Chapter 6
Basic Surgical Principles
Aseptic Technique
Since the late 1800s, when bacteria were first recognized, the concept in surgery has turned from accepting pathogenic agents, and hoping that the body can overcome them, to attempting to eliminate them from the surgical field. In hospitals, most operations are carried out using a truly aseptic technique. All instruments are sterile, having been autoclaved, or all organisms eliminated by some other physiochemical means. In addition, the operating room itself is surgically clean, and all trays, etc., on which instruments rest are sterile. The surgeon wears sterile gloves and a sterile gown, and a mask, head covering, and shoe covers or separate footwear that is only worn in the operating room. An aseptic technique is employed whereby sterile and non-sterile objects do not contact each other so that there is a continuous chain of sterility; the only organisms that come in contact with the patient are their own endogenous organisms. In this way, infections should not occur, and, in theory at least, antibiotics and other chemotherapeutic agents should be unnecessary if no exogenous infecting agents are introduced. In practice this type of sterility, although ideal, is imperfect. Infections do still occur in the operating room for a variety of reasons and antibiotics do still need to be employed in many cases.
The rules for carrying out invasive surgery in the operating room environment of a hospital are fairly standard and clear cut. The rationale in a dentist’s, or oral surgeon’s office, is, however, less clear cut. For many years, dentistry and relatively minor oral surgical procedures were carried out in an outpatient office without the use of gloves, cap, or mask and with only a clean gown or coat. This changed in the 1980s when new generations of pathogenic organisms were identified including hepatitis B and hepatitis C viruses, and human immunodeficiency virus (HIV). Following this, to protect both the dentist and the patient, dentists started to wear gloves, caps, and masks.
At the present time, there is no standard for the level of asepsis to be practiced in a dental office or for oral surgery performed in an outpatient setting. In all cases, dentists will now wear caps, masks, and gloves, but in most cases they will continue to wear their outside shoes. Gowns are often worn but are often not sterile but rather cleaned and laundered and changed between patients. Gloves are normally sterile for invasive procedures but are generally non-sterile for non-invasive procedures. Aseptic technique is not strictly followed in most cases, and, although all instruments are sterile and are normally placed on a sterile surface, they may on occasion come in contact with non-sterile instruments and techniques. For this reason, the chain of sterility is less secure in an office environment, and thus antibiotics tend to be used more frequently, and often prophylactically.
Principles of Surgical Incisions
Incisions are most often made with a surgical scalpel, and for oral and maxillofacial surgery, the #15 blade with its rounded tip is the most popular, although the #11 blade with its pointed tip and the #12C blade with its smaller rounded tip are popular for some procedures with some surgeons. Incisions should be made with one single firm movement using the palm of the hand as a support for the scalpel handle to avoid undesirable instability.
Incisions can also be made with electrosurgery or a laser, or even combined instruments such as a scalpel blade with electrosurgery capacity built into it, although these latter instruments are often expensive, somewhat unreliable, and not widely used. Electrosurgical cutting, although it produces a relatively bloodless field, does so at the expense of surface cauterization and does produce more wound breakdown, scarring and wound contracture, and so is generally not employed in esthetic areas.
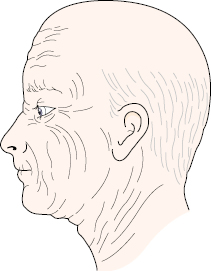
Skin incisions around the face are best sited either in established skin creases, the site of future skin creases (in young patients), or in the relaxed skin tension lines (RSTL) (Fig. 6.1). These lines generally run at right angles to the direction of the underlying musculature and are roughly equivalent to the original lines described by Langer in 1861, which he produced by puncturing the skin of fresh cadavers with a dagger. He then observed how much the incision gaped compared with the direction of the wound. Although there are differences between these and the relaxed skin tension lines, or even the so-called lines of minimal tension of Converse, they all follow the same general principles. If incisions are placed in this way, they will produce minimal scarring and the best esthetic results. One also needs to be cognizant of any underlying nerves, particularly the branches of the facial nerve. Incisions made on the oral mucosa are generally full thickness over the mandible and maxilla and go down to bone.
Types of Intraoral Incisions
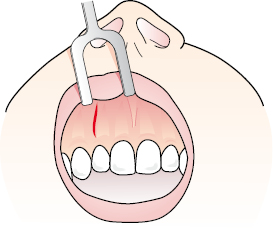
- The straight vertical incision is shown in Figure 6.2, and produces the most esthetic result with minimal scarring. It is indicated for obtaining access to deeper lesions, for tunneling procedures, and for many minimally invasive intraoral procedures. Access, however, is limited.
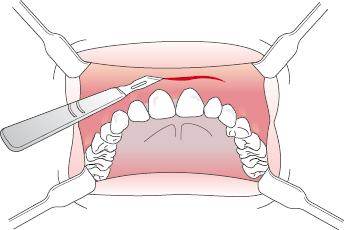
- The straight horizontal incision in the buccal sulcus, as shown in Figure 6.3, is often indicated for management of periapical pathology, impacted teeth, tumors, and sinus procedures. It does, however, tend to produce more scarring than a vertical incision.
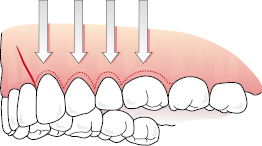
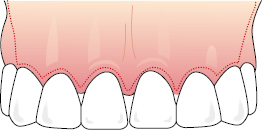
- The intrapapillary incision, sulcular incision, or gingival margin incision is carried out using a scalpel at a reverse bevel and sectioning the interdental papillae and some of the supracrestal and transeptal fibers of the periodontal ligament. It is shown in Figure 6.4 and gives excellent access with minimal scarring and can be used buccally, palatally, and lingually. However, there can be problems around crowns and bridges and it can cause gingival recession, root exposure, and occasionally subsequent gingival problems.
- The gingival margin incision can be combined with a releasing incision at an angle of about 70° to allow improved access to a bony lesion but maintain adequate vascularization of the flap (Fig. 6.5). This is a popular incision, but one disadvantage is that if the releasing incision is made anteriorly, the appearance of the papilla that is included in the releasing incision may become atypical, and the vertical scar produced may be visible on people with smile lines in the esthetic zone which expose the gingiva.
- A releasing incision can be made at each end of a gingival margin incision. The releasing incision should be divergent to protect the vascularity of the flap, particularly in its distal regions, and the further back the releasing incisions are made in the oral cavity, the less they will be visible when the patient smiles (Fig. 6.6). It is a general rule of all soft tissue flaps that the base should be wider than the apex to protect the vascularity.
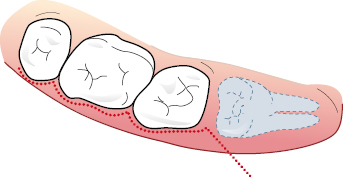
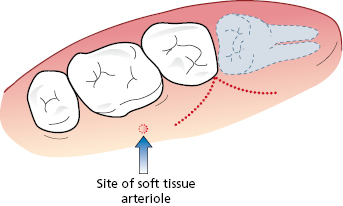
- Incisions for third molars are generally a Winter type incision, which comes down the external oblique ridge to the disto-buccal line angle of the second molar and then continues around the gingival margin of the first and second molar, occasionally with a releasing incision anteriorly if necessary (Fig. 6.7). This gives good access but it can be difficult to suture the papillae and can cause gingival recession on occasions. An alternative incision for third molars runs down the external oblique ridge to the disto-buccal line angle of the second molar and then proceeds as a releasing incision down into the sulcus terminating around the posterior edge of the first molar so as not to encounter a small arteriole which is often present opposite the first molar (Fig. 6.8).
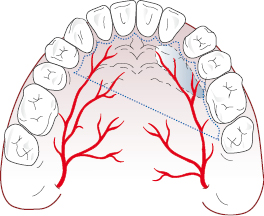
- For lesions such as a palatal torus, a double Y-type incision down to bone is often indicated. This incision leaves a good blood supply for the palatal mucosa and allows excellent access to the torus which can then be removed with a combination of drills and chisels (Fig. 6.9).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


