Background
Q: What is the difference between gingivitis and periodontitis?
Gingivitis is gingival inflammation without loss of connective tissue attachment. Periodontitis is gingival inflammation at sites where there has been loss of collagen fibers from cementum and the junctional epithelium has migrated apically. Periodontitis results from the advancement of gingivitis.1
Q: What is clinical attachment level?
Clinical attachment level (CAL) is the distance from the cementoenamel junction (CEJ) to the tip of the periodontal probe during normal probing.
Q: What is probing depth?
Probing depth is the distance from the soft tissue margin to the tip of the periodontal probe.
Q: What can affect probing depth?
The following factors may influence probing depth:
• Insertion force
• Size of the probe tip
• Inflammatory status of the tissues
In health, the probe should stop within the junctional epithelium. In patients with periodontitis, it may stop in connective tissue or bone.
Classification
The classification presented in the following answers is taken directly from the 1999 American Academy of Periodontology classification of periodontal diseases.2
Q: What are the dental plaque–induced gingival diseases?
I. Gingival diseases
A. Dental plaque–induced gingival diseases
1. Gingivitis associated with dental plaque only
a. without other local contributing factors
b. with local contributing factors
2. Gingival diseases modified by systemic factors
a. associated with the endocrine system
1) puberty-associated gingivitis
2) menstrual cycle–associated gingivitis
3) pregnancy-associated
a) gingivitis
b) pyogenic granuloma
4) diabetes mellitus–associated gingivitis
b. associated with blood dyscrasias
5) leukemia-associated gingivitis
6) other
3. Gingival diseases modified by medications
a. drug-influenced gingival diseases
1) drug-influenced gingival enlargements (Fig 6-1)
2) drug-influenced gingivitis
a) oral contraceptive–associated gingivitis
b) other
4. Gingival diseases modified by malnutrition
a. ascorbic acid–deficiency gingivitis
b. other

Fig 6-1 Drug-induced gingival enlargement.
Q: What are the non–plaque-induced gingival diseases?
B. Non–plaque-induced gingival lesions
1. Gingival diseases of specific bacterial origin
a. Neisseria gonorrhea–associated lesions
b. Treponema pallidum–associated lesions
c. streptococcal species–associated lesions
d. other
2. Gingival diseases of viral origin
a. herpesvirus infections
1) primary herpetic gingivostomatitis
2) recurrent oral herpes
3) varicella-zoster infections
4) other
3. Gingival diseases of fungal origin
a. Candida species infections
1) generalized gingival candidosis
b. linear gingival erythema
c. histoplasmosis
d. other
4. Gingival lesions of genetic origin
a. hereditary gingival fibromatosis
b. other
5. Gingival manifestations of systemic conditions
a. mucocutaneous disorders
1) lichen planus
2) pemphigoid
3) pemphigus vulgaris
4) erythema multiforme
5) lupus erythematosus
6) drug-induced
7) other
b. allergic reactions
1) dental restorative materials
a) mercury
b) nickel
c) acrylic
d) other
2) reactions attributed to
a) toothpaste/dentifrices
b) mouthrinses/mouthwashes
c) chewing gum additives
3) other
6. Traumatic lesions
a. chemical injury
b. physical injury
c. thermal injury
7. Foreign body reactions
8. Not otherwise specified
Q: What are the two subclassifications for chronic and aggressive periodontitis and their associated extent and severity?
II. Chronic periodontitis
A. Localized
B. Generalized
III. Aggressive periodontitis
A. Localized (Fig 6-2)
B. Generalized
Extent: Localized means ≤ 30% of sites are involved and generalized means > 30% of sites are involved.
Severity (based on CAL): Slight = 1 to 2 mm; moderate = 3 to 4 mm; severe ≥ 5 mm.
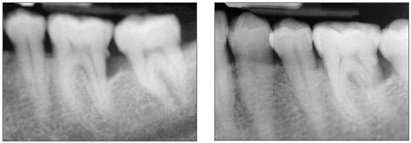
Fig 6-2 Radiographic appearance of localized aggressive periodontitis.
Q: How is localized aggressive periodontitis distinguished from generalized aggressive periodontitis?
Table 6-1 presents the distinguishing characteristics of localized and generalized aggressive periodontitis.
| Table 6-1 | Localized and generalized aggressive periodontitis* | |
| Localized aggressive periodontitis | Generalized aggressive periodontitis | |
| Amount of plaque and calculus | Absence of large accumulations of plaque and calculus | Marked periodontal inflammation and heavy accumulations of plaque and calculus |
| Teeth affected | Interproximal attachment loss on at least two permanent first molars and incisors, with attachment loss on no more than two teeth other than first molars and incisors | Generalized interproximal attachment loss including at least three teeth that are not first molars and incisors |
| Population | Occurs in children and adolescents without clinical evidence of systemic disease and is characterized by the severe loss of alveolar bone around permanent teeth |
Stay updated, free dental videos. Join our Telegram channel
VIDEdental - Online dental courses
 Get VIDEdental app for watching clinical videos
Get VIDEdental app for watching clinical videos

|
