5 Complications
S. Chen, D. Buser
5.1 Complications Following Implant Placement in Post-Extraction Sites
Dental implant therapy is now widely recognized as a predictable treatment option with high survival rates for replacing missing teeth. However, data have been emerging to show that biological, technical, and esthetic complications are frequently encountered in clinical practice (Lang and coworkers, 2004). Many of these complications are caused by patient-related factors beyond the control of the clinician, e.g. the patient’s healing response and level of compliance with oral hygiene and maintenance recalls. However, some complications and implant failures are clearly due to iatrogenic factors (i.e. complications attributable to errors by the clinician). As discussed in Chapter 3.1, the clinician’s role is to assess the patient’s suitability for treatment, to recommend the treatment approach, and to choose the appropriate biomaterials. The clinician is also responsible for carrying out the prescribed treatment to the standard of care necessary to achieve the anticipated outcome. The ultimate responsibility for providing best possible treatment outcome with the least risk and morbidity to the patient therefore rests with the clinician.
Problems and complications are a clinical reality. The clinical cases presented in this chapter highlight the range of problems that can be encountered. The first three cases present post-extraction implants that developed peri-implant infections, of which two occurred soon after placement and one several years later. The next three cases illustrate esthetic problems that occurred following immediate implant placement (Type 1) in the anterior maxilla. In each case, possible etiological factors and treatment options are discussed, and the treatment outcomes are presented.
5.2 Peri-Implant Infection Following Early Implant Placement
L. J. A. Heitz-Mayfield
A 44-year-old female patient was referred to a specialist periodontal practice for assessment and management of pain and soft-tissue swelling associated with an implant at the lower right first molar site (46) (Fig 1).
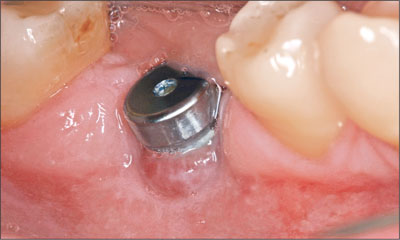
Fig 1 Implant at site 46 with swelling and inflammation of the peri-implant mucosa.
Tooth 46 had been extracted following endodontic treatment and a subsequent fracture. It had been deemed irrational to treat. Approximately 8 weeks following extrac-tion, the dentist placed a 12-mm tapered implant (Nobel-Replace, Tapered Groovy, with a TiUnite surface; Nobel Biocare) using a flapless approach (Figs 2 and 3).
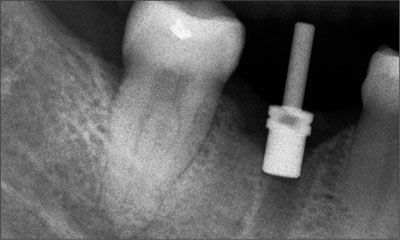
Fig 2 Periapical radiograph 8 weeks following the extraction of tooth 46 at the time of flapless surgery.
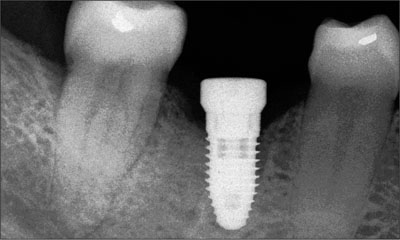
Fig 3 Periapical radiograph taken at the time of implant placement.
The implant was placed early (Type 2) after tooth extraction. Three months following implant placement, the dentist took a periapical radiograph with an impression coping in situ and noted a loss of supporting bone (Fig 4). The healing abutment was replaced and the patient referred to a specialist periodontal practice for assessment.
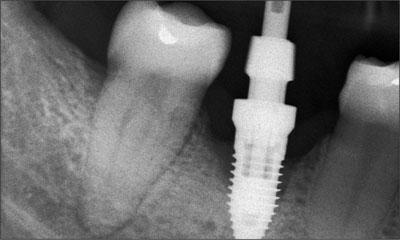
Fig 4 Periapical radiograph of the implant at site 46 showing supporting bone loss.
The patient was a non-smoker with no history of periodontitis. She had been diagnosed with Sjögren’s syndrome by her immunologist and was referred to an oral medicine specialist for the management of dry mouth. She was also assessed for leukoplakia of the oral mucosa, which was subsequently diagnosed as irritative keratosis.
Clinical examination revealed the following clinical and radiographic features:
-
Presence of plaque on all implant surfaces.
-
Bleeding on probing at all implant surfaces.
-
Suppuration.
-
Probing depths: mesiobuccal 4 mm, distobuccal 5 mm, lingual 2 mm, buccal 7 mm.
-
Swelling of the peri-implant mucosa on the facial aspect.
-
Radiographic bone loss. Mesial and distal bone loss 4–5 mm.
-
< 2 mm of keratinized labial mucosa.
The diagnosis was peri-implantitis associated with the implant at site 46. The following treatment options were presented to the patient:
-
Implant removal or
-
Treatment of the peri-implantitis according to Cumulative Interceptive Supportive Therapy protocol (CIST) (Lang and coworkers, 2004)
The patient expressed a strong desire to maintain the implant. Therefore, the second treatment option was chosen (treatment of peri-implantitis), and the patient was informed that the long-term prognosis was doubtful.
The following treatment was provided:
-
Oral-hygiene instructions.
-
Non-surgical mechanical debridement using titanium-coated curettes with local anesthesia.
-
Access flap surgery 3 weeks after non-surgical debridement. Removal of granulation tissue and debridement of the implant surface using titanium-coated curettes. Thorough irrigation and decontamination of the implant surface with sterile saline solution.
-
Systemic antibiotics were prescribed for 1 week – a combination of metronidazole (400 mg three times a day) and amoxicillin (500 mg three times a day).
-
Postoperative chlorhexidine (0.2%) rinses for 4 weeks, twice daily.
-
Weekly follow-up for 4 weeks, followed by quarterly maintenance visits.
At the time of access flap surgery, the absence of the facial bone wall was noted. A circumferential bone crater defect was present (Fig 5). Healing was monitored on a weekly basis for 4 weeks, during which time the patient rinsed twice daily with 0.2% chlorhexidine digluconate solution. At the 1-month follow-up visit, the inflammation and swelling had resolved, and the patient was no longer experiencing any pain. The peri-implant mucosa had receded by 3 mm, exposing the rough implant surface (Fig 6). Oral hygiene instruction was reinforced.

Fig 5 Large facial dehiscence defect visible on flap-reflection.

Fig 6 Clinical photograph of the implant in region 46 taken 3 months following peri-implantitis treatment. Note the mucosal recession of 3 mm.
At the 3-month follow-up visit, there was no bleeding on probing or suppuration and probing depths no longer exceeded 3 mm anywhere. At 5 months after peri-implant surgery, the clinical situation was stable, with shallow probing depths and no bleeding on probing. A periapical radiograph showed some bone regeneration at the mesial and distal aspects of the implant (Fig 7).
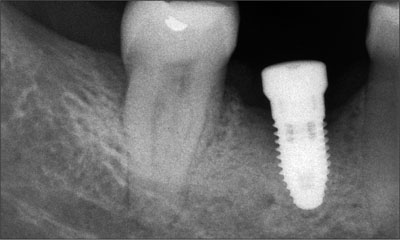
Fig 7 Periapical radiograph of the implant at site 46 taken 4 months after the peri-implantitis treatment.
The patient was then referred back to the referring dentist for the fabrication of a provisional restoration. Monitoring of the peri-implant conditions was to be scheduled over 3 months. At the 12-month follow-up, a decision was to be made as to whether a definitive restoration could be placed, based on the health and stability of the surrounding peri-implant tissues.
Discussion
This complication following early implant placement (Type 2) was likely due to insufficient facial bone at the time of placement, resulting in a facial dehiscence, colonization of the implant surface, and the subsequent development of a peri-implant infection. As no three-dimensional radiographs had been taken pre-operatively, the lack of facial bone available for implant placement had remained undiagnosed (Fig 8). Furthermore, the flap-less approach did not allow for the identification of the missing bone wall and simultaneous bone augmentation.

