4
The role of orthodontics
- Be aware of the indications for pre-surgical orthodontics in orthognathic patients.
- Understand the objectives of pre-surgical orthodontics.
- Be aware of the scope and limitations of pre-surgical orthodontics.
- Understand the role of orthodontic appliances in the peri-operative period.
- Be aware of the scope and limitations of orthodontics in the immediate post-operative healing phase.
- Understand the objectives of post-surgical orthodontics.
- Be aware of the advantages and disadvantages of carrying out surgery before orthodontics.
- Be aware of the possible indications for carrying out surgery without adjunctive orthodontics.
- Be aware of the common complications associated with orthodontic treatment in orthognathic patients.
4.1 Introduction
Orthodontic treatment is usually an integral part of contemporary orthognathic treatment. In most cases, the attainment of a satisfactory post-surgical occlusion will require the use of fixed appliances to achieve optimal arch coordination and inter-digitation. As explained in Chapter 3, the magnitude of surgical jaw correction that can be achieved is, to a large extent, dictated by the size of the overjet (positive or negative), which often needs to be adjusted through carefully planned incisor decompensation. It also stands to reason that the stability of the surgical jaw correction should be assisted by a well inter-digitated occlusion.
Whilst many patients seeking orthognathic surgery report concerns regarding their facial aesthetics, a large proportion are also unhappy with the appearance of their teeth. The ideal alignment that modern fixed appliance treatment can achieve helps to deliver optimal dental aesthetics as part of the overall treatment outcome.
It is logical to consider the role of orthodontics in three stages: before surgery (pre-surgical); just before and during surgery (peri-operative); and after surgery (post-surgical).
4.2 Pre-surgical orthodontics
The tooth movements required to prepare a patient for surgery should be carefully planned in all three planes of space, with reference to the patient in the clinic as well as appropriate diagnostic records. It is essential to carefully document the orthodontic plan in a way that can be readily referred to as treatment progresses.
4.2.1 Factors affecting incisor decompensation
Most orthognathic patients will have developed a degree of incisor compensation as a result of their disproportionate jaw growth (see Chapter 2). One of the main aims of pre-surgical orthodontics is to reverse these compensations. The tooth movements required vary with the type of malocclusion. In class II, division 1 cases the lower incisors typically need to be retracted from a proclined position, whilst in class III cases they need to be proclined. In the upper arch, the opposite movements will generally be needed. The notable exceptions to this are class II, division 2 malocclusions, where the upper incisors require proclination from their retroclined pre-treatment positions.
Complete decompensation of the incisors involves correction of their inclinations to their respective cephalometric norms, which is often appropriate. However, as stated in Chapter 3, there are also situations where partial decompensation is desirable and this must be agreed at the planning stage so that the orthodontist has clear goals. The main factors that influence incisor decompensation are as follows:
- Crowding and spacing of the teeth.
- Previous extractions.
- Soft tissue resistance.
- Magnitude of surgical jaw movements.
- Mandibular plane angle.
- Type of maxillary surgery.
- Quality of the planned occlusion.
- Limiting factors.
Crowding and spacing of the teeth
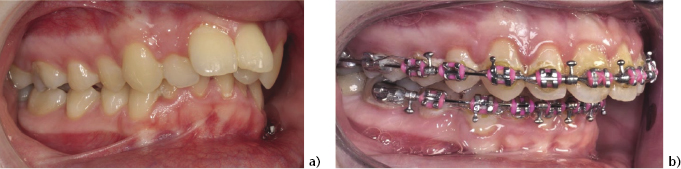
Space is required for incisor retraction and crowding assists proclination. Figure 4.1 illustrates how decompensation is largely facilitated by the presence of crowding, in a class III case where the lower incisors are retroclined. Conversely, in a class II case where the lower incisors are proclined and there is no spacing, extractions will be necessary to allow decompensation (Figure 4.2). For these reasons, the ideal amount of decompensation may not always be easy to achieve.
Figure 4.1 Class III orthognathic typodont model showing: (a) Compensated and crowded lower incisors, and (b) the proclining (decompensating) effect of incisor alignment.
