Chapter 6 Treatment Planning: Force Factors Related to Patient Conditions
Biomechanical stress is a significant risk factor in implant dentistry. Its magnitude is directly related to force. As a result, an increase in any dental force factor magnifies the risk of stress-related complications. Different patient conditions place different amounts of force in magnitude, duration, type, and direction. In addition, several factors may multiply or increase the effect of these other conditions. Once the prosthesis option and key implant positions are determined, the potential force levels that will be exerted on the prosthesis should be evaluated and accounted for in order to modify the overall treatment plan. Several elements observed during the dental evaluation predict additional forces on future implant abutments. The initial implant survival, loading survival, marginal crestal bone loss, incidence of abutment or prosthetic screw loosening, and unretained restorations, porcelain fracture, and component fracture are all influenced by the force factors.
Box 6-1 includes primary patient factors affecting the stress environment of the implant and prosthesis.
NORMAL BITE FORCE
The greatest natural forces exerted against teeth, and thus against implants, occur during mastication.1,2 These forces are primarily perpendicular to the occlusal plane in the posterior regions, are of short duration, occur only during brief periods of the day, and range from 5 to 44 lb for natural teeth. The actual force on each tooth during function has been recorded on strain gauges in inlays.3 A force of 28 psi was needed to chew a raw carrot, and 21 psi was needed to chew meat. The actual time during which chewing forces are applied on the teeth is about 9 minutes each day.4 The perioral musculature and tongue exert a more constant, yet lighter horizontal force on the teeth or on implants. These forces reach 3 to 5 psi during swallowing.5 A person swallows 25 times per hour while awake and 10 times per hour while sleeping, for a total of 480 times each day.4 Therefore natural forces against teeth are primarily in their long axis, less than 30 psi, and for less than 30 minutes for all normal forces of deglutition and mastication (Box 6-2). Forces of mastication placed on implant-supported bridges have been measured in a similar range as natural teeth.
Box 6-2 Normal Forces Exerted on Teeth
The maximum bite force differs from mastication force, varies widely among individuals, and depends on the state of the dentition and masticatory musculature. There have been many attempts to quantify the normal maximum bite force. In 1681, Borelli suspended weights on a thread over the molars while the mandible was open. The maximum load recorded for which the person was still able to close ranged from 132 to 440 lb. A force of 165 lb was recorded on a gnathodynamometer, the first instrument to record occlusal force, which was developed by Patrick and Dennis in 1892. Black improved this early design and recorded average forces of approximately 170 lb.6 More recent studies indicate normal maximum vertical biting forces on teeth or implants can range from 45 to 550 psi.7–22 The forces on the chewing side and the opposite side appear very similar in amplitude8 (Table 6-1).
Table 6-1 Mean Maximum Biting Force Recorded on Natural Teeth or Implants
| AUTHORS | NATURAL TEETH DENTAL IMPLANTS | MEAN MAXIMUM MASTICATORY FORCE |
|---|---|---|
| Carr and Laney, 1987a | Conventional denture | 59 N |
| Implant-supported prostheses | 112.9 N | |
| Morneburg and Proschel, 2002b | Implant-supported three-unit FPD | 220 N |
| Single implant: anterior | 91 N | |
| Single implant: posterior | 12 N | |
| Fontijn-Tekamp et al., 1998c | Implant-supported prostheses | (unilateral) |
| Molar region | 50-400 N | |
| Incisal region | 25-170 N | |
| Mericske-Stern and Zarb, 1996d | Complete denture/implant-supported prostheses | 35-330 N |
| van Eijden, 1991e | Canine | 469 ± 85 N |
| 2nd premolar | 583 ± 99 N | |
| 2nd molar | 723 ± 138 N | |
| Braun et al., 1995f | Natural teeth | 738 ± 209 N (male > female) |
| Raadsheer et al., 1999g | Male teeth | 545.7 N |
| Female teeth | 383.6 N |
Comparison of available studies examining masticatory forces generated under varying loading condition. Study results are reported in Newtons (N) of force unless otherwise indicated. Differences between male and female force generation are noted in applicable studies.
