Periodontics
Learning Outcomes
On completion of this chapter, the student will be able to achieve the following objectives:
• Pronounce, define, and spell the Key Terms.
• Describe the role of the dental assistant in a periodontal practice.
• Explain the procedures necessary for a comprehensive periodontal examination.
• Identify and describe the instruments used in periodontal therapy.
• Describe the role of radiographs in periodontal treatment.
• Describe the indications for and contraindications to use of the ultrasonic scaler.
• Describe the types of nonsurgical periodontal therapy.
• Describe the goals of nonsurgical periodontal therapy.
Performance Outcomes
On completion of this chapter, the student will be able to meet competency standards in the following skills:
• Assist with a dental prophylaxis procedure.
• Demonstrate periodontal charting.
• Assist with gingivectomy and gingivoplasty.
• Prepare and place noneugenol periodontal dressings (expanded function).
• Remove a periodontal surgical dressing (expanded function).
Electronic Resources
![]() Additional information related to content in Chapter 55 can be found on the companion Evolve Web site.
Additional information related to content in Chapter 55 can be found on the companion Evolve Web site.
• Interactive Dental Office Patient Case Studies: Janet Folkner and Louisa Van Doren
• Procedure Sequencing Exercises
• WebLinks
![]() and the Multimedia Procedures DVD
and the Multimedia Procedures DVD
Key Terms
Bleeding index Method of scoring the amount of bleeding present.
Bone augmentation Addition of natural or synthetic bone to a surgical site.
Crown lengthening Surgical procedure to expose more tooth surface.
Curette (kyoo-RET) Surgical instrument used to remove tissue from the tooth socket; also curet.
File A metal instrument of varying size and form with numerous ridges or teeth on its cutting surfaces.
Furcation probe Used to measure horizontal and vertical pocket depths of multirooted teeth in furcation areas.
Gingivectomy (jin-ji-VEK-tuh-mee) Surgical removal of diseased gingival tissues.
Gingivoplasty (JIN-ji-vuh-plas-tee) Surgical reshaping and contouring of gingival tissues.
Gracey curette Curette with one cutting edge, “area specific”; it is designed to adapt to specific tooth surfaces (mesial or distal).
Kirkland knife Double-ended knife with kidney-shaped blades; commonly used in periodontal surgery.
Laser (LAY-zur) Highly concentrated beam of light; acronym for light amplification by stimulated emission of radiation.
Mobility To have movement.
Occlusal trauma Abnormal occlusal relationships of the teeth, causing injury to the periodontium.
Osseous (OS-ee-us) surgery Surgical specialty of removing defects in bone.
Ostectomy (os-TEK-tuh-mee) Surgery involving the removal of bone.
Osteoplasty (OS-tee-oe-plas-tee) Surgery in which bone is added, contoured, and reshaped.
Periodontal (per-ee-oe-DON-tul) charting Commonly accepted notations that are made to the patient’s chart to indicate the condition, position, and restorative history of individual teeth.
Periodontal dressing (Perio Pak) Surgical dressing applied to a surgical site for protection, similar to a bandage.
Periodontal explorer Fine, thin instrument that is easily adapted around root surfaces used to locate deposits of calculus.
Periodontal flap surgery (flap surgery) Incisional surgery performed when excisional surgery is not indicated. In flap surgery, the tissues are not removed but are pushed away from the underlying tooth roots and alveolar bone, similar to the flap of an envelope.
Periodontal plastic surgery Surgical procedures of mucogingival tissues.
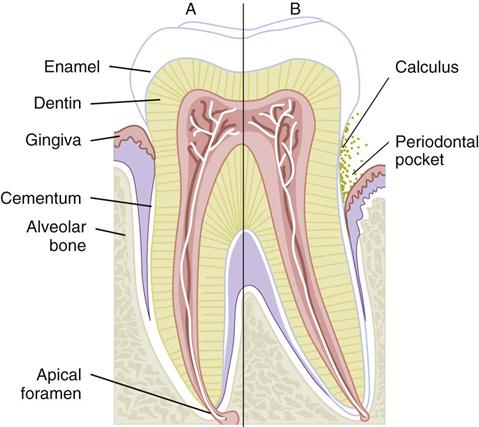
Periodontal pocket Deepening of the gingival sulcus beyond normal; results from periodontal disease.
Periodontal probe Probe used to locate and measure the depth of periodontal pockets; tapered to fit into the gingival sulcus with a blunt or rounded tip.
Periodontics (per-ee-oe-DON-tiks) Dental specialty involved with the diagnosis and treatment of diseases of the supporting tissues.
Periodontist (per-ee-oe-DON-tist) Dentist with advanced education in the specialty of periodontics.
Periotomes Instrument used to cut periodontal ligaments for atraumatic tooth extraction.
Scaling Removal of deposits of calculus deposits from the teeth with the use of suitable instruments.
Ultrasonic scaler Device used for rapid calculus removal; it operates on high-frequency sound waves.
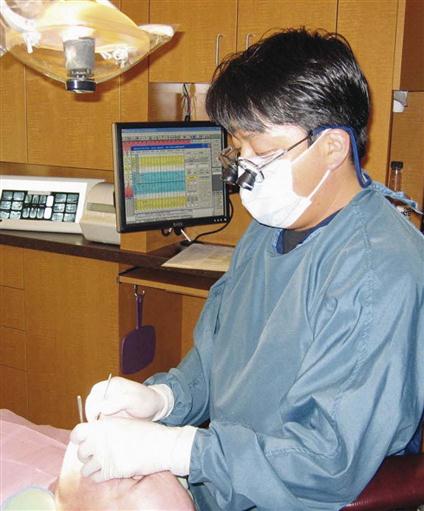
Periodontics is the dental specialty involved in the diagnosis and treatment of diseases of the supporting tissues. The dental assistant in a periodontal specialty office must have a thorough understanding of periodontal diseases and the types of periodontal instruments and procedures. In a periodontal practice, the dental assistant assists with periodontal charting and periodontal surgeries and provides home care instructions to the patient. Depending on the particular state’s dental practice act, the dental assistant also may place and remove periodontal dressings, remove sutures, perform coronal polishes, take impressions for study models, and administer topical fluoride applications.
This chapter focuses on the treatment of patients with periodontal disease and includes a discussion of the instruments used and procedures commonly performed in a periodontal specialty office. It is recommended that you refer to Chapter 14 to review the types of periodontal disease, the associated risk factors, and the systemic factors that influence the progression of periodontal disease.
The Periodontal Practice
Patients are usually referred to a periodontist’s office by a general dentist or a dental hygienist for treatment of a periodontal condition that requires the skill and knowledge of a specialist. After periodontal treatment, the patient will return to the general dentist for routine dental care.
Frequently, a periodontal patient will alternate periodontal maintenance (cleaning and follow-up) appointments between the periodontist’s office and the general dentist’s office. The staff in both offices must coordinate periodontal maintenance therapy between the two practices to provide the most comprehensive care for the patient.
The Periodontal Examination
In addition to a thorough dental examination (see Chapter 28), specialized periodontal examinations are necessary to diagnose periodontal disease and to determine the proper treatment. A periodontal examination includes the patient’s medical and dental history, radiographic evaluation, examination of the teeth, examination of the oral tissues and supporting structures, and periodontal charting.
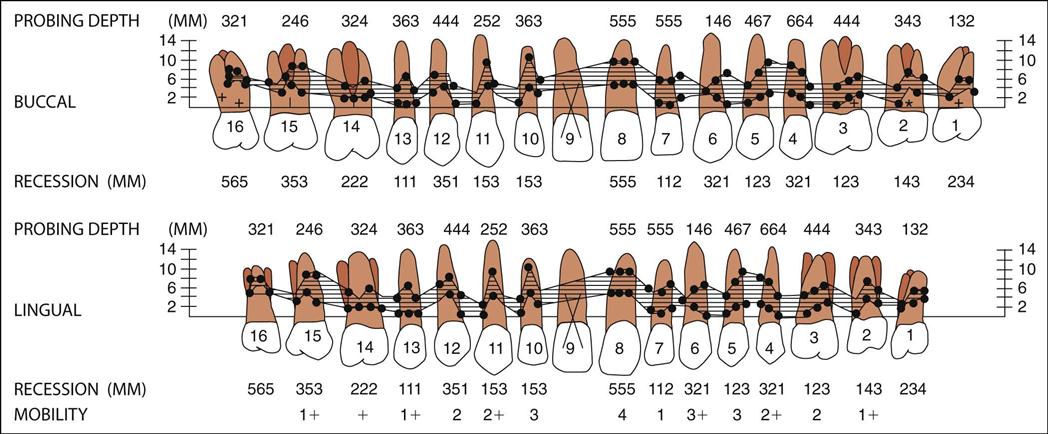
Periodontal charting includes pocket readings, furcations, tooth mobility, exudate (pus), and gingival recession. Clinical findings of the periodontal examination are recorded on the periodontal chart (Fig. 55-1). Software programs are available that provide computerized printouts of periodontal charting data (Fig. 55-2).
Medical and Dental History
The periodontist reviews the medical history to detect any systemic conditions that may influence periodontal treatment. Systemic diseases, such as acquired immunodeficiency syndrome (AIDS), human immunodeficiency virus (HIV) infection, or diabetes, can lower resistance of the tissue to infection. Lowered resistance makes periodontal disease more severe and more difficult to treat.
The dental history is used to gather information about conditions that could indicate periodontal disease. For example, patients with periodontal disease often complain of bleeding gums, loose teeth, or a bad taste. They may describe a dull pain after eating or a burning sensation in the gingival tissue.
Dental Examination
The dental examination focuses on the teeth for indications of periodontal disease or factors that could contribute to periodontal disease (Table 55-1).
TABLE 55-1
Dental Conditions That Contribute to Periodontal Disease
| Condition | Description |
| Pathologic migration | A shift in the position of the teeth is caused by loss of periodontal support. |
| Clenching or grinding (bruxism) | Bruxism places excessive biting forces on the teeth and may accelerate bone loss. |
| Defective restorations or bridgework | Dental prostheses may retain plaque and increase the risk of periodontal disease. |
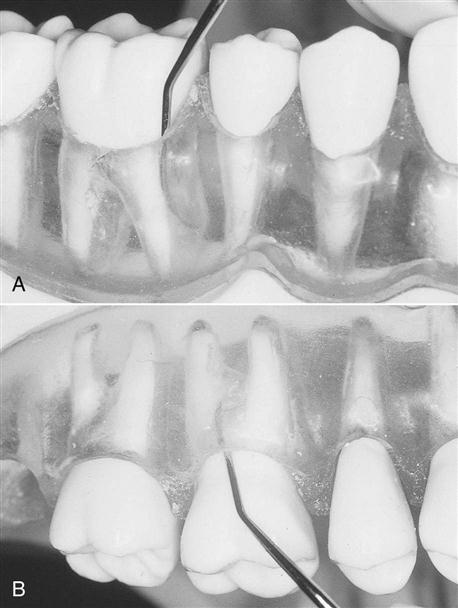
| Mobility | All teeth have some mobility (see Fig. 55-3). Mobility is recorded with the following scale: 0, normal; 1, slight mobility; 2, moderate mobility; 3, extreme mobility. |
| Occlusal interferences | Certain tooth areas can prevent the teeth from occluding properly. These interferences do not directly cause periodontal disease but can contribute to mobility, migration, and temporomandibular joint pain. |
Mobility
Teeth normally have a slight amount of mobility (tooth movement) because of the cushioning effect of the periodontal membranes. However, excessive mobility can be an important sign of periodontal disease (Fig. 55-3).
Oral Tissues and Supporting Structures
The periodontal examination includes an assessment of amounts of plaque and calculus, changes in gingival health and bleeding, and level of bone, as well as detection of periodontal pockets (Table 55-2).
TABLE 55-2
Periodontal Examination of Gingiva and Supporting Tissues
| Assessment | Description |
| Plaque | Plaque is the primary cause of gingival inflammation and most other forms of periodontal disease. |
| Calculus | Calculus is hard mineralized plaque. Calculus may be supragingival (above the gingivae) or subgingival (below the gingivae). Calculus adheres to the surfaces of natural teeth, crowns, bridges, and dentures. It is a contributing factor in periodontal disease because it is always covered with plaque. |
| Gingival recession | As disease progresses, the gingiva may recede, leaving portions of the roots of the teeth exposed below the cementoenamel junction. Gingival recession levels can be visualized on the chart by drawing a dotted or colored line to indicate the gingival margin (see Fig. 55-1). |
| Bleeding index | Severity of gingival inflammation is measured by the amount of bleeding observed during probing. Several different indices are used to measure bleeding. Each system is based on the principle that healthy gingivae do not bleed. |
| Measurement of periodontal pockets | A periodontal pocket occurs when disease causes the normal gingival sulcus to become deeper than normal. (A normal sulcus is 3 mm or less.) |
| Assessment of bone level | Radiographs and probing measurements are used to assess the patient’s bone level. These also may be visualized on the chart by drawing a colored line to indicate the bone level (see Fig. 55-1). |
| Radiographs | Detect interproximal bone loss. Show changes in the bone as periodontitis progresses. Locate furcation involvements. Measure the crown-to-root ratio (the length of the clinical crown compared with the length of the root of the tooth). Show signs of traumatic occlusion. |
Periodontal Probing
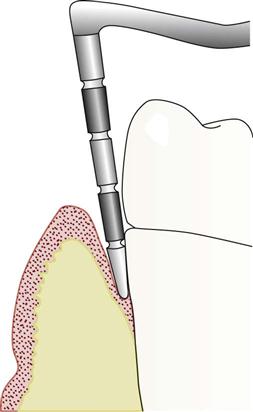
A periodontal pocket occurs when disease causes the gingival sulcus to become deeper than normal. A normal sulcus measures 3 mm or less (Fig. 55-4). The purpose of periodontal probing is to measure how much epithelial attachment has been lost to disease. The greater the depth of the periodontal pocket, the greater is the loss of epithelial attachment and bone, and therefore, the more severe is the periodontal disease (Fig. 55-5).
When periodontal pockets are present, it is very difficult and may be impossible for the patient to keep the pockets clean and free from bacteria and debris. The bacteria in the periodontal pockets will multiply, and, if left untreated, the disease will progress until the tooth is ultimately lost to periodontal disease.
Bleeding Index
The severity of gingival inflammation can be measured by the bleeding index, or the amount of bleeding observed during probing (Fig. 55-6). Several different systems of recording bleeding scores are used. Each system is based on the principle that healthy gingiva does not bleed.
Occlusal Adjustment
The patient’s bite is evaluated for areas of unequal pressure. If excessive biting pressure is noted in a specific area, occlusal trauma can result. Occlusal adjustment, or occlusal equilibration, is a procedure that adjusts the patient’s bite so that occlusal forces are equally distributed over all the teeth. Articulating paper, occlusal wax, stones, and burs are used to adjust the occlusion. Several appointments may be necessary to adjust the occlusion properly.
Occlusal trauma does not cause periodontal pocket formation, but it can cause tooth mobility, destruction of bone, migration of teeth, and temporomandibular joint pain.
Radiographic Analysis
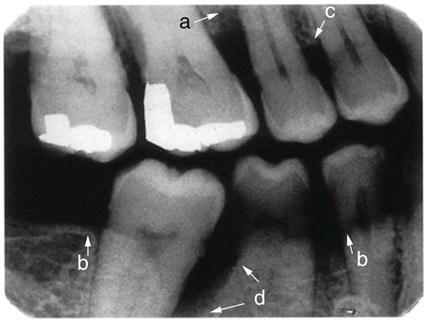
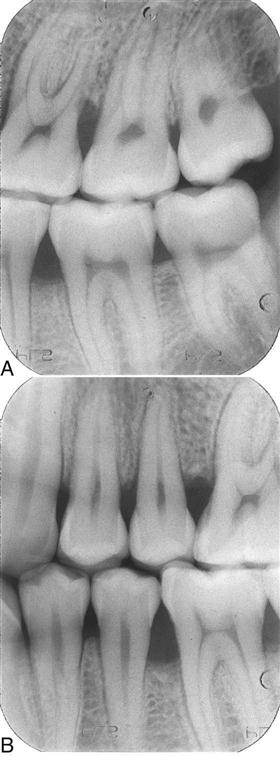
Radiographs are a valuable aid for evaluating periodontal disease. The accuracy of radiographs is critical in the diagnosis of periodontal disease because distortion of the image can result in an incorrect diagnosis (Fig. 55-7).
The bitewing radiograph is particularly valuable because it can accurately depict bone height along the root surface. Vertical bitewing radiographs are excellent for determining the extent of crestal bone loss (Fig. 55-8).
Periodontal Instruments
Periodontal therapy requires the use of specialized instruments to remove calculus, smooth root surfaces, measure periodontal pockets, and perform periodontal surgery. These instruments must be sharp to perform periodontal procedures such as scaling, root planing, and periodontal surgery. In general, the dentist or registered dental hygienist who uses these instruments takes responsibility for maintaining their sharpness.
Periodontal Probes
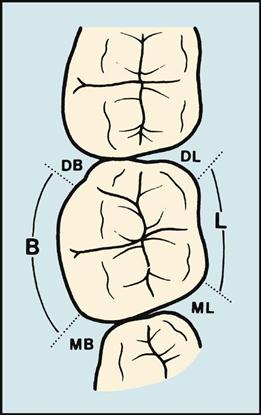
Periodontal probes, which are calibrated in millimeters, are used to locate and measure the depth of periodontal pockets. On some types of probes, the tip is color coded to make the measurements easier to read. The periodontal probe is tapered to fit into the gingival sulcus and has a blunt or rounded tip. Six measurements are taken and recorded for each tooth (Fig. 55-9). Periodontal probes are available in many designs; selection depends on the operator’s personal preference.

Furcation probes are used to measure horizontal and vertical pocket depths of multirooted teeth in furcation areas. They have flat or rounded ends, and may be single or double ended (Fig. 55-10).
Explorers
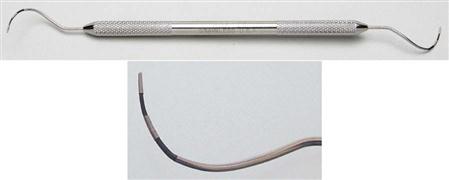
Periodontal explorers are used in periodontics to locate deposits of calculus that may be supragingival or subgingival. Explorers also provide tactile information to the operator about the roughness or smoothness of root surfaces (Fig. 55-11).
Many styles of explorers are used in periodontal treatment. Periodontal explorers are longer and more curved than explorers used for caries detection. (See Chapter 34 for other types of explorers.)
The working ends of periodontal explorers are thin, fine, and easily adapted around root surfaces. They also are long enough to be capable of reaching to the base of deep pockets and furcations. A furcation is the point at which the roots of a multirooted tooth diverge.
Scalers and Files
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses