Chapter 4
Dentofacial Infection
Introduction
Inflammation, infection, and pus formation were first described in Egyptian papyri. Inflammation is a reaction of the tissues to irritation as in an invasion by pathogenic microorganisms. These reactions tend to destroy and limit the spread of infectious agents and repair the damaged tissues. The inflammatory process involves fluid and cellular exudates in an attempt to destroy and engulf the invading microorganism.
Dentoalveolar Abscess
The acute dentoalveolar abscess is a localized suppurative inflammation which involves the teeth and the supporting periodontal structures (Fig. 4.1). The pathogenic microorganisms, which are predominantly anaerobes, normally gain entry to the periapical tissue through the necrotic pulp of carious teeth or via the gingival crevice of the periodontal ligament. The most typical clinical features are severe pain and exquisite tenderness on percussion or touching the tooth during mastication. The pain is due to the local release of inflammatory mediators such as kinins and histamines, and fluid exudates causing increased pressure in the confines of the underlying alveolar bone. Pyrexia and lymphadenopathy can be common symptoms associated with this infection. Prompt evacuation of pus by either extracting the tooth or removing the infective pulp reduces the internal pressure and the patient’s pain.
The fate of the acute dentoalveolar abscess depends on the number and the virulence of the invading microorganisms, as well as the resistance of the patient. The spread of the infection will be governed by the position of the tooth in the alveolus and relationship of the apices of the infected teeth to muscle attachments and their relative proximity to the lingual and buccal surfaces of the jaw bones.
Infection originating from a dental abscess may spread to involve the deeper tissues of the head and neck region, once the abscess has broken through the surface (usually buccally) of the alveolar bone. On the other hand, the invading microorganisms may be destroyed by the natural local resistance of the body, prescription of antibiotics, and removal of the source of infection by extraction or endodontic means. The lesion would then resolve. However, in some instances, lack of appropriate treatment may lead to the development of a chronic dentoalveolar abscess where the lesion never heals by itself but persists as a lesion of low-grade virulence, characteristic of the typical granuloma. Chronic dentoalveolar abscesses and periapical granulomas are generally asymptomatic unless, or until, reignited in an acute phase. Only the development of an acute exacerbation would lead to the cardinal signs of inflammation such as tenderness, pain, redness, and swelling. Sinus formation, either intraorally or extraorally, is not an infrequent feature of this chronic infection. The chronic lesion has the potential to stimulate epithelial cells and initiate the development of a dental cyst.
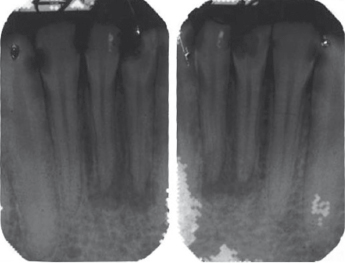
Radiographic Appearance
In the acute phase, the earliest changes are thinning of the periodontal space followed by loss of apical lamina dura, then radiolucency with ill-defined margins. Chronic abscesses or apical granuloma are usually associated with a well-circumscribed radiolucency.
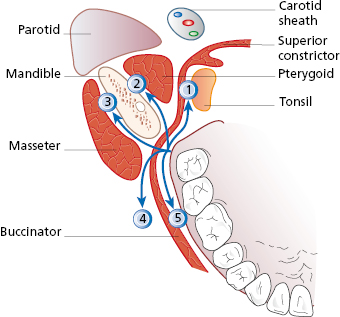
Site and Spread of Infection
Bone, muscle, aponeurosis or fascia, neurovascular bundles, and skin, can act as barriers against spread of infection. However, none of these tissue barriers or boundaries is so restrictive or containing that they necessarily prevent the spread of infection into contiguous anatomic spaces (Fig. 4.2). The following are the most common routes for the spread of infection from dentoalveolar infections:
- upper lip;
- canine fossa;
- infraorbital region;
- buccal space (5 in Fig. 4.2);
- palate;
- submasseteric (3 in Fig. 4.2);
- retropharyngeal;
- lateral pharyngeal (1 in Fig. 4.2);
- pterygomandibular space (2 in Fig. 4.2);
- infratemporal fossa;
- parotid space;
- buccinator space (4 in Fig. 4.2);
- suprahyoid region:
- submandibular space;
- submental space;
- sublingual space.
Upper Lip
Infection at the base of the upper lip originates from the upper anterior teeth. It spreads on to the orbicularis muscle from the labial sulcus between the levator labii superioris muscle and the levator angularis oris muscle.
Canine Fossa
Spread of infection to the canine fossa usually originates from maxillary canine or upper premolar teeth, often presenting above the buccinator muscle attachment. These swellings obliterate the nasolabial fold (Fig. 4.3).

