Myositis
Degenerative joint disease (Osteoarthritis)
Aetiology
• It is primarily a disorder of articular cartilage and subchondral bone, with secondary inflammation of the synovial membrane.
• The process starts in loaded articular cartilage, later it thins and clefts (fibrillation) and then breaks away during joint activity leading to sclerosis of underlying bone, subcondylar cysts and osteophyte formation. It is essentially a response of the joint to chronic microtrauma or pressure.
• The microtrauma could be due to continuous abrasion of the articular surfaces as in natural wear associated with age or as a result of increased loading forces possibly related to chronic para functional activity.
• However, the fibrous tissue covering is preserved due to remodelling and the recovery process in osteoarthrosis and osteoarthritis.
• Degenerative joint disease can be either primary or secondary even though they may present similar histopathologic pattern.
• Primary degenerative joint disease is usually of unknown origin, but sometimes genetic factors play an important role.
• Trauma, congenital dysplasia or metabolic disease may be the cause for secondary degenerative disease.
Clinical manifestations
• It is most commonly seen in people above the age of 50 years.
• Patients will have unilateral pain directly over the affected condyle, limitation of mandibular opening, crepitus and a feeling of stiffness after a period of inactivity.
• Tenderness and crepitus on intra-auricular and pre-tragus palpation with deviation of the mandible to the painful side is detected on examination.
• It is detected accidentally on radiographic examination and may not be responsible for facial pain symptoms or TMJ dysfunction.
• When the defects are confined to articular soft tissue, the symptoms may not be diagnosed by conventional radiography. MRI helps to detect soft tissue changes better.
• Radiographic findings may include narrowing of the joint space, irregular joint space, flattening of the articular surfaces, osteophytic formation, anterior lipping of the condyle and the presence of Ely’s cysts.
• These can be seen best on tomograms or CT scans and MRI images.
Treatment
• Conservative treatment is a treatment of choice and should be considered for 6 months to 1 year before considering surgery, unless severe pain or dysfunction persists after an adequate trial of nonsurgical therapy.
• Conservative therapy involves nonsteroidal anti-inflammatory medications, heat application, soft diet, rest and occlusal splints that allow free movement of the mandible.
• When TMJ pain or significant loss of function persists and when distinct radiographic evidence of degenerative joint changes exists, surgery is indicated.
• An arthroplasty, which limits surgery to the removal of osteophytes and erosive areas, is commonly performed. patients with advanced degenerative changes of the TMJ are treated with artificial TMJs.
Rheumatoid arthritis
• The disease process starts as a vasculitis of the synovial membrane progressing to chronic inflammation marked by an intense round cell infiltrate and subsequent formation of granulation tissue.
• The cellular infiltrate spreads from the articular surfaces eventually to cause an erosion of the underlying bone.
Clinical manifestations
• The rheumatoid arthritis (RA) usually involves the TMJ bilaterally.
• The most common symptoms are mandibular opening and joint pain. Pain may be due to the early acute phases of the disease. Other symptoms include morning stiffness, joint sounds and tenderness and swelling over the joint area.
• The symptoms are usually transient in nature only in some cases there will be disability.
• Common findings are pain on palpation of the joints and limitation of opening. Crepitus also may be evident.
• Micrognathia and an anterior open bite are commonly seen in patients with juvenile RA.
• Radiographic changes in the TMJ associated with RA may include a narrow joint space, destructive lesions of the condyle and limited condylar movement.
• There is little evidence of marginal proliferation or other reparative activity in RA in contrast to the radiographic changes often observed in degenerative joint disease.
• High-resolution CT of TMJ in a RA patients will show erosions of the condyle and glenoid fossae that cannot be seen by conventional radiography.
Treatment
• It is treated by anti-inflammatory drugs.
• The patient should be placed on a soft diet during acute exacerbation of the disease process, but intermaxillary fixation is to be avoided because of the risk of fibrous ankylosis.
• Use of a flat plane occlusal appliance may be helpful, particularly if parafunctional habits are exacerbating the symptoms.
• An exercise programme should be started after the acute symptoms subside to help in the mandibular movements.
• When patients have severe symptoms, the use of intra-articular steroids should be considered. Prostheses appear to decrease symptoms in fully or partially edentulous patients.
• Surgical treatment of the joints including placement of prosthetic joints, is indicated in patients who have severe functional impairment or intractable pain not successfully managed by other means.
Psoriatic arthritis
• Psoriatic arthritis (PA) is an erosive polyarthritis occurring in patients with a negative rheumatoid factor who have psoriatic skin lesions.
• The skin lesions starts few years before the joint lesions.
• The cutaneous and joint manifestations of the disease may be traced to the same immunologic abnormality.
Clinical manifestations
• The signs and symptoms are likely to be unilateral and they are more likely that of RA.
• Limitation of mandibular movement, deviation to the side of the pain and tenderness directly over the joint may be observed on examination.
• Erosion of the condyle and glenoid fossae rather than proliferation is detected radiographically.
• Coronal CT is particularly useful in showing TMJ changes of PA.
Treatment
• The management of PA emphasis on physical therapy and NSAIDS that control both pain and inflammation in many cases.
• For patients who do not respond to conservative treatment immunosuppressive drugs, particularly methotrexate, are used for patients with severe disease.
• Only when there is intractable TMJ pain or disabling limitation of mandibular movement is surgery indicated.
• Arthroplasty or condylectomy with placement of costochondral grafts has been performed successfully.
• Surgery may be complicated by psoriasis forming in the surgical scar (Koebner effect).
Septic arthritis
• Septic arthritis of the TMJ occurs in patients with previously existing joint disease such as RA.
• Septic arthritis is also seen patients receiving immunosuppressive drugs or long-term corticosteroids.
• The infection of the TMJ may result from blood-borne bacterial infection or through infection from adjacent sites such as the middle ear, maxillary molars and parotid gland.
• Gonococci are the primary blood borne agents causing septic arthritis in a previously normal TMJ.
Clinical symptoms
• Symptoms include trismus, deviation of the mandible to the affected side, severe pain on movement and an inability to occlude the teeth, owing to the presence of inflammation in the joint space.
• Examination reveals redness and swelling in the region of the involved joint.
• Septic arthritis can be differentiated from more common types of TMJ disorders by large tender cervical lymph nodes on the side of the infection.
• Diagnosis is made by detection of bacteria on grams stain and culture of aspirated joint fluid.
• Serious sequelae include osteomyelitis of the temporal bone, brain abscess and ankylosis.
• Facial asymmetry may accompany septic arthritis of the TMJ, especially in children. The primary sources of these infections were the middle ear, teeth and the hematologic spread of gonorrhoea.
• Evaluation of patients with suspected septic arthritis must include a review of signs and symptoms of gonorrhoea, such as purulent urethral discharge or dysuria.
Treatment
Gout and pseudogout
• Gouty arthritis is caused by long-term elevated serum urate levels, which results in the deposition of crystals in a joint, triggering an acute inflammatory response.
• Acute pain in a single joint, i.e., monoarticular arthritis is the characteristic clinical manifestation of gouty arthritis.
• Gouty arthritis appears to be very rare, an attack of gouty arthritis is most accurately diagnosed by examination of aspirated synovial fluid from the involved joint by polarized light microscopy.
• The detection of monosodium urate crystals confirms the diagnosis of gout.
• An acute attack of gout can be treated with colchicine, NSAIDS or the intra-articular injection of corticosteroids.
• The deposition of other crystals, such as calcium pyrophosphate dihydrate (CPPD) or calcium hydroxyapatite, may cause a syndrome that resembles gout and that has been referred to as pseudogout.
• This disorder most frequently effects elderly individuals, with the involvement of the TMJ.
• Colchicine or arthrocentesis is used for successful treatment of pseudogout of TMJ.
Q. 2. Describe in detail MPDS.
Or
Write clinical features and management of MPDS.
Or
Management of MPDS.
Ans.
• When muscle spasm develops in one or more masticatory muscles, dysfunction as well as pain occurs and the condition usually is designated as MPDS.
• The muscles of mastication, the tongue muscles and the strap muscle of the neck function as a unit and that dysfunction in one group of muscles is frequently associated with altered tonus and symptoms of ‘tension’ in the other related groups.
Aetiology
Occlusal status
• Periodontal point of view: It is a self-protecting and modifications occur in the pathway of closure to avoid and potentially damaging or painful contacts.
• Tooth muscle theory: In coordination and spasm of some muscles of mastication is caused due to occlusal interferences and altered proprioceptive feedback.
• Prosthetic reasons: Decreased vertical dimension due to over closure due to bilateral loss of molar teeth or increased VD in partial and complete dentures lead to TMJ dysfunction.
• Orthodontic conditions: Malocclusion, discrepancies in occlusion or MPDS can lead to TMJ dysfunction.
Psycho-physiologic theory
Spasm due to over extension of muscles due to following reasons:
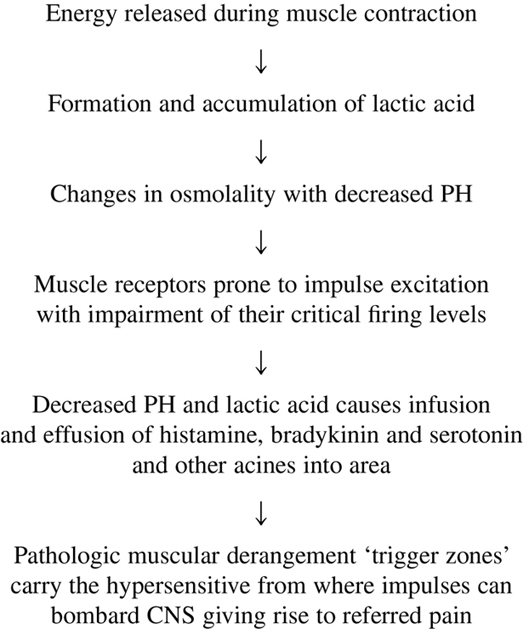
Pathogenesis
Joint status
Cardinal signs and symptoms outlined by laskin
Positive characteristics emphasized by laskin
Negative characteristics emphasized by laskin
Signs
Symptoms
Treatment of MPDS
• Treatment of MPDS should include the treatment of emotional as well as physical components of the disorder.
• In acute stages, conservative noninvasive treatment is usually successful in alleviating the pain and dysfunction.
• Treatment of MPDS should begin with strong doctor–patient relationship by showing concern and empathy when reviewing the history of patient problems.
• Patient should be told that they are not suffering from more serious, life threatening disorder like malignancy.
Conservative treatment and recommendations
Conservative treatment and recommendations at the initial visit should include the following:
• Limitation of parafunctional habits: Patient should attempt to limit parafunctional habits by becoming more aware of clenching and grinding of the teeth during the day.
• Hot moist packs: Warm to hot, moist compresses should be applied over the involved muscles for 15–20 minutes three times a day.
• Soft diet: A relatively soft diet should be advised and limit wide opening of mouth while eating.
• Pharmacotherapy or drugs to be prescribed: Aspirin or NSAID should be recommended for analgesic and anti-inflammatory actions.
• Breaking up stress–pain–stress cycle with LA injections without epinephrine: Injecting the trigger points of muscles that are in spasm with a local anaesthetic not containing epinephrine is often beneficial in breaking up the spasm and in disrupting the stress pain stress cycle.
• Ethylchloride spray on the skin: The skin over lying the affected muscles can be sprayed with ethylchloride or fluoromethane or ultrasound can be used in an attempt to relieve muscle spasms. The effectiveness of local anaesthetic injections ethylchloride refrigerant spray, and ultrasound in allowing patients to open wide without pain may be noted immediately following treatment.
• Jaw exercises: Isometric exercises are often beneficial, for example, placing the tip of the tongue in the back of the palate and then opening and closing may help in retraining spastic muscles.
• Diazepam: Diazepam 2 mg/3 times daily and 5 mg at bed time during a 2-week trial period is commonly advocated for its anxiety reducing and muscle relaxing properties.
Occlusal splints
• They should be fabricated if pain and dysfunction persist without improvement following the treatment and recommendations of the initial visit.
• Splints most often used are:
• Benefits derived from occlusal splints have most commonly attributed to greater freedom in mandibular movement and to an increase in muscle balance.
Biofeedback
• It is helpful when the primary reason for the failure in initial treatment appears to be the inability to control stress and anxiety.
• Biofeedback is a valuable therapeutic aid that permits patients to treat themselves while decreasing their dependence on therapists as it provides them with information concerning bodily functions that are usually not discernible or controllable.
Nerve stimulation
• Transcutaneous electrical nerve stimulation (TENS) treatment appears to be more effective in alleviating chronic pain than acute pain.
• The mode of action of TENS in reducing pain is uncertain but it is attributed to neurologic, physiologic, pharmacologic and psychologic effects.
• The pharmacologic action of TENS may involve the stimulated release of endorphins, which are endogenous morphine like substances.
Other treatments
Treatment of MPDS is summarized below
| Treatment Component | Description |
| Education | The diagnosis and treatment should be explained to the patient Encourage the patient to take self-care with reassurance about the good prognosis |
| Self-care | Educate the patient towards elimination of oral habits (e.g., tooth clenching, chewing gum) |
| Physical therapy | Education regarding biomechanics of jaw, neck and head posture Passive modalities and posture therapy with general stretching and exercise is advised |
| Intraoral appliance therapy | Cover all the teeth in the arch with appliance placed on them Simultaneous contact against opposing teeth should be achieved Adjust to comfortable position avoiding continuous use |
| Pharmacotherapy | NSAIDs, acetaminophen, muscle relaxants, antianxiety agents, tricyclic antidepressants and clonazepam |
| Behavioural/relaxation techniques | Relaxation therapy such as hypnosis is preferred |
Q. 3. What conditions may produce trismus?
Or
Enumerate the causes of trismus. Discuss in detail.
Ans. The word trismus is derived from the Greek word ‘trismus’ meaning gnashing and is defined as a prolonged, tetanic spasm of the jaw muscles by which normal opening of the mouth is restricted (locked jaw).
Aetiology
• Fractures of mandible, zygomatic or temporal bones
• Haematomas in the joint or muscle of mastication
• Injury due to local anaesthetic injection
• Tumours of the oropharynx (Trotter syndrome)
• Metastatic disease of the mandible and infratemporal fossa
• Osteomyelitis of the mandible and temporal bone
• Abscesses of the submasseteric, lateral pharyngeal, pterygomandibular, submandibular and temporal spaces
Clinical examination
Treatment
Q. 4. Describe in detail TMJ ankylosis.
Ans.
• TMJ ankylosis is an intra-articular condition where there is a fusion between the bony surfaces of the joint, the condyle and the glenoid fossa. The term ‘ankylosis’ is derived from the Greek word that means stiffening of a joint as a result of a disease process.
• Ankylosis of the mandible with immobility of the joint may be of an osseous, fibro-osseous or cartilaginous variety.
• Ankylosis must be distinguished from its counterpart pseudoankylosis.
• In pseudoankylosis, hypomobility of the joint occurs due to coronoid hyperplasia or due to fibrous adhesions between the coronoid and tuberosity of the maxilla or zygoma as in ‘V-shaped’ fracture of the zygomatic arch impinging on coronoid leading to fibrous or bony union are also examples of pseudoankylosis.
• In pseudoankylosis, even though jaw movement is restricted as in bony ankylosis, the pathology is extra-articular in these cases.
Aetiopathology
I. Tauma
• Most cases of ankylosis result from condylar injuries sustained before 10 years of age.
• A unique pattern of condylar fractures is seen in children. Condylar cortical bone in children is thin with a broad condylar neck and rich subarticular interconnecting vascular plexus. An intracapsular fracture leads to combination and haemarthrosis of the condylar head. This sort of intracapsular burst fracture is called ‘ mushroom fracture’.
• It results in the organization of a fibro-osseous mass in a highly osteogenic environment. Moreover, immobility leads to ossification and consolidation of the mass, resulting in ankylosis.
• Ankylosis may also occur in trauma sustained during forceps delivery.
Laskin (1978) had outlined various factors that may be implicated in the aetiology of ankylosis following trauma, they are as follows:
• Younger patients have significantly higher osteogenic potential and rapidity of repair. Moreover, the articular capsule is not as well developed in younger patients, thus permitting easier condylar displacement out of the fossa and thereby damage to the disc ultimately, there is a greater tendency for prolonged self-imposed immobilization of the mandible posttraumatically in children.
• The condyle in children has a thinner cortex along with a thick neck, which predisposes them to a higher proportion of intracapsular comminuted fractures. In contrast, adults have a thinner condylar neck which usually fractures at the neck, thus sparing the head of the condyle within the capsule.
II. Local infections
III. Systemic conditions
• In systemic conditions like tuberculosis, meningitis, pharyngitis, tonsillitis, rubella, varicella, scarlet fever, gonococcal arthritis, ankylosing spondylitis, the route of spread of infection is haematogenous.
• The local and systemic infections may pass along as septic arthritis, which may not always cause ankylosis. Staphylococcus species, Streptococcus species, Haemophilus influenzae, Neisseria gonorrhoea are the most likely causes of septic arthritis. The infection may take either the haematogenous, contiguous, or by direct inoculation. The synovium with its high vascularity and lack of a limiting basement membrane is vulnerable to infection.
IV. Arthritis/inflammatory conditions
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


