38
Bone augmentation: graft materials
The autogenous bone graft with its biological properties (osteogenicity, inductivity, conductivity) has long been considered the ideal grafting material in bone reconstructive surgery. Recent advances in biotechnology have provided the surgeon with access to a great variety of bone grafting materials, i.e. osteobiologics, in order to reduce the morbidity and unpredictable resorption of autogenous bone graft (Hallman & Thor, 2008). Trends suggest that the survival rate of dental implants in grafted zones may be slightly lower than the survival rate of implants placed in native bone (Tonetti & Hammerle, 2008; Esposito et al., 2009).
Autogenous Bone Graft
The grafted bone can be regarded as a scaffold for new bone formation. The vascular supply of cortico-cancellous bone graft enables the survival of cells, the diffusion of nutrients, and revascularization (Davies & Hosseini, 2000). The healing events involve osteoconduction (new bone is gradually formed around the resorbed graft) and osteoinduction (release of proteins stimulating osteoblasts to form new bone).
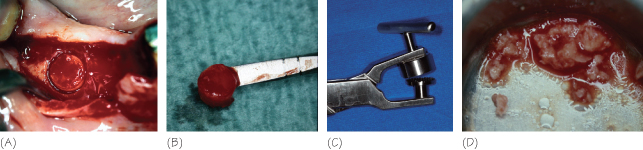
Positive outcomes have been reported in sinus floor augmentation (Boyne & James, 1980). Rigid fixation of block bone graft is a prerequisite for stimulating the progenitor cells. Particulate or chip bone grafts with/without substitutes and non-resorbable membranes are alternatives (Fig. 38.1).
Figure 38.1 Autogenous bone (A,B) Bone is harvested at the donor site with a trephine. (C,D) Bone is ground in a bone mill.
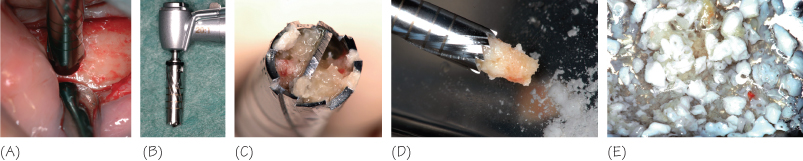
Autogenous bone grafts can be mixed with any of the materials listed below (Fig. 38.2).
Figure 38.2 Autogenous bone plus xenograft (A–C) Bone is harvested with a trephine mill system. (D,E) The retrieved bone is collected, and may be blended with a bone substitute.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