FPD, Fixed partial dentures.
a Carr AB, Laney WR: Maximum occlusal forces in patients with osseointegrated oral implant prostheses and patients with complete dentures, Int J Oral Maxillofac Impl 2:101-108, 1987.
b Morneburg TR, Proschel PA: Measurement of masticatory forces and implant loads: a methodologic clinical study, Int J Prosthodont 15:20-27, 2002.
c Fontijn-Tekamp FA, Slageter AP, van’t Hof MA et al: Bite forces with mandibular implant-retained overdentures, J Dent Res 77:1832-1839, 1998.
d Mericske-Stern R, Assal P, Buergin W: Simultaneous force measurements in three dimensions on oral endosseous implants in vitro and vivo: a methodological study, Clin Oral Implants Res 7:378-386, 1996.
e van Eijden TM: Three dimensional analyses of human bite force magnitude and moment, Arch Oral Biol 36:535-539, 1991.
f Braun S, Bantleon HP, Hnat WP et al: A study of bite force. Part I: relationship to various physical characteristics, Angle Orthod 65:367-372, 1995.
g Raadsheer MC, van Eijden TM, van Ginkel FC et al: Contribution of jaw muscle size and craniofacial morphology to human bite force magnitude, J Dent Res 87:31-42, 1999.
PARAFUNCTION
Parafunctional forces on teeth or implants are characterized by repeated or sustained occlusion and have long been recognized as harmful to the stomatognathic system.23–25 These forces are also most damaging when applied to implant prostheses.18 The lack of rigid fixation during healing is often a result of parafunction on soft tissue-borne prostheses overlying the submerged implant. The most common cause of both early and late implant failure after successful surgical fixation is the result of parafunction. Such complications occur with greater frequency in the maxilla, because of a decrease in bone density and an increase in the moment of force.26 The presence of these conditions must be carefully noted during the early phases of treatment planning.
Nadler has classified the causes of parafunction or nonfunctional tooth contact into the following six categories24:
Local factors include tooth form or occlusion, as well as soft tissue changes such as ulcerations or pericoronitis. Systemic factors include cerebral palsy, epilepsy, and drug-related dyskinesia. Psychological causes occur with the greatest frequency and include the release of emotional tension or anxiety.27 Occupational factors concern professionals such as dentists, athletes, and precision workers, as well as the seamstress or musician who develops altered oral habits. The fifth cause of parafunctional force is involuntary movement that provokes bracing of the jaws, such as during lifting of heavy objects or sudden stops while driving. Voluntary causes include chewing gum or pencils, bracing the telephone between the head and shoulder, and pipe smoking.
Bruxism
Bruxism primarily concerns the horizontal, nonfunctional grinding of teeth. The forces involved are in significant excess of normal physiologic masticatory loads. Bruxism may affect the teeth, muscles, joints, bone, implants, and prostheses. These forces may occur while the patient is awake or asleep and may generate increased force on the system several hours per day. Bruxism is the most common oral habit.25 Sleep clinic studies have evaluated nocturnal bruxism and found approximately 10% of those observed had obvious movement of the mandible with occlusal contacts.28,29 More than half of these patients had tooth wear affecting esthetics. Only 8% of these patients were aware of their nocturnal bruxism, and only one quarter of the patients— spouses were aware of the nocturnal habit. Muscle tenderness in the morning was observed less than 10% of the time.30 A study on bruxing patients with implants showed 80% of sleep bruxism occurred during light sleep stages but did not cause arousal.31 Therefore patients with bruxism may or may not have obvious tooth wear affecting esthetics; may brux nocturnally, but their bed partners do not know most of the time; rarely have muscle tenderness when they are awake; and are usually unaware of their oral habit. In other words, nocturnal bruxism is sometimes difficult to diagnose.32
The maximum biting force of bruxing patients is greater than average. Just as an experienced weight-lifter can lift more weight, the patient constantly exercising the muscles of mastication develops a greater bite force. A man who chews paraffin wax for an hour each day for a month can increase the bite force from 118 to 140 psi within 1 week. Chewing gum, bruxism, and clenching may accomplish the same feat. Eskimos, with a very tenacious diet and who chew their leather to soften it before fabrication of clothing, have maximum bite forces above 300 psi. A 37-year-old patient with a long history of bruxism recorded a maximum bite force of more than 990 psi (four to seven times normal).33 Fortunately, the bite force does not continue to increase in most bruxing patients. When muscles do not vary their exercise regimen, their size and function adjust to the dynamics of the situation. As a result, the higher bite forces and muscle size usually do not continue in an unending spiral.
Diagnosis
Bruxism does not necessarily represent a contraindication for implants, but it does dramatically influence treatment planning. The first step is to recognize the condition before the treatment is rendered. The symptoms of this disorder, which may be ascertained by a dental history, may include repeated headaches, a history of fractured teeth or restorations, repeated uncemented restorations, and jaw discomfort upon awakening.23,34 Therefore when the patient is aware of muscle tenderness or the spouse is conscious of the nocturnal condition, the diagnosis is readily obtained. However, many patients do not attribute these problems to excessive forces on the teeth and report a negative history. A lack of these symptoms does not negate bruxism as a possibility.
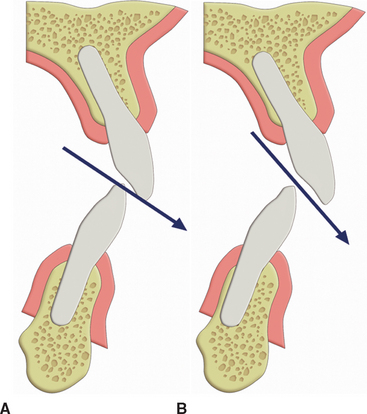
Fortunately many clinical signs warn of excessive grinding. The signs of bruxism include an increase in size of the temporal and masseter muscles (these muscles and the external pterygoid may be tender), deviation of the lower jaw on opening, limited occlusal opening, increased mobility of teeth, cervical abfraction of teeth, fracture of teeth or restorations, and uncemented crowns or fixed prostheses. However, the best and easiest way to diagnose bruxism is to evaluate the wearing of teeth. Not only is this the easiest method to determine bruxism in an individual patient, it also allows the disorder to be classified as absent, mild, moderate, or severe (Figures 6-1 to 6-3). No anterior wear patterns in the teeth signify an absence of bruxism. Mild bruxism has slight wearing of anterior teeth but is not a cosmetic compromise. Moderate bruxism has obvious anterior incisal wear facets but no posterior occlusal wear pattern. Severe bruxism has absent incisal guidance from excessive wear, and posterior wearing of the teeth is obvious.

Figure 6-2 Patients often grind their teeth in a specific, repeated movement of the mandible. When the opposing wear facets of the teeth are in contact, one should note the occlusal position of the teeth. The patient shown in Figure 6-1 has a working contact on the mandibular premolar with the maxillary canine in this engram position. The slight cervical abfraction of the mandibular first premolar is a consequence of the parafunction. The patient’s posterior teeth should not occlude in this position to decrease the amount of force on the anterior teeth.
Tooth wear is most significant when found in the posterior regions and changes the intensity of bruxism from the moderate to the severe category. Posterior wear patterns are more difficult to manage, because this usually is related to a loss of anterior guidance in excursions; once the posterior teeth contact in excursive jaw positions, greater forces are generated.35 The masseter and temporalis muscles contract when posterior teeth contact. With incisal guidance and an absence of posterior contact, two thirds of these muscles do not contract and, as a consequence, the bite force is dramatically reduced. However, when the posterior teeth maintain contact, the bite forces are similar in excursions, as during posterior biting. Therefore in the patient with severe bruxism, the occlusal plane, the anterior incisal guidance, or both may need modification to eliminate all posterior contacts during mandibular excursions before the implant restoration.