This space is in close proximity to the lower eyelids, and therefore early management is mandatory to avoid circumorbital infection. There is a risk of spread cranially via the external angular vein which may become thrombosed.
Buccal Space
The attachment of the buccinator muscle to the base of the alveolar process can control the spread of infection in the region of the mandibular and maxillary molars. The infection spreads intraorally superficial to the buccinator muscle in front of the anterior border of the masseter muscle. Therefore the clinical manifestation of the infection of this space is characterized by swelling confined to the cheek (Fig. 4.4). However, infection may spread superiorly towards the temporal space, inferiorly to the submandibular space or posteriorly into the masseteric space. In some cases infection may spread to the surface of the skin, leading to fistula formation (Fig. 4.5).

Palate
The palate is usually involved by infection originating from the maxillary lateral incisor or the palatal roots of the posterior teeth. The infection spreads from the apices of these teeth, perforating the palatal alveolar bone, and pus accumulates below the palatal mucoperiosteum (Fig. 4.6). Since the tissue is tightly bound down in this area, infection at this site is often very painful. It is important to be aware that, although the lateral incisor is the commonest source of palatal abscess, most lateral incisor abscesses present labially.

Pterygomandibular Space
Infection in this space is manifested by trismus due to the involvement of the pterygoid muscles. This space is bounded medially by the medial pterygoid muscle and laterally by the medial surface of the mandible, anteriorly by the pterygomandibular raphe, and posteriorly by the deep lobe of the parotid gland. The lateral pterygoid muscle forms the roof of this space (Fig. 4.7).
Submasseteric Space
The commonest source of infection in this space is from lower third molar pericoronitis. This space is bound laterally by the masseter muscle and medially by the outer surface of the ramus of the mandible (Fig. 4.8). It is in direct communication with the lateral pharyngeal space posteriorly. The temporalis muscle divides the superior part of this space into two portions – the superficial temporal space, which is bounded by temporalis muscle medially, and the deep temporal space with the temporalis muscle laterally and the periosteum of the temporal bone medially. Severe trismus due to spasm of the masseter muscle is a characteristic feature of involvement of this fascial space.
Infratemporal Space
Extension of infection from maxillary molars can pass into this space. Infection may also spread from the pterygomandibular, parotid or lateral pharyngeal region to the infratemporal space. The patient then complains of pain, particularly with mouth opening, some dysphagia, and difficulty with lateral mandibular movements. This space is located behind the zygomatic bone posterior to the maxilla and medial to the insertion of the medial pterygoid muscle. The infratemporal space is bounded superiorly by the greater wing of the sphenoid and is in close proximity to the inferior orbital fissure with a possible risk of spread of infection to the orbit.
Parotid Space
Involvement of this space may be an extension of infection from the middle ear or the mastoid region. Infection from the masseteric or the lateral pharyngeal space may also spread to the parotid region. Therefore, the most characteristic feature of involvement of this space is swelling of the parotid gland region below the ear lobe. This space contains several important structures which may be affected by infections. These include the 7th cranial nerve, auriculotemporal nerve, facial vein, the parotid lymph node, and, more deeply, the external carotid with its branches.
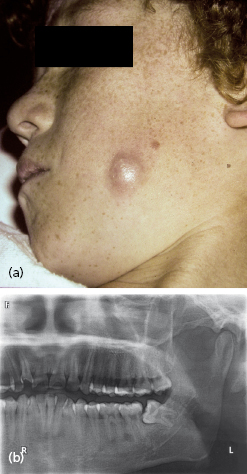
Submandibular Space
This space is located below the mylohyoid muscle, medial to the ramus and body of the mandible. It is bounded anteriorly by the attachments of the anterior belly of the digastric muscle and posteriorly by the posterior belly of digastric muscle and stylomandibular ligament. Infection from the posterior mandibular teeth may pass lingually below the attachment of the mylohyoid muscle into this space. Clinically, swelling of the submandibular regions tends to obliterate the angle of the mandible, causing pain and redness of the skin overlying this region. Dysphagia is usually a marked symptom (Fig. 4.9).