Fig 8 Diagram showing the missing facial bone wall at the time of early implant placement (Type 2) after tooth extraction (F = facial; L = lingual).
This case highlights the need for adequate preoperative radiographs to assess the available bone volume. It also illustrates the potential problems associated with flapless implant placement when placing an implant into an extraction socket that may not have healed completely.
While peri-implantitis treatment appears to have been successful at the 5-month follow-up, the long-term prognosis for this implant is unknown. A recent 5-year prospective study reported that the treatment of peri-implantitis was only successful in 58% of cases after 5 years (Leonhardt and coworkers, 2003).
Clinical recommendations
Flapless surgery should only be used when all the conditions are favorable for this treatment approach. This includes the following:
Accurate three-dimensional radiographic images of the site to determine the condition of the bone walls and to locate the position of important anatomical structures.
Intact bone walls.
Situations where simultaneous bone augmentation is not required for contour augmentation of the ridge.
Bone sounding to confirm radiographic findings regarding bone walls prior to commencing surgery.
Post-extraction site without infection.
Adequate zone of keratinized mucosa surrounding the implant when placed in a correct restorative position.
The clinician should be experienced in these procedures.
5.3 Loss of an Immediate Implant with Immediate Restoration Due to a Post-Operative Peri-Implant Infection
D. Buser
A 35-year-old male patient was referred to the department for the management of a failed implant at the upper right central incisor site (11). The implant had been placed using an immediate placement (Type 1) and immediate-restoration approach. Simultaneous bone augmentation was carried out at the time of implant placement. Soon after surgery, an infection developed and the implant and provisional crown became loose and had to be removed. There was significant loss of bone at the site. The dentist attempted to regain lost tissue with a bone-grafting procedure, but this was not successful. It was at this juncture that the patient was referred to the department for management.
The patient was healthy, but was a cigarette smoker (12 cig/d). Clinical examination showed that he had a medium lip-line and medium-thick tissue biotype. Site 11 showed a significant tissue defect (Fig 1).

Fig 1 Intraoral facial view of site 11 at the time of presentation. A large ridge defect was noted with a loss of the papilla on the mesial aspect of tooth 12.
There was a loss of vertical and horizontal ridge dimension, and a recession and loss of papilla on the mesial aspect of the adjacent tooth 12. Tooth 21 was endodontically treated and restored with a post-retained crown. Tooth 12 was non-vital. A radiograph taken after the loss of the implant showed a large defect that involved the mesial root surface of the lateral incisor (Fig 2).

Fig 2 Periapical radiograph of site 11 taken after the initial immediate implant had failed. A large osteolytic lesion extended to the mesial surface of the root of tooth 12.
An intraoperative photograph provided by the dentist at the time of bone augmentation showed a large bony defect with a loss of facial and palatal bone (Fig 3).
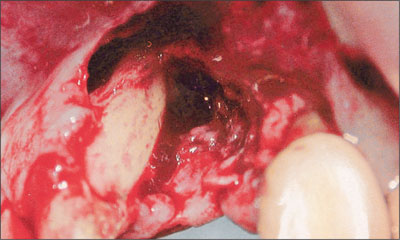
Fig 3 Intraoperative view of site 11 taken at the time of bone augmentation. Note the loss of bone on the mesial aspect of tooth 12.
In addition, the entire mesial surface and apical region of the adjacent tooth were exposed. A post-operative radiograph showed the bone graft and a tack that had been used to stabilize a membrane (Fig 4).
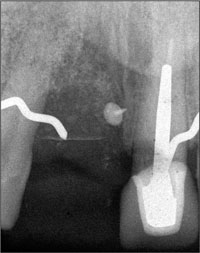
Fig 4 Periapical radiograph taken after bone augmentation, showing a membrane-stabilizing tack in place. The graft subsequently failed.
This graft subsequently failed. A radiograph taken prior to the commencement of implant treatment indicated that teeth 11 and 12 both had normal proximal bone support (Fig 5).

Fig 5 Pre-treatment radiograph showing that teeth 11 and 12 had normal proximal bone support.
The situation was discussed with the patient, and the following issues were highlighted:
-
The prognosis of tooth 12 was hopeless.
-
Due to the large vertical bone defect at site 11, it would be extremely difficult to reconstruct the site so that an implant could later be placed with a good esthetic outcome.
-
Tooth 21 had good bone support and no periapical pathology.
In light of these issues, the following treatment plan was proposed:
-
Extraction of tooth 12 and soft-tissue grafting with a free mucosal graft at site 12 to increase the width of the keratinized mucosa.
-
Early implant placement (Type 2) at site 12 with simultaneous guided bone regeneration at site 12 and a vertical ridge-augmentation procedure at site 11, primarily for soft-tissue support.
-
Reentry after an appropriate healing period.
-
Restoration with a combined implant-tooth-supported fixed dental prosthesis (implant at site 12 and tooth 21).
-
In the event of an unsatisfactory soft-tissue contour in the pontic area at site 11, an additional soft-tissue grafting procedure could be considered.
After obtaining consent from the patient, tooth 12 was extracted without flap elevation (Fig 6).
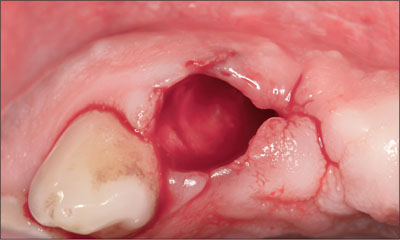
Fig 6 Occlusal view of site 12 after the extraction of the tooth.
A free mucosal graft was harvested from the palate and positioned over the socket and sutured into place (Fig 7).
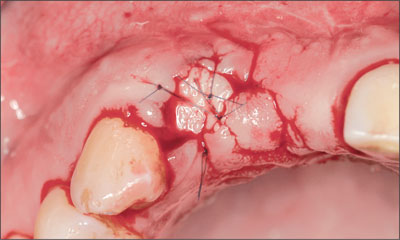
Fig 7 Post-extraction site 12 was sealed with a free mucosal graft.
After 8 weeks, the extraction site had healed (Fig 8).

Fig 8 Site 12 had healed after 8 weeks after extraction. The vertical tissue defect at site 11 was clearly seen.
Facial and palatal flaps were raised to expose the bone and the underlying defect (Fig 9).

Fig 9 Intraoperative view of sites 11 and 12 with a surgical stent in place. Significant loss of vertical bone height at site 11 site was evident on the facial aspect. A similar degree of vertical bone loss was present on the palatal aspect.
A through-and-through defect was found at site 11 with about 5 to 7 mm of vertical bone loss on the facial and palatal walls extending into the nasopalatine canal. A Straumann Standard implant (endosteal diameter 4.1 mm, length 12 mm, Regular Neck prosthetic platform 4.8 mm) with a SLA surface was placed at site 12, using a surgical stent as a guide. The implant shoulder had to be positioned about 3 mm apically of the future mucosal margin as indicated by the stent. With this coronoapical position, most of the microrough SLA surface on the mesial aspect was positioned within bone (Fig 10).