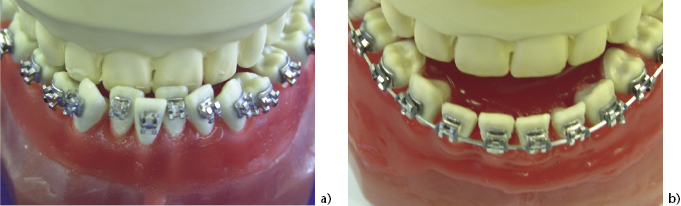
Figure 4.2 Class ll, division 1 patient. (a) The lower incisors are proclined and mildy crowded, with no space for retraction. (b) Pre-molar extractions have allowed lower incisor decompensation.
In class III cases the amount of lower incisor proclination that will be achieved as a result of crowding should be assessed. As a general rule, each millimetre of lower arch crowding will produce approximately 0.5mm of labial movement of the incisal edges, in the midline. Equally, in a class II case, where retraction of the lower incisors is required, each millimetre of space will allow 0.5mm of lingual movement.
Previous extractions
Previous extractions in either the upper or the lower dental arch can present a problem in the execution of decompensation. For example, in a class II case such as that shown in Figure 4.3, the lower incisors are proclined, but the patient has previously lost lower premolars as part of earlier fixed appliance treatment. Decompensation, through incisor retraction, will therefore be difficult, since further extractions are not an ideal option. Conversely, in the severe class III malocclusion shown in Figure 4.4, there has been previous loss of both lower first premolars and subsequent extreme retroclination of the lower labial segment. The spacing in the lower dental arch will make proclination of the incisors difficult without re-opening space for prosthetic tooth replacement.
Figure 4.3 Class II occlusion (a) with lower incisor compensation and previous loss of both lower first premolars and complete space closure (b).
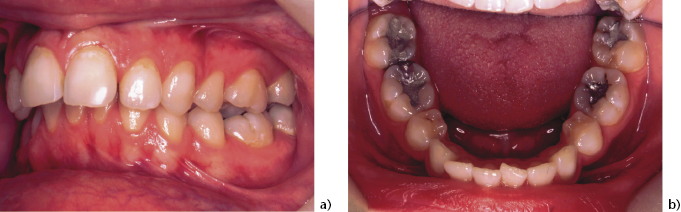
Figure 4.4 Class III patient with severe lower incisor compensation and previous loss of both lower first premolars leaving residual spaces.

Soft tissue resistance
Teeth have to be moved within their soft tissue envelope and the lower lip and tongue may offer resistance to the proclination and retraction of incisors. This problem is likely to increase with the severity of the jaw discrepancy and, in class III cases, will also depend on the muscular tone of the lower lip. There are also the constraints of the alveolar bone which, in non-growing patients, is of limited adaptability. Careful anchorage management is required to ensure that the crowding or spacing in the lower arch translates into the planned amount of incisor movement.
Magnitude of surgical jaw movements
As explained in Chapter 3, one of the main functions of pre-surgical orthodontics is to create an overjet (class II patients), or reverse overjet (class III patients), that will allow the desired amount of surgical jaw correction. If it is not possible to adequately decompensate the incisors then the patient will be left with a residual jaw discrepancy after surgery. Equally, excessive decompensation will result in surgical over-correction. Setting a ‘target (reverse) overjet’ is therefore helpful for the orthodontist and, if this is proving difficult to achieve, it is advisable to take the patient back to the planning clinic for a review of the treatment objectives.
Mandibular plane angle
In patients where the mandibular plane angle (to Frankfort Plane or horizontal reference plane) is predicted to be outside its normal range following surgery, consideration should be given to adjusting the lower incisor inclination, such that it will add with the mandibular plane angle to approximately 120° after surgery (see also Chapters 2 and 3 and Figure 3.5).
Type of maxillary surgery
Where the provisional surgical plan is to differentially impact or down graft the maxilla, there will be a corresponding change in the inclination of the upper incisors. For example, where posterior impaction is planned, the incisors will retrocline relative to the Frankfort Plane (or horizontal reference line). This should be compensated for by modifying the extraction pattern, or adding torque to the archwire (see also Chapter 3).
Quality of the planned occlusion
Incisor inclination directly affects the quality of the buccal segment occlusion that can be achieved in orthognathic patients, because proclined incisors occupy more space in the dental arch than upright or retroclined incisors. In class II cases, incomplete decompensation will tend to result in a class II molar relationship when the check models are hand occluded with the incisors in class I (Figure 4.5). In class III cases the opposite will tend to be true, although mild compensation of the incisors generally produces quite a pleasing occlusion.
