Chapter 8
Extraction of Teeth
Extraction of teeth is one of the most common surgical procedures worldwide. It has a psychological impact on the patient, because the patient will be losing a tooth, and the associations the patient will have with such a procedure. The patient will also face another problem in that the loss of a tooth often requires a later replacement of the missing tooth. For this reason patient information and consent is very important. Moreover, extraction of teeth incorporates basic principles from physics, mechanics, and surgery, and the clinician should therefore fully understand and master the techniques of extraction.
Indications for Extraction
Although teeth in principle should be treated and maintained in the oral cavity as long as possible, provided they fulfill functional and esthetic criteria, it is sometimes inevitable that teeth have to be removed for various reasons. General indications for extractions, as listed in Box 8.1, are discussed under their respective headings; however, the decision to extract has to be made individually for each case.
Caries
When the tooth is subjected to severe caries with extensive loss of tooth substance that will not permit restorative procedures, it may sometimes be necessary to extract the tooth.
Periodontal Disease
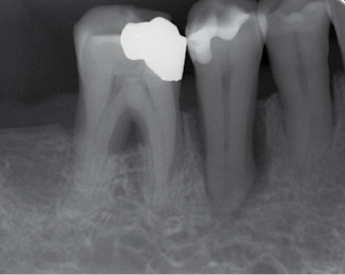
Periodontal disease should be treated as first alternative, but there are situations where severe periodontal disease can be an indication for extraction, especially when the prognosis is poor for periodontal treatment. Severe bone and attachment loss and irreversible tooth hypermobility may be an indication for extraction (Fig. 8.1). Long-standing, progressive periodontitis will result in alveolar bone loss. If implant treatment is going to be performed after extraction it is important not to wait too long before severely periodontally affected teeth are extracted. The severity of periodontal disease, long-term prognosis, and even cost/benefit aspects should be considered before making the decision.
Pulp Disease When Endodontic Treatment is Not Possible or Has Failed
Irreversible pulpitis, pulp necrosis or internal resorption of the root canal where endodontic procedures are not possible or have failed are sometimes other indications for tooth extraction. This could be because of obliterated root canals, canals that are not accessible due to root anatomy, or when a patient chooses not to undergo such treatment.
Pathologic Lesions in Relation to Teeth
Pathologic lesions associated with teeth, i.e. apical or juxtaradicular periodontitis, can usually be solved by endodontic treatment. If endodontic procedures are not possible, then extraction can be considered. If teeth compromise the surgical treatment of other pathologic lesions found in the tissues surrounding them, then extraction may be considered, e.g. in the treatment of osteomyelitis, or benign and malignant tumors of the jaw.
Crown and Root Fractures
Crown, crown-root, and root fractures after trauma can most often be successfully treated and extraction avoided. However, there are other situations where fractures of the crown and root do not allow successful restorative therapy and extraction is the only alternative (Fig. 8.2).

Malposition of Teeth
Although malposition of teeth is not an indication for extraction, there are situations where malposition is associated with other conditions such as trauma to soft tissue or blockage of eruption of adjacent teeth (Fig. 8.3). Another situation is when there is elongation of teeth due to the missing antagonist and where prosthetic rehabilitation is considered in the opposing jaw. The elongated tooth may then be considered for extraction.

Impacted Teeth
Impacted teeth do not always reach functional occlusion, often because of lack of space. These teeth should be investigated and considered for extraction if they present a potential for the development of pathology in the future. These could include the risk for root resorption of adjacent teeth, loss of bone around adjacent roots or development of other pathologic conditions such as cysts. Impacted third molars are the most common teeth considered for extraction. However, there must always be an indication if third molars are going to be removed and prophylactic removal of impacted third molars without pathology or symptom is not justified today. For more details regarding strategies for third molar extraction see Chapter 9.
Supernumerary Teeth
Supernumerary teeth that are potential sources for future pathology should sometimes be removed. However, supernumerary teeth without pathology do not have to be routinely removed (Fig. 8.4).

Orthodontic Indications
Extraction of teeth is sometimes required to create space in order to carry out planned orthodontic treatment. The most common teeth for extraction on orthodontic indications are premolars. The decision on which tooth/teeth are to be extracted is made by the orthodontist.
Before Prosthetic Procedures
Before prosthetic reconstructions is carried out it is sometimes necessary to extract teeth. Teeth could interfere with the proper placement of a fixed or removable prosthetic appliance and may then be extracted. For example, in the case of rehabilitation of a jaw with implants where there are only one or two incisors remaining that have a dubious prognosis, in some situations it may be better to be radical and extract the remaining teeth and perform a full arch implant-supported reconstruction.
Before Other Surgical Procedures
Sometimes teeth have to be removed prior to other surgical procedures. The most common indication in this regard is the removal of impacted molars prior to LeFort-I and sagittal split osteotomies. This is done if the teeth lie in the line of the planned osteotomies or increase the risk for other complications such as undesired fractures.
Before Radiation Therapy
Careful consideration should be given to patients who are to undergo radiation therapy due to tumors in the head and neck region. These extractions should preferably be carried out before radiation treatment is starting. Teeth associated with pathologic conditions such as periapical periodontitis should be considered either for swift endodontic procedures or extraction. A radical approach by extracting rather than choosing doubtful restorative treatment with less chance of successful outcome is recommended to avoid later complications in the irradiated bone. There is a high risk of osteoradionecrosis if extractions have to be carried out after radiation therapy, especially with high doses of radiation (>60 Gray). This risk persists throughout the life of the patient.
Before Bisphosphonate Therapy
Patients treated with bisphosphonates, especially those treated for malignancies with intravenous administration of bisphosphonates, run a high risk of osteonecrosis if extraction is carried out after bisphosphonate treatment has started. Like in irradiated patients, this risk persists throughout the life of the patient. For this reason dental examination and appropriate treatment shall always be taken into consideration when such bisphosphonate treatment is planned. Extractions should be carried out before bisphosphonate therapy is started. Teeth associated with pathologic conditions such as periapical periodontitis should be considered either for swift endodontic procedures or extraction. A radical approach by extracting rather than choosing doubtful restorative treatment with less chance of successful outcome is recommended to avoid later complications. There is a high risk of osteonecrosis if extractions have to be carried out after intravenous bisphosphonate therapy is started. Patients on oral bisphosphonates, usually osteoporosis patients, are not subjected to the same high risk of osteonecrosis.
Teeth in Bone Fracture Lines
Sometimes teeth in the line of a jaw fracture should be considered for extraction in order to prevent infection. Tooth luxation can almost always be treated by repositioning and fixation, but where there is severe luxation of teeth associated with complex jaw fractures, where teeth are in the line of the fractures and interfering with the repositioning, these teeth should be extracted (Fig. 8.5).

Other Reasons for Extraction
There are other situations where extraction may be chosen, even when the extraction may be on doubtful indications. In these situations it is especially important to discuss alternative treatment and inform the patient preoperatively so the surgeon and patient agree on the choice of treatment. Extractions can sometimes be performed due to economic reasons. Patients might choose to extract a tooth rather than incur the costs of, for example, having endodontic treatment or a more expensive restorative procedure. Extractions can sometimes also be performed due to esthetic reasons. For example, the patient could choose to extract an upper malformed lateral incisor and have it replaced with an implant. Furthermore, a patient could choose to extract protrusive teeth in the upper front and have them replaced by an implant-supported prosthesis as an alternative to undergoing orthodontic or orthognathic surgical correction. Malformed or severely discolored teeth could also be considered for extraction due to esthetic reasons where the patients choose extraction and prosthetic reconstruction over other procedures such as veneers and crowns. Teeth could sometimes also be extracted due to difficulty in maintaining adequate oral hygiene. Most commonly, the third molars are extracted due the recurrence of pericoronitis and difficulties in maintaining oral hygiene.
Contraindications for Extraction
The surgeon should also consider the contraindications for extracting the tooth, for example with consideration to the patient’s general health or local conditions in the region of extraction. Contraindications for extractions are often relative and can be changed after treating or adjusting the underlying reason for the contraindication.
Systemic Contraindications
These constitute all general health factors and mental factors which have influence on the patient’s ability to withstand the surgical procedure. Severe dental anxiety is a relative contraindication to extraction in local anesthesia and in some cases patients can be treated in general anesthesia. One should pay extra attention to patients on medication such as anticoagulant drugs, cancer medication, glucocorticoids, immunosuppressants and bisphosphonates.
Patients with hemophilia or other coagulopathies should first have their disorders controlled before extraction. In general, most uncontrolled metabolic diseases, such as diabetes, constitute a relative contraindication until they are brought under control. Similarly, patients with severe uncontrolled hypertension and cardiac diseases should ideally be treated for these conditions first before extractions are carried out. Ongoing radio- and/or chemotherapy is also a relative contraindication. In all cases, one should be aware of the medications, especially those drugs that affect the immune system, delay or impair the healing process, or could interact with medication administered to manage an extraction. Some cancer medications, e.g. bisphosphonates, can also cause necrosis of the jaws after extractions.
Local Contraindications
The most common local contraindication is an ongoing acute inflammatory or infectious process. The acute infection/inflammation should first be treated before proceeding with the extraction, depending on the location of the acute process. Extraction of a third lower molar during an ongoing acute pericoronitis could lead to a life-threatening postoperative infection. Local treatment of the pericoronitis is preferred and extraction may be carried out later.
However, there are also situations where an acute abscess is best drained by extraction of the tooth even in an acute phase. Therefore, an acute infectious and inflammatory process should not be considered as an absolute contraindication for extraction. The surgeon should, however, bear in mind that there could be other problems, such as severe pain, swelling, reduced mouth opening, and anxiety, which could make extractions associated with other acute conditions suboptimal. In such cases extractions should be deferred until the acute symptoms have subsided.
One of the most important contraindications to extraction is radiation therapy, past and present, involving the jaws. Delayed healing, dehiscence, and necrosis of the bone are often complications due to extractions performed in irradiated bone. Finally, teeth within the area of a malignant tumor should not be removed before the planning of tumor treatment has been performed.
Clinical Evaluation of the Tooth Before Extraction
Before starting extraction it is important to evaluate the condition of the crown. Deep caries or a large restoration may indicate a high risk for fracture of the crown during extraction, which would complicate the procedure. A tooth with missing crown will require a special approach. Other factors to consider are tooth/root mobility. Ankylosis, which is often seen with infrapositioned primary teeth or teeth subjected to earlier trauma, often indicates a surgical approach for removal of the primary tooth or, with ankylotic infrapositioned permanent teeth in the anterior region, decoronation to preserve the alveolar bone crest in the anterior region should be chosen. It is also important to assess the status of the adjacent teeth to avoid damage to fragile teeth or teeth with large restorations. The clinical evaluation of the tooth to be removed is done in conjunction with a radiographic assessment.
Preoperative Radiographic Examination
Radiographic examination must always be carried out prior to extraction of teeth to evaluate the degree of difficulty of extraction. Root anatomy, presence of pathology in the root or surrounding bone, vital structur/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