Fig 10 Intraoperative view of the implant at site 12. The mesial aspect of the implant was exposed in the coronal half.
The mesial bone structure was augmented with locally harvested autogenous bone chips (Fig 11). A block of deproteinized bovine bone mineral (DBBM; Bio-Oss Collagen, Geistlich) was used at site 11 to gain bone height (Fig 12).
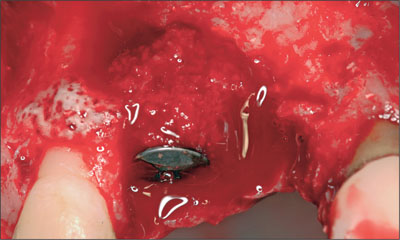
Fig 11 Locally harvested autogenous bone chips were used to cover the exposed implant surface.
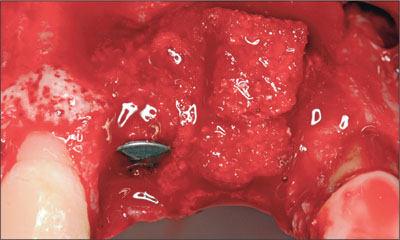
Fig 12 Block of DBBM adapted to site 11 for vertical augmentation.
DBBM granules (Bio-Oss, Geistlich) were used to cover the DBBM block and bone chips on the facial aspect (Fig 13), and covered with a collagen membrane (BioGide, Geistlich) as a barrier (Fig 14).

Fig 13 Particles of DBBM grafted superficially over sites 12 and 11.
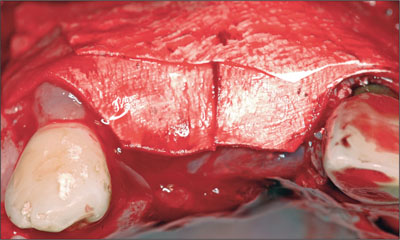
Fig 14 Resorbable collagen membrane, trimmed and adapted over the graft.
To complete the surgery, an incision of the periosteum was applied to allow tension-free primary wound closure (Fig 15).

Fig 15 Tension-free primary wound closure was achieved.
Due to the extended defect, a healing period of 5 months was allowed (Fig 16).

Fig 16 After 5 months, the mucosa was fully healed. Vertical augmentation of the ridge at site 11 had been achieved.
The implant at site 12 was exposed with a punch procedure and a healing cap attached. The patient then commenced restorative treatment. A combined implant- and tooth-supported fixed dental prosthesis (FDP) was fabricated and delivered to the patient (Figs 17 to 19).

Fig 17 Intraoral facial view of a 3-unit metal-ceramic fixed dental prosthesis with mixed tooth (21) and implant (12) support.

Fig 18 3 Extraoral facial view of the completed prosthesis with the patient smiling.
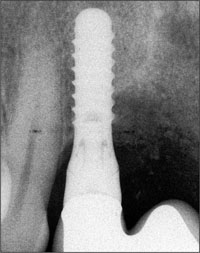
Fig 19 Radiograph of the implant at site 12 and the vertically augmented site 11.
Although the soft-tissue contour in the pontic area was not ideal, the patient decided not to have an additional soft-tissue surgery. The 3-year follow-up examination demonstrated a satisfactory treatment outcome considering the severity of the original status (Figs 20 to 22).

Fig 20 Clinical status at the 3-year examination shows an acceptable treatment outcome with the combined implant- and tooth-supported FDP. The pontic element is slightly too long. Considering the initial status of the edentulous space, the patient was quite pleased.

