period is relatively less, hence resorption is not a specific feature of a malignant lesion as in benign lesion.
• Since radiograph is a two-dimensional image of the tissues, hence, superimposition of various structures occur thereby making it difficult for the observer to analyse the extent of the features of the lesion. Radiographic exposure at two angulations can solve this problem to some extent.
• CT scan or computerized tomography is good answer to this problem.
• With CT scan, the invasion of the lesion into the soft tissue can also be analyzed.
Carcinomas
Squamous cell carcinoma
Aetiology
There is no specific aetiology but many factors have been accounted for:
Clinical features
• Occurs predominantly in men over 50 years of age.
• The most predominant site is that of posterolateral border of the tongue and lower lip, less frequently floor of mouth, alveolar mucosa, palate and buccal mucosa.
• Size and bony involvement: Osseous involvement is most frequently in third molar region of mandible where it is closest to the bone. Small lesions, which are less than 1.0 cm in diameter are generally asymptomatic. It is only when the lesion enlarges that there is pain, anaesthesia or swelling. With the gradual increase in size of the lesion, if lying close to the tooth there occur loosening of the tooth with some root resorption or at times leading to exfoliation.
• Further increase in size may lead to metastasis through the lymphatic channels to submental and submandibular lymph nodes.
Radiographic features
• It appears as a destructive lesion. There is gradual erosion of the bone resulting in ill-defined margins all along the tumour or at some specific points.
• In the mandible, gradual growth of the lesion may lead to complete erosion of the bone resulting in a pathological fracture.
• Usually a combination of postero-anterior view, occlusal view, and lateral oblique view are helpful in understanding the extent of the lesion and in the demonstration of such fractures.
• Usually the lesion has an irregular border but at times the border of the tumour is lined by a radiopaque margin as in condensing osteitis.
• Also, sometimes specks of radiopaque materials signifying pieces of left over bone by the rapidly advancing tumour (especially in central squamous cell carcinoma).
Management
Metastatic carcinoma
Clinical features
• Mandible is more susceptible for metastatic carcinoma than the maxilla.
• The most common site is premolar and molar region.
• Age varies from 40 to 60 years. Metastasis may occur from breasts, lungs, kidneys, prostrate glands, colon, testis, and stomach.
• Oral findings are usually the first indication of the disease.
• Only when the mandibular nerve is involved by the lesion, there is pain, paraesthesia or anaesthesia.
• The teeth may become loose or get exfoliated with occasional evidence of root resorption.
Radiographic features
Sarcomas
Osteosarcoma
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


