Chapter 4
Scaling and Root Planing
INTRODUCTION
Ever since Loe demonstrated the role that plaque plays in the development of gingivitis (Loe et al., 1965; Theilade et al., 1966) there has been an emphasis on plaque removal as the primary goal of non-surgical periodontal therapy. With the confirmation that microorganisms are involved in the initiation and progression of periodontal infections, studies have examined the efficacy of various modalities of treatment to eliminate or suppress these microorganisms and reverse the inflammatory changes or damage to the periodontium. Manual scaling and root planing (SRP) are considered the basis of periodontal treatment and as such are often the control to which other modalities are compared. This chapter provides an evidence-based understanding of what can and cannot be achieved with scaling and root planing and how its effectiveness can be optimized.
Scaling refers to the removal of hard and soft deposits from the crown and root surfaces. Root planing denotes the removal of cementum and dentin that is rough or impregnated with bacteria, endotoxins, and calculus to produce a root surface that is smooth and hard. SRP can be performed as either a closed or open procedure. An open procedure differs from a closed one in that it denotes reflection of the gingival tissues, allowing direct visualization of the root surface — this is also known as surgical scaling.
The general purpose of SRP is to reduce or eliminate plaque-associated gingival inflammation (Figure 4.1). Specifically, this is achieved by mechanical instrumentation of the affected root surfaces. The result of this instrumentation is a reduction of bacterial plaque via disruption and/or removal of the microbial biofilm, the removal of accretions from the root surface, and ultimately a shift in the ecology of the pocket from one that favors disease to one that is conducive to health.
Instruments that can be used for scaling can be either manual or power-driven. Power-driven types can be sonic or ultrasonic, rotating instruments such as fine-grained diamonds, reciprocating instruments represented by the Profin Directional System, or lasers. The most commonly used and studied instruments for mechanical debridement are manual scalers and sonic or ultrasonic scalers.
INSTRUMENTATION
Manual Scalers
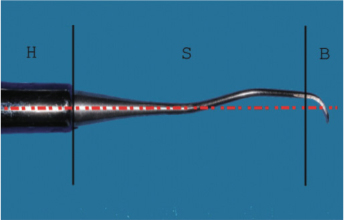
All manual instruments have three sections: (1) the handle, (2) the shank, which can have bends, and (3) the working end or blade (Figure 4.2). The various scalers differ primarily in the number and angle of bends at the shank, and the shape, curvature, and number of cutting edges at the blade. There are five major classifications: sickle, curette, file, hoe, and chisel. The most commonly used are the sickle and curette. The design of a sickle scaler enables it to be used effectively for supragingival calculus removal, while curettes are better suited for subgingival application.
The working end of a sickle scaler is triangular in cross-section, coming to a point at the tip. The blade faces up and is angled 90 degrees to the terminal shank with cutting edges on both sides of the face. This shape facilitates removal of heavy calculus and access to the area associated with the gingival embrasure and the proximal contact, which can be quite narrow. It is also very useful as an initial instrument to remove large, heavy deposits of supragingival calculus, thus improving access to the subgingival areas with the curettes. While sickle-type scalers are very effective at supragingival sites, they are not designed to be used at subgingival sites because the sharp tip can easily traumatize gingival tissues and gouge the root surface. Furthermore, the blade shape does not adapt well against the often concave, subgingival root anatomy (Figure 4.3).
Accessing the complex subgingival anatomy and minimizing damage to the delicate sulcular tissues is better achieved with curettes. Curettes are subdivided into two types, universal and Gracey. The main difference is that Gracey curettes are area specific; this specificity is realized via differences in the working ends. Gracey curettes have bends in the shank to facilitate access to either of the four sides of a tooth: mesial, distal, oral, or facial. In addition, the face of the blade is angled down 120 degrees to the terminal shank and only the lower side of the blade is sharpened. Thus, the Gracey 11/12 curette is designed to scale only the mesial surfaces of molars and premolars, while the Gracey 13/14 is specific to the distal surfaces (Figure 4.4). On the other hand, the universal curettes are not area-specific; the same instrument can be used anteriorly or posteriorly and for any of the four sides of the tooth. This is because both sides of the blade are sharpened and the angle of the face to the terminal shank is 90 degrees (Figure 4.5). Neither is objectively better than the other and thus operator preference based on an understanding of the instrument’s design and the dental anatomy being scaled determines which instrument is best for any particular circumstance.
Figure 4.1. One month follow-up demonstrating resolution of gingival inflammation after scaling and root planing.

Figure 4.2. Scaler design. H: handle, S: shank, B: blade. Note that the blade is centered to the handle for ideal force transmission.
Power-driven Scalers
Power-driven scalers are classified as either sonic or ultrasonic; the ultrasonic variety are sub-classified as magnetostrictive or piezoelectric. They are broadly distinguished according to the type of tip movement and tip vibration frequency. The sonic scalers operate at low frequencies ranging from 3,000 to 8,000 cycles per second (Cps) with a tip movement that is generally orbital, while both types of ultrasonic scalers operate at much higher frequencies. The magnetostrictive range is from 18,000 to 45,000 Cps with an elliptical tip movement, while piezoelectric units have a Cps in the 25,000 to 50,000 range and a tip movement that is generally linear.
Figure 4.3. Contrast between the sharp tip of a sickle scaler (above) and the rounded toe of a curette (below).

Figure 4.4. Series of Gracey scalers from left to right: 1/2 (anteriors), 11/12 (mesial of posteriors), and 13/14 (distal of posteriors). Note the increasing angle of bends in the shank to allow access to more posterior sites.
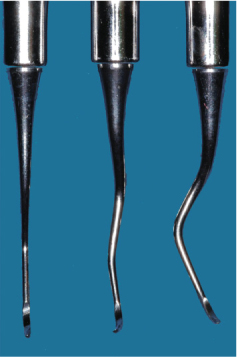
Figure 4.5. Key differences in blade design between universal and Gracey curettes. Universal: the face of the blade is 90 degrees to the shank (red dotted line) with both sides sharpened (arrows). Gracey: the face is angled 120 degrees to the shank (red dotted line) with only the lower side of the blade sharpened (arrow).

Sonic and ultrasonic instruments were originally only used for supragingival plaque, calculus, and stain removal. They were found to leave an uneven root surface, and thus it was thought that manual root planing was required following ultrasonic scaling to smooth the root surface. Over the years, there have been many modifications in the instruments, including smaller tip diameters, longer working lengths, different angles, and diamond coatings. These developments, along with a better, evidence-based understanding of the root surface alterations, has allowed powered scalers to be used safely and effectively in deep subgingival probing depths and difficult anatomy such as furcations, without having to be supplemented with subsequent manual instrumentation.
It should be noted that manual and sonic/ultrasonic scalers are used in a very different manner. The blade of a curette is inserted within the sulcus apical to the deposit at the base of the pocket. The calculus is then engaged and removed as the scaler is pulled coronally out of the sulcus. On the other hand, sonic and ultrasonic scalers engage the deposit at its coronal extent. The instrument is inserted within the pocket like a dental probe, with the working end parallel to the root surface and the tip pointing into the sulcus. Calculus is removed with multiple, light apically directed strokes. It is beyond the scope of this chapter to discuss how each instrument is used and maintained. However, it should be understood that all scalers are technique sensitive. It is critical that the clinician be fully aware of an instrument’s design and its proper use because incorrect application of a scaler will result in poor calculus removal and damage to the root surface or gingival tissues.
Manual vs. Power-driven Scalers
The advances in ultrasonic and sonic instrument design and the expansion of their use to subgingival sites has resulted in a body of literature that compares their effectiveness with hand scalers. These studies have examined the efficacy of the debridement to bring about improvements in clinical endpoints such as probing depth and bleeding on probing, as well as shifts in the microbiological profile of the sulcus. Researchers have also considered alterations to the root surface and whether there is any advantage with powered scalers in accessing difficult anatomy or reducing the time required to effect this debridement.
Clinical Endpoints
Generally, the studies show that there is no statistical difference in clinical endpoints such as reduction in bleeding on probing, pocket depth reduction, attachment level gain, and reduction in sites with plaque (Loos et al., 1987; Badersten et al., 1984; Copulos et al., 1993; Boretti et al., 1995; Laurell and Pettersson, 1998). The reduction in probing depths with sonic or ultrasonic instruments ranges from 1.2 mm to 2.7 mm (Drisco et al., 1996). This compares favorably with the reductions achieved with manual scalers of 1.29 mm to 2.16 mm (Cobb, 1996). The microbiological changes are related to the clinical outcomes. Here, as well, there does not appear to be a clear difference between the two types of debridement; both treatments result in similar shifts in the microbial flora (Baehni et al., 1992; Oosterwaal et al., 1987).
Access to the Base of the Pocket or Difficult Anatomy
In relation to the similarity in clinical and microbiological endpoints achieved, it should be noted that in their systematic review, Tunkel et al. point out that most studies comparing powered and manual scaling are either done on single-rooted teeth or they group the results of single-and multi-rooted teeth, and that more research is required to assess the efficacy of powered instrumentation on multi-rooted teeth (Tunkel et al., 2002). In this regard there is evidence that suggests that ultrasonic instruments have an advantage over hand scalers for the debridement of furcations (Leon et al., 1987; Oda et al., 1989). These studies have found that both types of instruments are equally efficacious in Class I furcations, but in Class II and III situations the ultrasonic scalers are more effective. If one considers that anatomical studies have found that the entrance to a furcation is often smaller than the width of a curette (Bower, 1979), then it is not surprising that specialized ultrasonic tips with widths of 0.55 mm or less would have an advantage (Figure 4.6).