Fig 21 The patient exhibits a medium smile line.
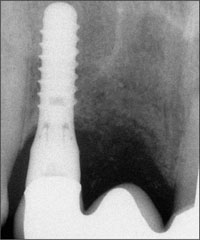
Fig 22 Periapical radiographic at 3 years showing stable bone-crest levels, although the vertical bone level in the pontic area is clearly reduced due to the previous massive infection.
Discussion
This case documents a severe complication of peri-implant infection following immediate implant placement (Type 1) with an immediate restoration. The pre-treatment radiographs showed normal proximal bone support for both teeth 11 and 12. Hence, the loss of tooth 12 was a direct result of the post-operative infection. Several factors may have contributed to the occurrence of this disastrous complication leading to (a) the loss of an adjacent tooth and (b) to the worst clinical situation for a clinician to deal with: a site with two missing adjacent teeth, including a lateral incisor.
The “immediate placement – immediate restoration” approach for single-tooth replacements in the esthetic zone must be considered a complex treatment. Several prospective studies have documented survival rates ranging from 92.5% to 100% (Kan and coworkers, 2003; Locante, 2004; Barone and coworkers, 2006; Degidi and coworkers, 2006). Thus, a proportion of the implants placed with this approach must be anticipated to fail, and the risk is that these implants may be lost with esthetic implications.
The patient is a smoker and is therefore at risk for complications and implant failure (Strietzel and coworkers, 2007). The chosen treatment approach may have over-stressed the healing capacity of the patient.
It was unclear when the implant was removed after the infection first developed. The longer the delay, the more likely it is for an infection to spread to adjacent tissue structures. In this case, the infection must have persisted long enough for the lateral incisor to be involved.
Clinical recommendation
The immediate placement-immediate restoration approach should only be used when all the conditions are favorable. This includes the following low-risk factors:
Healthy, non-smoking patient.
A low-lip situation.
Thick tissue biotype.
Thick facial bone wall at extraction.
Extraction socket without infection.
Single-tooth gap situation.
Favorable occlusion.
The clinician should be experienced in these demanding procedures, allowing a correct three-dimensional implant placement (Buser and coworkers, 2004) with good primary stability using an implant of appropriate shape and dimensions (threaded implant, no wide-platform/wide-neck type implants).
5.4 Peri-Implant Infection Three Years Following Immediate Implant Placement
S. Chen
A 53-year-old female patient was referred to the clinic for the replacement of the lower left second premolar (tooth 35) with an implant-supported crown. The crown on the tooth had fractured, leaving behind the root (Figs 1 and 2).

Fig 1 Preoperative facial view of site 35 showing the retained root. Note the pronounced scallop of the gingival margins on the facial aspect of the teeth.

Fig 2 Preoperative occlusal view of site 35.
The remaining root structure was insufficient to offer a good prognosis for a new post-retained crown. The adjacent teeth had been endodontically treated and restored with post-retained crowns (Fig 3). The patient was healthy and a non-smoker.
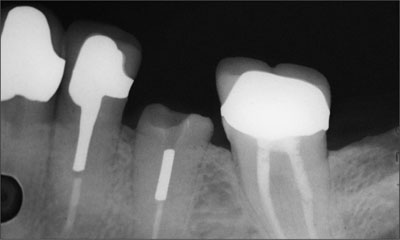
Fig 3 Preoperative radiograph of site 35.
The treatment plan was to extract the root of tooth 35 and immediately place an implant into the socket (Type 1). Following flap reflection, the root of tooth 35 was carefully extracted (Fig 4).
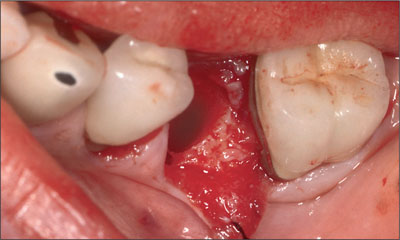
Fig 4 Intraoperative view of site 35 following flap-reflection and the extraction of tooth 35. The vertical height of the facial bone at the mid-point of the socket was lower than at the distal and lingual bone walls.
The facial bone was thin and had a marked scallop with the mid-facial bone located apically of the mesial, distal, and lingual bone walls. The socket was debrided and a Straumann Tapered Effect implant (endosteal diameter 4.1 mm, length 10 mm, Regular Neck prosthetic platform 4.8 mm) with SLA surface was placed (Fig 5).

Fig 5 Occlusal view of the site following the placement of the implant.
The implant was placed with the rough-to-smooth junction at the level of the mid-facial crestal bone (Fig 6).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