Bruxing patients often repeat mandibular movements, which are different from border movements of the mandible and are in one particular direction. As a result, the occlusal wear is very specific and primarily on one side of the arch, or even on only a few teeth (Figure 6-4). This engram pattern usually remains after treatment. If the restoring dentist reestablishes incisive guidance on teeth severely affected by an engram bruxing pattern, the incidence of complications on these teeth will be increased. The most common complications on teeth restored in this “pathway of destruction” are porcelain fracture, uncemented prostheses, and root fracture.34 When implants support the crowns in the pathway of destruction, the implant may fail, fracture, or have crestal bone loss, abutment screw loosening, porcelain fracture, or unretained restorations.36–39 If the patient continues the severe bruxism pattern, the question is not whether, but when and which complications will occur. The dentist should tell the patient that these habits will cause these problems. Treatment may be rendered to repair these problems, but there will be complications if the bruxism is not reduced.
Bruxism changes normal masticatory forces by the magnitude (higher bite forces), duration (hours rather than minutes), direction (lateral rather than vertical), type (shear rather than compression), and magnification (four to seven times normal).33,40–42 The method to restore severe bruxism may be problematic, even when the desire is primarily cosmetic. As the anterior teeth wear, they often erupt and the overall occlusal vertical dimension remains unchanged. In addition, the alveolar process may follow the eruption of the tooth. As such, when the anterior teeth are restored for esthetics (or to obtain an incisal guidance), the reduced crown height cannot be increased merely by increasing the height of the crown to an average dimension. Instead, the following guidelines are suggested:
In patients with moderate to severe bruxism, the height of the vertical overjet and the angle of incisal guidance should not be extreme, as the amount of the force on the anterior abutments, cement seals, and porcelain is directly related to these conditions (Figure 6-5). In other words, the greater the incisal overjet, the greater the distance between the posterior teeth in excursions, and the greater the force generated on the anterior teeth during this movement. In patients with severe bruxism, the intensity of the force should be reduced, because the duration of the force is increased.
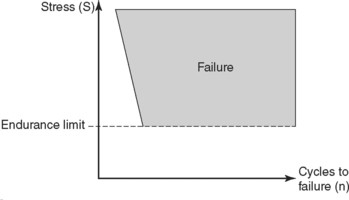
Fatigue Fractures
The increase in duration of the force is a considerable problem. Materials follow a fatigue curve, which is affected by the number of cycles and the intensity of the force43–45 (Figure 6-6). A force can be so great that one cycle causes a fracture (e.g., a karate blow to a piece of wood). However, if a lower force magnitude repeatedly hits an object, the object will still fracture. The wire coathanger that is bent does not break the first time, but repeated bends will fracture the material, not because the last bend was more forceful but because of fatigue. A bruxing patient is at greater risk of fatigue fractures for two reasons. The magnitude of the forces increases over time as the muscles become stronger, and the number of cycles increase on the prosthetic components. Eventually, one of the components (implant, screw, abutment, prosthesis) will break if the parafunction cannot be reduced in intensity or duration (Figure 6-7). No long-term prosthetic result is expected in patients with severe bruxism. Therefore, once the implant dentist has identified the sources of additional force on the implant system, the treatment plan is altered in an attempt to minimize the negative effect on the longevity of the implant, bone, and final restoration. All elements able to reduce stress should be considered.
Occlusal Guards
The cause of bruxism is multifactorial and may include occlusal disharmony.46 When an implant reconstruction is considered in a bruxing patient, occlusal analysis is warranted. Premature and posterior contacts during mandibular excursions increase stress conditions. An elimination of eccentric contacts may allow recovery of periodontal ligament health and muscle activity within 1 to 4 weeks. Occlusal harmony does not necessarily eliminate bruxism, but this is no reason not to perform an occlusal analysis and eliminate the premature contacts. No study demonstrates an increase in parafunction after occlusal adjustment. Therefore the ability to decrease the risk of occlusal overload on particular teeth and the added benefit of perhaps reducing parafunction is warranted in almost every patient diagnosed with a parafunctional habit of bruxism or clenching.