Figure 4.6. The smaller tip size of an ultrasonic scaler (left), designed for access into a furcation, contrasted with a curette (right).

Other modifications of ultrasonic tips are designed to allow improved penetration into the base of deep pockets. These tips, which are slimmer and probe-like in shape, can reach closer to the base of the pocket (0.78 mm) than manual curettes (1.25 mm) (Dragoo, 1992). This result was confirmed recently by Barendregt et al., who also found that ultrasonic tips penetrated deeper, particularly in moderate (4 mm to 6 mm) and severe (≥ 7 mm) pockets (Barendregt et al., 2008).
In both of these papers, the greater penetration depth for ultrasonic scalers was on untreated periodontitis patients. The relevance of this point is highlighted by the Barendregt paper, which found that unlike the results observed for the periodontitis group, the maintenance group (less inflamed gingival tissue) showed equal penetration depth for manual curettes and ultrasonic instruments. It is likely that in the periodontitis group some of the greater depth reached by the ultrasonic scaler could be explained as ingress of the ultrasonic tip through the epithelial attachment and into the connective tissue. This has been observed when using a periodontal probe to measure pocket depth in inflamed tissues where the difference in probing depths between treated and untreated pockets amounted to approximately 1.2 mm (Fowler et al., 1982). Even if all of the deeper access cannot be explained by connective tissue invasion, it has yet to be established if greater penetration translates to improved calculus and plaque removal.
Where studies have shown clear differences is in the time required to clean the root surface. A review of the evidence indicates that manual instrumentation takes 20% to 50% longer to achieve the same clinical results as with powered scaling (Cobb, 1996).
Surface Roughness and Cementum Removal
Since the introduction of sonic/ultrasonic instruments there have been investigations to determine if these instruments remove less or more root surface than hand scalers, as well as the smoothness of the resultant surface. Recent evidence suggests that ultrasonic scalers remove less cementum (Vastardis et al., 2005; Ritz et al., 1991) but leave a rougher surface than curettes (Kocher et al., 2001; Schlageter et al., 1996). However, as will be discussed later, the clinical significance of a rougher surface has yet to be elucidated. Irrespective, sonic and ultrasonic instrumentation can result in excessive cementum removal if used improperly. Increasing instrument pressure, contact time, or tip to tooth angle can all cause more root damage. In this regard it has been suggested that the ultrasonic scaler be used at low or medium power with multiple, light overlapping strokes and with the tip angled parallel to the root surface (Flemmig et al., 1997). The importance of light strokes is underlined by a study which found that increasing the application force from 0.3 N to 0.7 N resulted in a twofold increase in root surface loss (Jespen et al., 2004).
Summary
In general, studies have found that a comparison of clinical endpoints shows manual and power-driven instruments to be equally effective. Thus, if the desired therapeutic outcome is reduction in inflammation, reduction in probing depth, and removal of root surface accretion, then either manual or powered instruments can be used. Despite these findings, powered scalers demonstrate some advantages, particularly with respect to time efficiency and access to challenging root anatomy. It remains to be seen if continued advances in tip design and ultrasonic energy generators will further improve the efficacy of these instruments.
SCALING AND ROOT PLANING
Objectives
As indicated above, effective scaling and root planing can be achieved by either powered or manual instrumentation. Although advances in technology may engender advantages to one instrument or the other, the focus of the therapy emains constant: the primary objective of mechanical non-surgical therapy is the removal of bacterial plaque from the tooth surface. This is affected by removal of the soft microbial biofilm on the root surface as well as the hard accretions or calculus that harbor bacteria within their structure. With this mechanical reduction or disturbance of the microbial community, we expect resolution of the inflammatory changes in the tissues of the periodontium, which in turn precipitate a change in the local environment of the sulcus from one that supports inflammatory destruction to one that is conducive to the maintenance of periodontal health.
To gain a holistic understanding of mechanical non-surgical therapy we need to consider not only the response of the periodontium to our hygiene efforts but also the factors that modify this response. In this way we can better optimize our results as well as understand the limits of and limitations on this form of therapy.
Changes in Clinical Endpoints
The most common endpoints used to evaluate the clinical outcome of mechanical therapy are probing pocket depth and clinical attachment level. Although there is only a weak correlation between bleeding on probing and continued disease activity (Lang et al., 1990), decreases in the percentage of bleeding sites continue to be considered a surrogate indicator for the resolution of gingival inflammation. In this regard it is useful to note that collectively, studies investigating all forms of mechanical therapy show reductions in gingival inflammation by 45% in 4-mm to 6.5-mm pockets (Cobb, 2002). In addition, this resolution of inflammation is affected largely by su/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