Figure 4.5 Class II case following mandibular advancement surgery, where the buccal segment occlusion is still class II, due to under-torquing of the upper incisors.

Whilst the correct torque and tip of the incisors are important in achieving an ideal occlusion, the orthodontist must also be aware of tooth-size discrepancies. Most commonly, disproportionately small upper lateral incisors can result in class II buccal segment relationships and a decision has to be made to either accept this compromised occlusion or leave space around the lateral incisor for build-up to the correct size.
Limiting factors
It is important to recognise the scope and limitations of incisor decompensation for each patient and these should inform the orthodontic planning process, as outlined in Chapter 3. Decompensation should not be planned simply to attain cephalometrically ‘normal’ incisor inclinations, which may not necessarily be appropriate, or achievable, for an individual patient.
4.2.2 Control of incisor decompensation
The inclination of the upper and lower incisors can be controlled orthodontically to help achieve the planned degree of decompensation, using the following methods:
- Extraction pattern.
- Bracket prescriptions.
- Mechanics.
Extraction pattern
Where compensation has resulted in significant incisor proclination, extractions will usually be required to retract them to the desired position. Typically, this will apply to lower incisors in class II cases and upper incisors in class III cases. As a general rule, the further forward the extractions are in the dental arch, the more incisor retraction will result. For example, extraction of first premolars will generally allow more decompensation than extraction of second premolars.
Bracket prescriptions
Pre-adjusted edgewise fixed appliances have first-order (in-out), second-order (tip) and third-order (torque) adjustments built into the individual brackets. The amount of ‘torque’ in the incisor brackets controls their inclination and therefore contributes to the delivery of decompensation during pre-surgical orthodontics. Different appliance prescriptions have different torque values for the upper and lower incisors and so may be more or less suitable as aids to decompensation.
The MBT™ prescription.
One of the most common currently used prescriptions, MBT™, has negative torque in the lower incisor brackets and increased torque in the upper incisor brackets, which is aimed primarily at conserving anchorage in the orthodontic camouflage treatment of class II malocclusions. This prescription is advantageous in the pre-surgical preparation of class II cases, where retraction of lower incisors and the maintenance of a large overjet are required. However, in class III cases it will tend to be disadvantageous, limiting lower incisor proclination and maintaining upper incisor proclination.
Individual adaptations.
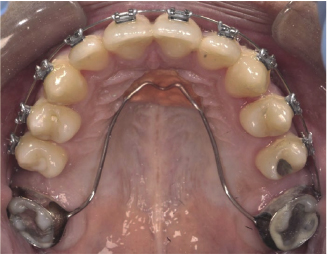
Whilst some clinicians may opt for customised prescriptions to ensure that the brackets are working in sympathy with their treatment goals in all cases, it is possible to make certain adaptations that can help to overcome some of these problems. For example, the torque values of the lower incisor brackets can be changed from − 6° to + 6° by inverting them, which will help to procline the lower incisors in a class III case with minimal crowding (Figure 4.6). In addition, incisor inclinations can be adjusted by introducing third order bends into stainless steel rectangular archwires.
Figure 4.6 In this class III case with an absence of lower incisor crowding, the lower MBT™ incisor brackets have been inverted to convert 6° of lingual crown torque to 6° of labial crown torque to encourage incisor proclination.

Mechanics
In addition to the effects of the extraction pattern and the appliance prescription, there are also a number of intra- and inter-arch mechanical techniques available to the orthodontist to control the incisor positions:
Intra-arch mechanics.
Resistance of unwanted mesial movement of upper posterior teeth can be increased by using anchorage reinforcement devices, such as trans-palatal arches. They exert their effect by maintaining the inter-molar width and, in the case of the Nance arch, also engaging the mucosal surface of the anterior palatal vault (Figure 4.7).
Figure 4.7 Example of a Nance palatal arch in a class lll orthognathic patient requiring upper incisor retraction along with first molar extractions. Anchorage reinforcement of the second molars is acheived by a combination of maintaining inter-molar width and resisting tipping by engaging the anterior palatal vault with the acrylic button.