A night guard can be a useful diagnostic tool to evaluate the influence of occlusal disharmony on nocturnal bruxism. The Michigan night guard exhibits even occlusal contacts around the arch in centric relation occlusion and provides posterior disocclusion with anterior guidance in all excursions of the mandible.47 This device may be fabricated with 0.5 to 1 mm colored acrylic resin on the occlusal surface. After 4 weeks of nocturnal wear, if the patient wears this device for an additional month or more, the influence of occlusion on the bruxism may be directly observed. There are no premature contacts while the device is worn; however, if the colored acrylic is still intact, the nocturnal parafunction has been reduced or eliminated.48 Therefore occlusal reconstruction or modification may proceed. If the colored acrylic on the night guard is ground through, an occlusal adjustment will have little influence on decreasing this parafunctional habit. The night guard is still indicated to relieve stresses during nocturnal parafunction, but the treatment plan should account for the greater forces.
Forces from bruxism are the most difficult to address on a long-term basis. Education and informed consent of the patient are helpful to gain cooperation in eliminating or reducing the noxious effects. If the opposing arch is a soft tissue-supported removable prosthesis, the effects of the nocturnal habit may be minimized if the patient removes the prosthesis at night. The use of a night guard is helpful for a patient with a fixed prosthesis, in order to transfer the weakest link of the system to the removable acrylic device.49 Centric contacts in centric relation occlusion and anterior-guided disocclusion of the posterior teeth in excursions are strongly suggested on the night guard, which may be designed to fit the maxilla or mandible.
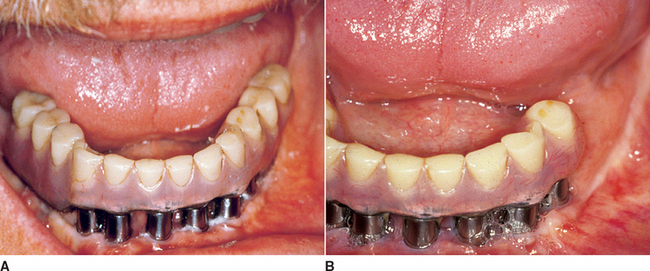
Unlike teeth, implants do not extrude in the absence of occlusal contacts. As a result, in partially edentulous patients, the maxillary night guard can be relieved around the implant crowns so the remaining natural teeth bear the entire load. For example, for a maxillary implant restoration, the night guard is hollow so no occlusal force is transmitted to the implant crown. When the restoration is in the mandible, the occluding surfaces of the maxillary night guard are relieved over the implant crowns so no occlusal force is transmitted to the implants (Figure 6-8).
A mandibular posterior cantilever on a full-arch implant prosthesis may also be taken out of occlusion with a maxillary night guard. When a posterior quadrant of implants supports a fixed prosthesis in the maxilla opposing mandibular teeth, a soft reline material is placed around the implant crowns to act as a stress relief element and decrease the impact force on the restoration (Figure 6-9). When full-arch implant restorations are opposing each other, the night guard provides solely anterior contacts during centric occlusion and mandibular excursions. Thus the parafunctional force is reduced on the anterior teeth/implants and eliminated in the posterior regions.
Treatment Planning
The implant treatment plan is modified primarily in two ways when implants are inserted in the posterior region: (1) additional implants that are wider in diameter are one method used to reduce the overload risk or (2) the anterior teeth may be modified to recreate the proper incisal guidance and avoid posterior interferences during excursions. The elimination of posterior lateral occlusal contacts during excursive movements is recommended when opposing natural teeth or an implant or tooth-supported fixed prosthesis. This is beneficial in two aspects: (1) because lateral forces dramatically increase stress at the implant-bone interface, the elimination of posterior contacts diminishes the negative effect of angled forces during bruxism; (2) the presence of posterior contacts during excursions, almost all fibers of the masseter, temporalis, and the external pterygoid muscles contract and place higher forces on the anterior teeth/implants. On the contrary, during excursions in the absence of posterior contacts, fewer fibers of the temporalis and masseter muscles are stimulated, and the forces applied on the anterior implant-teeth system are reduced by as much as two thirds.25
Diagnosis
Many clinical symptoms and signs warn of excessive grinding. However, the signs for clenching are often less obvious. The forces generated during clenching are directed more vertically to the plane of occlusion, at least in the posterior regions of the mouth. Wearing of the teeth is usually not evident; therefore clenching often escapes notice during the intraoral examination. As a result, the dentist must be more observant to the diagnosis of this disorder.25,
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses