Chapter 8
Other diseases and disorders affecting the oral cavity
INTRODUCTION
Many disorders and diseases affect the oral cavity. This chapter explores those, other than gingivitis, periodontitis, caries, tooth surface loss and xerostomia, which the oral health educator (OHE) may encounter and includes their features, treatment and management. It includes certain systemic (whole body) conditions and diseases that can directly or indirectly affect the oral cavity.
PERIODONTAL ABSCESS
A periodontal abscess (Figure 8.1) is a localised collection of pus, also sometimes referred to as a lateral periodontal abscess, as it occurs on the side of the root or in the furcation (the division between two roots). It is usually, although not always, a development of advanced periodontitis.
Figure 8.1 Periodontal abscess (© John Wiley & Sons, Ltd 2003. Reproduced with permission from Reference 1)

Aetiology (causes)
A periodontal abscess usually develops from a periodontal pocket – as organisms invade tissues and the outlet is blocked by a foreign body or food debris. It can still occur if oral hygiene improves before adequate scaling has taken place to remove the organisms (gingival tissue tightens as hygiene improves and stops pus oozing from the pocket).
Clinical features
Clinical features of a periodontal abscess, which may subside and recur, include:
- Swelling (sometimes localised, sometimes the whole side of the face). This can also include localised swelling of lymph glands.
- Redness.
- Pain.
- Pus discharge (in later stages).
- Appears as a radiolucent (transparent) area on X-ray.
Treatment
Treatment depends on the severity of the periodontal abscess.
Short-term treatment includes:
- Hot saltwater mouth rinses.
- Antibiotics (often required).
- Drainage – through deep scaling or incision.
Long-term treatment includes:
- Regular deep scaling (ultrasonic scaler) and irrigation (chlorhexidine).
- Extraction (last resort).
APHTHOUS ULCERS (MINOR AND MAJOR)
A mouth ulcer (Figure 8.2) is a painful open sore caused by a breach in the oral epithelium. Ulcers can occur for no apparent reason, are not contagious and can affect the non-keratinised mucosa, lateral border of the tongue, floor of the mouth, buccal mucosa and the lips.
Figure 8.2 Mouth ulcer (apthous ulceration) (From Farthing, P. (2006) [2]. Reproduced with permission of John Wiley & Sons, Ltd)

Aetiology
The causes of mouth ulcers are not fully understood, but predisposing factors include:
- Trauma (e.g. from cheek biting, toothbrushing, hard foods).
- Orthodontic appliances.
- Inherited genetic susceptibility.
- Reaction to chemicals (e.g. sodium lauryl sulphate in toothpaste).
- Vitamin or mineral deficiency (B12, zinc, iron, folic acid).
- Hormonal (some women develop ulcers prior to menstruating).
- Gastrointestinal disease (e.g. Crohn’s disease, ulcerative colitis, coeliac disease).
- Cow’s milk allergy.
- Stress.
- Citrus fruits.
- Lack of sleep.
- Sudden weight loss.
- Immunodeficiency (e.g. HIV).
Clinical features
Minor aphthous ulcer
Clinical features of a minor aphthous ulcer include:
- Painful sore – a few millimetres in size. Red raised area around the border, with a white or grey centre.
- Circular or oval in shape.
- Can occur singularly or in clusters.
- Should heal after 7–14 days. If no improvement is seen after this time, the dentist should be consulted as this could be a sign of more serious disease, such as oral cancer or gastrointestinal disease.
Major aphthous ulcer
Clinical features of a major aphthous ulcer include:
- 0.5–1 cm or more in size.
- Irregular shape.
- Can take up to 4–6 weeks to heal and can leave scarring.
- Often multiple, they can occur on keratinised and non-keratinised surfaces – lips, cheeks and soft palate are common areas.
Treatment
There is no specific cure for major or minor aphthous ulcers, but patients can be advised on ways to alleviate the symptoms and pain as well as avoid known triggers:
- Use topical gels and sprays containing analgesics (painkillers) and local anaesthetic properties (e.g. Difflam™, Bonjela).
- Protection from secondary infection (consider chlorhexidine).
- Toothpaste free from sodium lauryl sulphate (e.g. Sensodyne® Pronamel™, Biotene®, bioxtra®).
- Avoid spicy, acidic or sharp foods.
- Control stress and get plenty of good quality sleep.
- A healthy well-balanced diet (see Chapter 9).
- Silver nitrate (this burns the top layer of the ulcer, which reduces pain and aids with healing).
- Zinc or vitamin B12 supplements.
- Orthodontic appliances (soft wax can be placed over the appliance where the ulcer forms).
- Herbal remedies and homeopathy – for example, aloe vera (in toothpaste), Feverfew and propolis ointment (see Chapter 19).
COLD SORES (HERPES LABIALIS)
Cold sores (Figure 8.3) are very common in the United Kingdom and most sufferers are infected in early childhood, often through close contact with a relative (kissing). When a small child is first infected, the disease can present as an acute and unpleasant illness (see Acute Herpetic Gingivostomatitis).
Figure 8.3 Cold sore (herpes labialis) (© Professor M.A.O. Lewis, Cardiff University. Reproduced with permission)