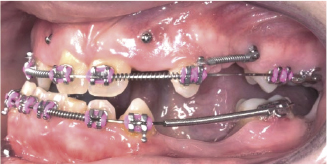
Temporary Anchorage Devices (TADs) are mini screws that are placed in the alveolar bone to offer points of absolute anchorage from which to apply traction. They can provide direct or indirect anchorage for mesio-distal and vertical tooth movements, either by being placed buccally between the roots of the upper first molar and second premolar, or palatally to reinforce a trans-palatal arch (Figure 4.8).
Figure 4.8 This orthognathic patient, who also has hypodontia, has a number of mini bone screws or Temporary Anchorage Devices (TADs) inserted in strategic positions to provide absolute anchorage for tooth movements that might otherwise be difficult to acheive. (Courtesy of Dr Lucy Chung.)
Inter-arch mechanics.
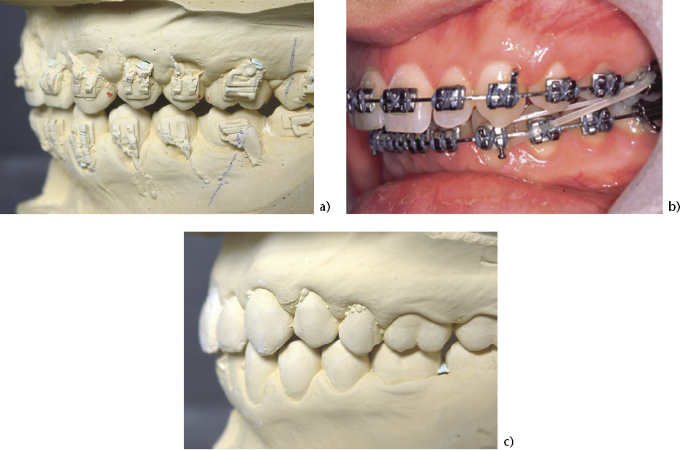
Inter-maxillary elastics can be used to apply traction between upper and lower fixed appliances. Wearing these requires good patient compliance but they allow at least small adjustments to the overjet, or reverse overjet, when the intra-arch methods of anchorage control have been exhausted. Figure 4.9 shows a class II case in which the occlusion on the first set of check models during pre-surgical orthodontics was not ideal, due to inadequate decompensation. The incisor inclinations were then adjusted, using class III elastics, producing an improved inter-digitation of the buccal segments.
Figure 4.9 (a) These check models, taken for a class II patient during pre-surgical orthodontics, revealed that the buccal segment occlusion would be class II, due to incomplete incisor decompensation. (b) Inter-maxillary traction with class III elastics, aimed at retroclining the lower incisors and proclining the uppers enabled class I buccal segments to be achieved in the final result (c).
4.2.3 Vertical tooth movements
Patients with extreme vertical jaw disproportions will usually have developed accentuated curves of Spee. In anterior open bite cases this will tend to affect the upper arch, whilst in deep bite cases it tends to affect the lower arch (see Chapter 2). One of the treatment objectives for orthognathic patients should be to level the dental arches for an optimal occlusion. In planning pre-surgical orthodontics, the following factors must be taken into account:
Limitations of orthodontic mechanics
There is a limit to the amount of levelling that orthodontic appliances can achieve through tooth movement alone, particularly in a non-growing patient, and attempting orthodontic levelling of extreme curves is unlikely to be successful. In the lower arch this may be partly due to the fact that deep overbite cases tend to be accompanied by heavy bite forces, which resist the molar extrusion that normally contributes to overbite reduction.
Where pre-surgical levelling of the lower arch is required (see also ‘Lower anterior face height’ below) the use of utility arch wires, which bypass the premolars to apply an intrusive force to the incisors using molar tip-back bends, may be effective during the early stages of treatment. When continuous arch mechanics are required, modern reverse-curve nickel-titanium arch wires can be useful in maintaining a prolonged levelling force along the length of the arch.
Stability
In anterior open bite cases with a significant curve in the upper arch, orthodontic levelling will involve extrusion of the incisors to some extent and there is a risk that this may relapse after surgery. In such cases, the alternatives to pre-surgical levelling are two-fold:
Figure 4.10 This patient is planned for segmenta/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


