Q. 2. Define sialography and describe in detail the contrast media used in sialography.
Or
Define sialography. Give the ideal requirements of the contrast media used in sialography.
Ans. Sialography is a specialized radiographic view taken by introduction of the radiopaque dye into the ductal system of the major salivary glands, mainly parotid and submandibular.
This technique is used to examine the ductal and acinar systems of the major salivary glands. The sublingual and the minor glands cannot be studied obviously because of their small and numerous openings.
Contrast media
An ideal sialographic contrast media should have the following characteristics:
i. Physiological properties similar to that of saliva.
iii. Absence of local or systemic toxicity.
v. Satisfactory opacification.
vi. Low surface tension and low viscosity to allow easy filling of fine components of the ductal system.
vii. Easy elimination, but should be durable for sufficient time so as to permit time for satisfactory radiographs.
viii. Residual contrast media should be absorbed by the salivary gland and detoxified by the liver or excreted by the kidney.
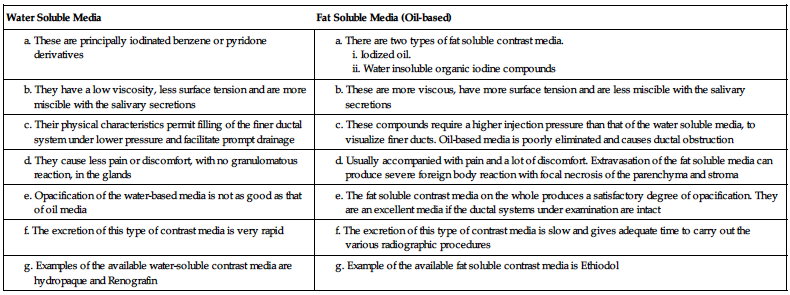
Two types of contrast media available are explained in the table below:
| Water Soluble Media | Fat Soluble Media (Oil-based) |
Q. 3. Describe sialography in detail and write briefly on its significance in various salivary gland disorders. Add a note on its interpretation in various diseases of salivary glands.
Ans.
• Sialography is a specialized radiographic view taken by introduction of the radiopaque dye into the ductal system of the major salivary glands, mainly parotid and submandibular.
• This technique is used to examine the ductal and acinar systems of the major salivary glands. The sublingual and the minor glands cannot be studied obviously because of their small and numerous openings.
Indications
i. Detection of calculus or calculi or foreign bodies and also ductal disorders of major salivary glands.
ii. Determination of the extent of destruction of the gland secondary to obstructing calculi or foreign bodies.
iii. To evaluate the extent of irreversible ductal damage caused by infection. This will help in deciding treatment plan whether a total excision of the gland or a simple lithotomy should be performed.
iv. Detection of fistulae, diverticula or strictures.
v. Determination and diagnosis of recurrent swellings and inflammatory processes.
vi. Demonstration of a tumour and the determination of its location, size, and origin.
vii. Determining outline of the plane of the facial nerve as a guide in planning a biopsy or dissection.
viii. Detection of residual stone or stones, residual tumour, fistula or stone retention cysts following surgical procedures.
ix. Sialography has also been employed as a therapeutic procedure because:
• The dilatation of the ductal system produced during the study may aid in the drainage of the ductal debris.
• A therapeutic effect is produced by the iodinated contrast media when injected into the ductal system.
• It may be used as a dilating procedure for mild ductal stenosis. For evaluation of diverticula, strictures, and fistula.
Contraindications
Armamentaria required
Procedure
• The parotid gland and submandibular glands are more readily studied using sialography.
• Before the passage of cannula, a lacrimal or periodontal probe is used to dilate the sphincter at the ductal orifice.
• Cannula is connected by extension tubing to a syringe containing contrast medium. Once the duct is cannulated, the injection of contrast medium is made with hand pressure. Patient may complain of mild pain during injection. A slow constant injection technique can accomplish complete ductal filling without patient discomfort.
• Patient sensation of glandular fullness is suggested by a sharp pain when the operator usually stops and proceeds for radiography.
Phases of sialography are as follows:
Appearance
Normal salivary glands have a leafless-tree appearance on sialograph.
II. Obstructive and inflammatory disorders
a. Sialolithiasis: It has a cigar- or oval-shaped radiopacity on sialogram.
b. Bacterial Sialadenitis: Ball-in-hand appearance.
c. Saccular dilatation of acini of the glands: Produces focal narrowing of duct.
d. Autoimmune sialadenitis: Sialography is helpful in diagnosis and staging of sialadenitis.
1) Early stage: Initiation of punctate and globular spherical collection of contrast medium evenly distributed.
2) During progression of disease: Collection of contrast agent greater than 2 mm and irregular in shape.
e. Sicca syndrome: Gives snowstorm or cherry blossom like appearance.
f. Sialectasis: Appearance of focal collection of contrast medium.
Interpretations of sialograph
• The sialographic appearance of the normal salivary glands is that of a leafless tree. This radiograph shows the main duct gradually going in secondary branches and then into tertiary branches.
Various sialographic findings are described below:
• Sialography is an invaluable asset in the diagnosis of neoplastic diseases of salivary gland origin.
• Since the benign tumour develops at the expense of normal glandular structure, the sialogram will often reflect its presence by revealing a filling defect, the latter being due to distortion and displacement of the normal duct system by the pressure of the expanding mass.
• A centrally located defect, devoid of ducts and surrounded by a whorl-like formation of ducts, is referred to as the ‘ball-in-hand’.
• The tumour with no ductal structures in its midst represents the ‘ball’ whereas the normal secondary and tertiary ducts that have been pushed to the periphery are supposedly the fingers and palm of the ‘hand’. This pattern may be visualized on lateral and/or anteroposterior films.
• The presence of localized puddling or widespread diffusion of the contrast medium throughout the gland parenchyma suggests the diagnosis of a malignant neo plastic disease.
• The invasive character of the malignant tumour leads to partial destruction of ducts, and as the sialographic solution reaches these regions, it escapes into the surrounding interstitial connective tissue, either accumulating in localized puddles or diffusing widely.
• Not all malignant tumours are portrayed in this manner. Occasionally, a malignant neoplasm gives the ‘ball-in-the hand’ pattern, since it, too, may manifest a tendency to encapsulation in spite of its infiltrative character.
• When dealing with a parotid gland tumour, an anteroposterior film may shed further light regarding its nature and more precise location. The parotid gland with its contained duct system may be displaced laterally away from the ramus of the mandible. Thus, the exact location of the lesion is noted and its size may even be precisely measured.
• Displacement of Stensen’s or Wharton duct by the presence of a tumour may also be detected sialographically.
a. With forward displacement of the gland → buckling of the major duct is observed, with the posterior portion crowding upon its anterior segment.
b. Posterior glandular displacement results in the opposite effect → A distention and elongation of the major duct.
c. Inferior or superior gland displacement inevitably causes → a disturbance in the course of Stensen’s and Wharton ducts that may be visualized sialographically.
Q. 4. What is tomography and describe in detail computed tomography.
Ans.
• Tomography is a process by which an image layer of the body is produced, while the images of the structures above and below that layer are made invisible by blurring.
• In many cases a distinction can be made by choosing appropriate orientation of the patient, or otherwise it is necessary to use a technique known as ‘body section radiography’ or tomography’.
Tomography may be classified into three types:
Conventional tomography
• Tomography is a Greek word where tomo means ‘ slice’ and graph means ‘picture’, which was adopted in 1962 by the International Commission on Radiographic Units and measurements to describe all forms of body section radiography.
• Body section radiography is a special X-ray technique that enables visualization of a section of the patient’s anatomy by blurring regions above and below the section of interest.
• This is achieved by a synchronized movement of the film and the tube in opposite directions, about a fulcrum.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