Aetiology
Cold sores are caused by an infection with the herpes simplex virus at nerve endings. The virus can live throughout the life of an individual and reactivates. Contact with others (usually mouth) leads to spread of virus.
Clinical features
Clinical features (and contagious stages) of cold sores include:
What reactivates the virus?
The virus is often reactivated by the following:
- Illness (e.g. cold, flu, AIDS).
- Emotional stress.
- Menstruation.
- Bright sunlight (which explains why some people develop cold sores while on holiday).
- Extreme cold weather.
- Fatigue and physical injury.
Treatment
Treatment of cold sores includes:
- Antiviral cream – should be applied at the initial tingling stage before clinical signs appear. Scratching or close contact with others (particularly young children) should be avoided.
- Severe cold sores can be treated using systemic antiviral drugs.
- Herbal remedies and homeopathy – for example, propolis ointment (see Chapter 19).
ACUTE HERPETIC GINGIVOSTOMATITIS
Acute herpetic gingivostomatitis (AHGS) (Figure 8.4), also known as primary gingival herpetic stomatitis, is how the herpes simplex virus can present in babies and small children, and it is occasionally seen in adults who have lowered immunity.
Figure 8.4 Acute herpetic gingivostomatitis (© John Wiley & Sons, Ltd 2003. Reproduced with permission from Reference 3)

Aetiology
AHGS is caused by infection with the herpes simplex virus.
Clinical features
The herpes simplex virus may be mild and produces few symptoms, or may be severe with widespread ulceration.
Clinical features of AHGS include:
- Small vesicles (blisters), which rupture and produce ulcers, appear in the mouth and/or throat.
- Sudden onset of feeling unwell and irritability.
- Dehydration (due to refusal to eat and drink).
- Dribbling – as too painful to swallow saliva.
- General malaise – fever, coated tongue, swollen tongue and foul breath.
Treatment
AHGS is treated as a flu-like illness, by:
- Rest.
- Frequent drinks, soft foods (infants may require hospital treatment to restore fluids if they refuse to drink).
- Mild analgesics.
- Chlorhexidine mouthwash (for adults).
- Gentle oral hygiene.
- Antiviral drugs (may be prescribed in severe cases).
TOOTH ANOMALIES
Hypodontia
Hypodontia is a congenital (from birth) disorder that describes a reduced number of teeth. It usually occurs in the permanent dentition and rarely in the deciduous dentition [4]. The teeth most commonly missing are lower third molars, upper lateral incisors and lower second premolars. Hypodontia can be hereditary, but can also occur for no apparent reason.
Anodontia
Anodontia is a congenital disorder that describes the total absence of teeth. It is rare and usually associated with the hereditary genetic condition hypohidrotic ectodermal dysplasia (a genetic defect in which patients have very few or no teeth, and an absence of hair and sweat glands) [4].
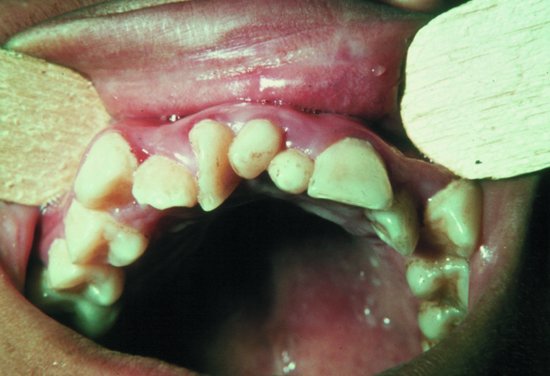
Hyperdontia
Hyperdontia is a congenital disorder in which the person has more teeth than normal. The extra teeth are called supernumerary teeth. They can occur anywhere in the mouth, but are most commonly found anteriorly in the maxilla and in the premolar region of the mandible. They are more common in the permanent dentition and in females and can cause crowding, prevent teeth erupting, the displacement of teeth and resorption if unerupted [4].
Supernumerary teeth are classified according to their morphology (shape), which are known as supplemental (including conical, tuberculate, molariform) and location (mesiodens, paramolar, distomolar).
The most common type of supernumerary teeth are mesiodens (Figure 8.5), which occur between the upper central incisors. Paramolars are found in addition to molars.
Figure 8.5 Two mesiodens in the midline between the upper central incisors (From Farthing, P. (2012) [5]. Reproduced with permission of John Wiley & Sons, Ltd)
Teeth size
Genetic factors can cause abnormalities in tooth size, causing them to be unusually large or small. The whole dentition is usually affected, but it occasionally affects just a few teeth. Peg-shaped upper lateral incisors can also herald a missing lateral on the opposite side.
Tooth morphology anomalies
Variations in morphology of the tooth root or crown are quite common. They may present as [4]:
- Double tooth (Figure 8.6) – where two teeth have fused together during development.
- Enamel pearls – nodules on the buccal root surface.
- Dens in dente – literally a tooth within a tooth.
- Dilaceration (disturbance in tooth shape) – caused by trauma to the developing tooth resulting in the root and crown being bent.
- Amelogenesis imperfecta – an inherited disorder, in which the enamel is poorly mineralised and defective resulting in soft, brittle and pitted enamel that can breakdown a/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