Submental Space
This space lies between the two anterior bellies of the digastric muscle. Anteriorly and laterally this space is bounded by the body of the mandible (Fig. 4.10). It is contained superficially by the platysma muscle and deeply and superiorly by the mylohyoid muscle. The infection of this space usually arises from mandibular anterior teeth where the infection perforates the lingual cortex; swelling of the submental region is a characteristic clinical feature. The skin over the swelling is stretched and hardened, and the patient experiences considerable pain and difficulty with swallowing. The infection may progress buccally causing swelling in the labial sulcus and over the chin.

Sublingual Space
Infection spreads into this space as the result of perforation of the lingual cortex above the attachment of the mylohyoid muscle. This space is bounded superiorly by mucous membrane and inferiorly by the mylohyoid muscle. The genioglossus and geniohyoid muscles form the medial boundary. Laterally, this space is bounded by the lingual surface of the mandible. Infection in this space will raise the floor of the mouth and displace the tongue medially and posteriorly. The tongue displacement may compromise the airway and immediate intervention may be required. Dysphagia and difficulty in speech are also common.
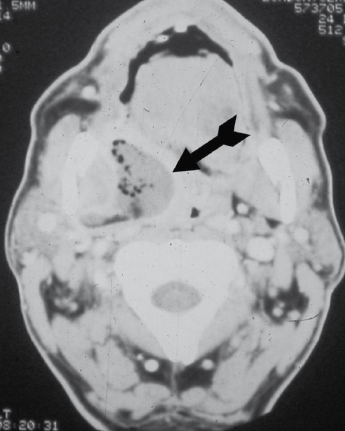
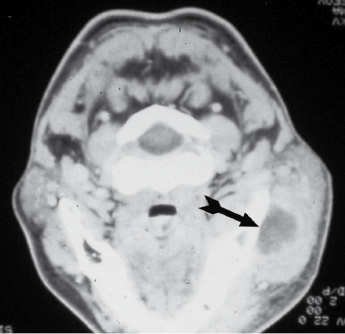
Pharyngeal Space
This space is located on the lateral side of the neck, bounded medially by the superior constrictor muscle of the pharynx and posterolaterally by the parotid space. Infection in this space may originate from mandibular molars or third molar pericoronal suppuration. This could also be a site of spread of infection from the parotid space or fascial space around the body of the mandible. The lateral pharyngeal space contains the carotid sheath, glossopharyngeal nerve, accessory nerve, and the hypoglossal nerve, as well as the sympathetic trunk. Therefore, spread of infection into this space carries the significant danger of spread into a descending neck infection and involvement of the mediastinum. Clinically, stiffness of the neck, swelling of the lateral wall of the pharynx, medial displacement of the tonsils, dysphagia, and trismus are among the characteristic clinical features of involvement of this space (Fig. 4.11).

Retropharyngeal Space
This space is located between the posterior wall of the pharynx and the prevertebral fascia. This space is in direct communication with the base of the skull superiorly and the mediastinum inferiorly. It has the same characteristic clinical features as infection of the lateral pharyngeal space and carries the significant complication of a descending neck infection.
Microbiology of Dental Infections
There is usually a polymicrobial cause for oral/dental infection comprising facultative anaerobes, such as viridans group streptococci and the Streptococcus anginosus group, with predominantly strict anaerobes, such as anaerobic cocci, Prevotella and Fusobacterium species. The use of sophisticated non-culture methods has identified a wider range of organisms such as Treponema species and anaerobic Gram-positive rods such as Bulleidia extructa, Cryptobacterium curtum, and Mogibacterium timidum.
Management of Patients with Orofacial Infection
The management of orofacial infection involves surgical intervention to drain localized pus and medical support for the patient.
- Incision and drainage. This could be carried out either intraorally or extraorally depending on the location of the infection (Fig. 4.12). Aspiration of pus prior to incision allows a more accurate sampling method as it reduces contamination and helps preserve anaerobic bacteria. Fluctuation of the swelling indicates the presence of pus and is defined as fluid transmission using bi-digital palpation.
- Antibiotics. Antibiotics can be provided empirically or a specific antibiotic given based on culture and sensitivity tests. Penicillin has the potential to be the first-line agent in the treatment of odontogenic infections. Most other beta-lactam antibiotics, including fourth-generation cephalosporins, are not found to have greater effectiveness than penicillin. />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


