5 Esthetic Complications and Their Causes
D. Buser, W.C. Martin
5.1 Introduction
Esthetic complications with implant-supported restorations can be either iatrogenic or caused by anatomic factors such as bone or soft-tissue deficiencies. In many patients with esthetic complications, a combination of several factors is present. A thorough understanding of these factors is therefore important to be able to improve esthetic treatment outcomes in daily practice.
Iatrogenic causes of esthetic complications include:
-
Selection of an inappropriate, oversized implant (wide platform)
-
Malpositioned implant entering a danger zone in a coronoapical, mesiodistal or orofacial direction
-
A surgical approach that overstresses the healing capacity of the tissues, leading to the resorption of the facial bone wall
-
Improper use or non-use of provisional restorations to shape the peri-implant soft tissues
-
Inappropriate use of restorative implant components or materials for fabricating restorations
Anatomic causes of esthetic complications include:
-
Horizontal or vertical bone deficiencies at the implant site
-
Vertical bone deficiencies at adjacent root surfaces
-
Implant sites with multiple missing teeth leading to the placement of adjacent implants
For single-tooth replacement, the factor of adjacent implants plays no role and will not be discussed in this Treatment Guide. A separate Treatment Guide will be devoted to this issue.
These factors will be discussed with seven reports on cases with esthetic complications. Each case will be systematically analyzed to improve the reader’s understanding of these problems.
5.2 Case Reports
5.2.1 Patient No. 1
A 20-year-old female patient presented with a compromised esthetic treatment outcome after implant therapy in the anterior maxilla. Figure 1 shows the clinical status 4 months after implant restoration in the area of the right central incisor. The patient presented with a high lip-line situation exposing not only the crowns, but also the gingiva when smiling.

Fig 1 The high lip-line situation clearly reveals the interruption of the harmonious gingival line.
The close-up view shows the full extent of the interruption of the harmonious gingival line by a soft-tissue recession at the implant-supported crown (Fig 2). The gingival recession measures approximately 3 mm and developed rapidly within a few weeks after the insertion of the implant crown.

Fig 2 The detail view illustrates the extent of the gingival recession at the implant crown.
The periapical radiograph reveals the cause for the esthetic failure (Fig 3): The implant shoulder was placed too far apically using an extensive countersinking procedure. In addition, the implant was also malpositioned in a mesiodistal direction, since the implant shoulder almost touched the root surface of the lateral incisor. Both these factors led to bone resorption on the facial aspect of the implant and on the adjacent root surface of the lateral incisor.

Fig 3 Periapical radiograph showing the malposition of the implant in a coronoapical and in a mesiodistal direction.
Figure 4 illustrates the coronoapical implant position in relation to the correct coronoapical implant position for this case. The implant shoulder is located approximately 4 mm apical to the cemento-enamel junction (CEJ) of the adjacent central incisor. The correct distance to the CEJ should only be 1 mm.
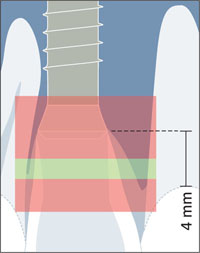
Fig 4 The implant in apical malposition due to excessive countersinking and the close proximity of the implant to the lateral incisor.
The peri-implant “bone saucer” that routinely forms around dental implants after prosthetic restoration can lead to a partial resorption of the facial bone wall and subsequent facial soft-tissue recession when the implant is placed in the apical danger zone, since it has a vertical extension of about 1.5 to 2.0 mm and a horizontal component of 1.0 to 1.5 mm (Buser and coworkers, 2004) (Fig 5).
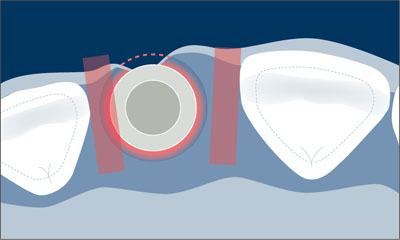
Fig 5 The “bone saucer” (red) causes facial bone wall resorption if the facial bone wall is only 1 mm in thickness.
When the peri-implant “bone saucer” had developed around this particular implant after loading, it added to the resorption of the facial bone wall. As a result, facial soft-tissue recession rapidly developed within a few weeks. The graphic also shows a malposition of the implant shoulder in the mesiodistal danger zone of the adjacent lateral incisor.
Case summary:
The soft-tissue recession of 3 mm was mainly caused by a malposition of the implant shoulder in the coronoapical direction. The complication cannot be resolved by mucogingival surgery. Due to the high lip-line situation of the patient, the only option to resolve the recession is to remove the implant. From a surgical point of view, this is very difficult due to the close proximity of the implant to the lateral incisor. The removal of the implant will not only create a bone defect at the implant site, but also a shortened mesial papilla at the lateral incisor.
5.2.2 Patient No. 2
This 40-year-old female patient was referred with a serious esthetic complication. She presented with a major gingival recession at the implant crown in the area of tooth 12. The main cause of this complication was a severe implant malposition in coronoapical direction. The implant shoulder was positioned about 5 mm apical to the planned soft-tissue margin of the future implant-supported crown. This malposition resulted in severe facial bone resorption and subsequent soft-tissue recession. The use of pink ceramic was necessary to mask the unfavorable esthetic treatment outcome (Fig 6).

Fig 6 Severe esthetic complication with the implant crown at site 12.
The periapical radiograph reveals the apical malposition of the implant that caused the severe esthetic complication (Fig 7).
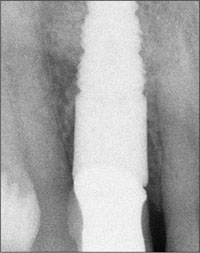
Fig 7 Periapical radiograph demonstrating a well-integrated implant in an apical malposition.
The patient exhibited a mid lip-line situation. When she was smiling, the severe soft-tissue recession was partially covered by the lip (Fig 8).

Fig 8 The patient’s mid lip-line situation masking the compromised treatment outcome.
Case summary:
The severe soft-tissue recession was mainly caused by an extreme apical malposition of the implant shoulder. Due to the mid lip-line situation, the esthetic complication was marginally acceptable to the patient.
5.2.3 Patient No. 3
A 30-year-old female patient presented at the clinic for a consultation to replace a missing tooth (21) lost in a sport accident. Examination of the esthetic risk for her treatment revealed a medium lip line at full smile, exposing three-quarters of the clinical crowns and the tips of the papillae. The gingival biotype was thin, with highly scalloped papillae, tapered clinical crowns, and a thin band of keratinized tissue. The site analysis showed a deficiency in osseous width and height extending apically of the middle third of the adjacent roots (Fig 9).

Fig 9 An attempt to “sound” for osseous support revealed a deficiency in vertical and horizontal bone
The periapical radiograph confirmed this bone loss while showing that adequate bone support existed on the interproximal of the adjacent teeth 11 and 22 (Fig 10).

Fig 10 Periapical radiograph confirming bone deficiencies at the proposed implant site and interproximal support on the adjacent roots.
Based upon the clinical finding/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


