Dental Cements
Learning Outcomes
On completion of this chapter, the student will be able to achieve the following objectives:
• Pronounce, define, and spell the Key Terms.
• Describe luting cements and differentiate between permanent and temporary cements.
• Discuss the factors that influence luting cements.
• List the five cements discussed in this chapter and identify their similarities and differences.
Performance Outcomes
On completion of this chapter, the student will be able to achieve competency standards in the following skills:
• Mix and prepare polycarboxylate for cementation.
• Mix and prepare glass ionomer for cementation.
• Mix and prepare composite resin for cementation.
• Mix and prepare two-paste zinc oxide–eugenol (Tempbond) for temporary cementation.
Electronic Resources
![]() Additional information related to content in Chapter 45 can be found on the companion Evolve Web site.
Additional information related to content in Chapter 45 can be found on the companion Evolve Web site.
• Interactive Dental Office Patient Case Study: Amy Harris
• Procedure Sequencing Exercises
• WebLinks
![]() and the Multimedia Procedures DVD
and the Multimedia Procedures DVD
Key Terms
Dissipate (DI-suh-payt) To cause something to scatter, or become dispersed, and gradually disappear.
Exothermic (ek-so-THUR-mik) Characterized by the release of heat from a chemical reaction.
Luting (LOO-ting) agent Cement-type substance used to seal a surface.
Provisional Referring to temporary coverage made for crown or bridge preparations and worn during cast preparation.
Retard (ree-TAHRD) To slow down a process.
Spatulate (SPACH-uh-layt) To mix using a spatula-type instrument.
Classification of Dental Cements
Dental cements are a category of dental materials that are routinely used when working with indirect restorations. The American Dental Association (ADA) and the International Standards Organization (ISO) have classified dental cements into three types according to their properties and their intended use in dentistry:
• Type II cements involve materials that could be used as a restorative material, such as intermediate restorative material (IRM), which was discussed in Chapter 43.
• Type III cements include the liners and bases that are placed within the cavity preparation. These were discussed in Chapter 44.
Permanent Cements
Permanent cements are luting agents that are used for the long-term cementation of cast restorations such as inlays, crowns, bridges, laminate veneers, and orthodontic fixed appliances. As discussed in Chapter 43, permanent indirect restorations, such as those produced from gold and ceramic, are designed and cast by a dental laboratory technician. Once prepared in the laboratory, cast restorations are delivered to the dentist for the cementation appointment.
Because these types of restorations are seated on a prepared tooth structure, the hollow, shell-like structure of the indirect restoration requires that a luting agent should have qualities that do not interfere with a proper fit (Fig. 45-1).

Temporary Cements
Temporary cementation of an indirect restoration may be completed if the dentist needs to remove the indirect restoration at a later date; if the tooth is sensitive or is exhibiting other symptoms that might require removal of the cast restoration; or when temporary cementation of provisional coverage is required while the patient waits until the laboratory technician completes the cast restoration. Provisional coverage is a temporary coverage that is placed on a tooth to protect the tooth until the permanent restoration is ready to be cemented (see Chapter 51).
Variables Affecting Final Cementation
A number of factors can influence actual cementation with a luting cement. Cementing errors can be the result of improper mixing technique, time, humidity, or incorrect temperature of the glass slab.
Mixing Time
One of the first and foremost rules in the preparation of a cement material is to follow the manufacturer’s directions regarding a material’s exact mixing time, working time, and delivery time. Any delay between completion of the mix and seating of the cast restoration will result in the initial setting process, which could cause the casting not to seat properly.
Regardless of the type of dental cement used, basic guidelines must be followed.
Guidelines for Mixing Dental Cements
Humidity
If the clinical area is warm, or if it is a humid day, premature exposure of the cement to these environmental conditions can create loss of water from the liquid or addition of moisture to the powder. Always dispense the powder first, then the liquid, to minimize the loss of water from evaporation. Wait until it is time to mix the material before placing it on the pad. Do not set it out at the beginning of the procedure.
Powder-to-Liquid Ratio
Incorporating too much or too little powder will alter the consistency of the cement. Be sure to fluff the powder in the bottle before dispensing the powder in the measuring scoop. Always hold the bottle or vial upright to ensure drops of consistent size when dispensing the liquid (Fig. 45-2).
Temperature
Specific types of cement will have a chemical reaction during the setting stage. An example of this is seen when the material zinc phosphate generates heat; this is referred to as an exothermic reaction. In such cases, it is beneficial to cool a glass slab in the refrigerator before mixing the cement. If the glass slab is kept in the refrigerator, make sure to thoroughly wipe the slab dry before dispensing the material, so as not to incorporate any moisture condensation into the material.
Types of Cement
The cements described in this chapter are designed to be versatile in their properties, uses, and mixing techniques. Many of the cements that were traditionally used for routine cementation through the 1990s have been replaced by newer makeup and mixing techniques. The selection of cement for a specific procedure requires knowledge of the chemical and physical properties of each particular cement type for the specific restorative process to be performed.
Glass Ionomer Cement
Glass ionomer cement is one of the most versatile types of cement used in dentistry. Glass ionomer cements are a hybrid of silicate and polycarboxylate cements. This type of cement adheres to enamel, dentin, and metallic materials. Glass ionomer cements are supplied in special formulations according to their use.
• Type I is used for the cementation of metal restorations and direct-bonded orthodontic brackets.
• Type II is designed for restoring areas of erosion near the gingiva, as discussed in Chapter 43.
• Type III is used as a liner and dentin-bonding agent, as discussed in Chapter 44.
Glass ionomer cement has the following benefits, which account for its popularity:
• The cement causes less trauma or shock to the pulp than is caused by many other types of cement.
• The cement has low solubility in the mouth.
• The cement adheres to a slightly moist tooth surface.
• The cement has a very thin film thickness, which is excellent for ease of seating a casting.
• Glass ionomer cements can be formulated for use as a dentin substitute or base material.
Chemical Makeup of Glass Ionomer Cement
Application
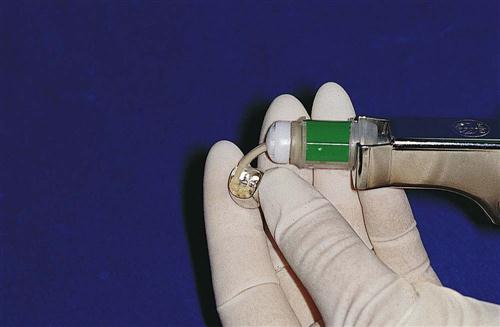
Glass ionomers are available as a self-curing or light-cured formula. The cements are supplied in bottles of powder and liquid, which can be mixed manually on a paper pad or a cool, dry glass slab. Use of the glass slab increases the working time of the cement. Glass ionomer material is also supplied in premeasured capsules, which are triturated and expressed through a dispenser (Fig. 45-3). These capsules have the advantages of (1) being more convenient to use, (2) requiring less mixing time, and (3) producing consistent mixes because of the controlled powder-to-liquid ratio. See Procedure 45-1.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses