Anesthesia and Pain Control
Learning Outcomes
On completion of this chapter, the student will be able to achieve the following objectives:
• Define, pronounce, and spell the Key Terms.
• Discuss the importance of pain control in dentistry.
• Describe the composition and application of topical anesthetics.
• Discuss the composition and application of local anesthetic agents.
• Describe nitrous oxide/oxygen sedation and its use in dentistry.
• Discuss the importance of reducing the dental team’s exposure to nitrous oxide.
Performance Outcomes
On completion of this chapter, the student will be able to meet competency standards in the following skills:
• Demonstrate the placement of a topical anesthetic agent.
• Demonstrate the preparation and management of the local anesthetic setup.
• Assist during the administration of local anesthesia.
• Assist in the administration and monitoring of nitrous oxide/oxygen sedation.
Electronic Resources
![]() Additional information related to content in Chapter 37 can be found on the companion Evolve Web site.
Additional information related to content in Chapter 37 can be found on the companion Evolve Web site.
![]() and the Multimedia Procedures DVD
and the Multimedia Procedures DVD
Key Terms
Analgesia (an-ul-JEE-zee-uh) Stage of anesthesia in which the patient is relaxed and conscious.
Anesthesia (an–es-THE-zhuh) Temporary loss of feeling or sensation.
Anesthetic Medication that produces temporary loss of feeling or sensation.
Aspirate (AS-pi-rayt) To draw back or to draw within.
Diffuse (di-FYOOZ) To spread from an area of high concentration to one of low concentration.
Duration (duh-RAY-shun) Time from induction to complete reversal of anesthesia.
Gauge Standard dimension or measurement of the thickness of an injection needle.
Induction (in-DUK-shun) Time from injection to effective anesthesia.
Innervation (in–ur-VAY-shun) Supply or distribution of nerves to a specific body part.
Lumen (LOO-men) The hollow center of the injection needle.
Oximetry (ok-SIM-uh-tree) Measurement of oxygen concentration in the blood.
Permeate (PUR-mee-ayt) To spread or flow throughout.
Porous (POR-us) Describes an object with minute openings that allow the passage of gas or fluid.
Systemic toxicity (sis-TEM-ik tok-SIS-i-tee) Related to a system, or typically the entire body.
Tidal volume Amount of air inhaled and exhaled with each breath.
Titrate (TYE-trayt) To determine the concentration of a substance.
Vasoconstrictor (vay-zoe-kun-STRIK-tor) Type of drug that constricts (narrows) blood vessels; used to prolong anesthetic action.
A wide variety of anxiety and pain control procedures have allowed the dental profession to extend oral healthcare to millions of individuals who would otherwise remain untreated. Anesthesia is the term used for temporary loss of feeling or sensation, and anesthetics are the drugs that produce the temporary loss of feeling or sensation.
Anxiety and pain control is defined as the practice of various psychological, physiologic, and chemical approaches to the prevention and treatment of preoperative, operative, and postoperative anxiety and pain. Methods of pain control used in dentistry to alleviate or reduce anxiety and pain include the following:
Topical Anesthesia
The primary purpose of topical anesthesia in dentistry is to provide a numbing effect in a specific area where an injection is to take place. Topical anesthetic agents provide a temporary numbing effect on nerve endings located on the surface of the oral mucosa. The drugs in topical anesthetics are concentrated to allow penetration of the mucous membranes and action at the nerve endings.
Topical anesthetic agents are available in the form of ointments, liquids, sprays, and patches, with each form having a slightly different application process (Fig. 37-1). For today’s products, an ointment type of topical anesthetic should remain on the site of injection for a minimum of 15 to 30 seconds and a maximum of 1 to 2 minutes to have optimum effectiveness.
Spray topical anesthetic agents are applied to larger surface areas of the oral tissues. These anesthetics are useful when they are applied at the back of the throat in patients with a strong gag reflex when an impression or intraoral radiographs are taken. It is noted that topical sprays could pose a potential danger if too much is administered. Because topical anesthetics are prepared in a higher concentration, the anesthetic would be absorbed into the bloodstream, causing an overdose reaction to the anesthetic.
The topical patch is a new product that when placed provides topical anesthesia within 10 seconds. The patch is used for injections and for alleviation of discomfort from denture sores and oral ulcers (Fig. 37-2). See Procedure 37-1.
Local Anesthesia
Local anesthetics were first discovered in the mid-1800s and have greatly reduced pain during dental care. Local anesthetic agents are the most frequently used form of pain control in dentistry. This method of pain control provides a safe, effective, and dependable method of anesthesia of suitable duration for virtually all forms of dental treatment.
Characteristics of Local Anesthetics
• Nonirritating to the tissues in the area of the injection
• Associated with minimal toxicity (cause the least possible damage to body systems)
• Rapid onset (take effect quickly)
• Able to provide profound anesthesia (completely eliminate the sensation of pain during a procedure)
• Sufficient duration (remain effective long enough for the procedure to be completed)
• Sterile or capable of being sterilized by heat without deterioration
Method of Action
Local anesthesia is obtained by injecting an anesthetic solution near a nerve, where treatment is to take place. The local anesthetic agent temporarily blocks the ability of the nerve membrane to generate an impulse. When this anesthetic solution attaches to specific receptors within the nerve, it slows down neuron conductance, causing the patient to feel numbness in that area.
After the injection is completed, the anesthetic diffuses, or spreads, into the nerve and blocks its normal action. To obtain complete anesthesia after the injection, the nerve must be sufficiently permeated by a concentration of the anesthetic base to inhibit conduction in all fibers. The action of local anesthesia is reversed as the bloodstream carries away the solution.
Chemical Composition of Anesthetics
Local anesthetic solutions for dental use come under two chemical groups: amides and esters. The amides were first introduced into clinical practice in the 1940s and have maintained the standards by which all other local anesthetics are measured. Ester-type anesthetic solutions are used primarily as topical anesthetics. The difference between the two groups can be seen in how they are metabolized by the body. Amide local anesthetics are metabolized by the liver, and ester local anesthetics are metabolized primarily in the plasma.
Each local anesthetic cartridge contains a combination of the following ingredients:
Time Span of Anesthetics
An important consideration for the dentist when a local anesthetic is chosen is the time span of pain control required. Induction is the length of time from injection of the anesthetic solution to complete and effective conduction blockage. Duration is the length of time from induction until the reversal process is complete. Depending on the procedure, the dentist will select a local anesthetic agent on the basis of its duration (Box 37-1), as follows:
Vasoconstrictors in Anesthetics
To slow down the intake of an anesthetic agent and increase the duration of action, a vasoconstrictor is added to a local anesthetic agent. When a vasoconstrictor is used:
• Blood vessels to the site of administration are constricted.
• Absorption into the cardiovascular system is slowed.
• Bleeding at the injected area is decreased, which is especially important for surgical procedures.
Major vasoconstrictors used with local anesthetic agents include epinephrine, levonordefrin, and Neo-Cobefrin. A very small quantity of vasoconstrictor is added to the local anesthetic solution in the ratio of vasoconstrictor-to-anesthetic solution of 1 : 20,000; 1 : 50,000; 1 : 100,000; or 1 : 200,000. With the concentration levels of a vasoconstrictor, the smaller the ratio, the higher the percentage of vasoconstrictor. In most situations, it is desirable to use as high a ratio as possible.
Contraindications to Vasoconstrictors
Because a vasoconstrictor may cause strain on the heart as the local anesthetic solution is absorbed into the body, the use of an anesthetic solution without a vasoconstrictor is recommended for patients with a history of heart conditions. Such conditions include unstable angina (heart-related chest pain), recent myocardial infarction (heart attack), recent coronary artery bypass surgery, untreated or uncontrolled severe hypertension (high blood pressure), and untreated or uncontrolled congestive heart failure.
The vasoconstrictor action may interact with those of other drugs the patient is taking. Therefore, the dental team must be aware of the patient’s current medication intake and always must update and communicate any changes in the patient’s medical history.
Before you prepare a syringe, you should always check with the dentist as to the type of local anesthetic solution to be given and the desired vasoconstrictor-to-anesthetic solution ratio. See Box 37-1 for the types of routinely used dental anesthetics.
Injection Techniques
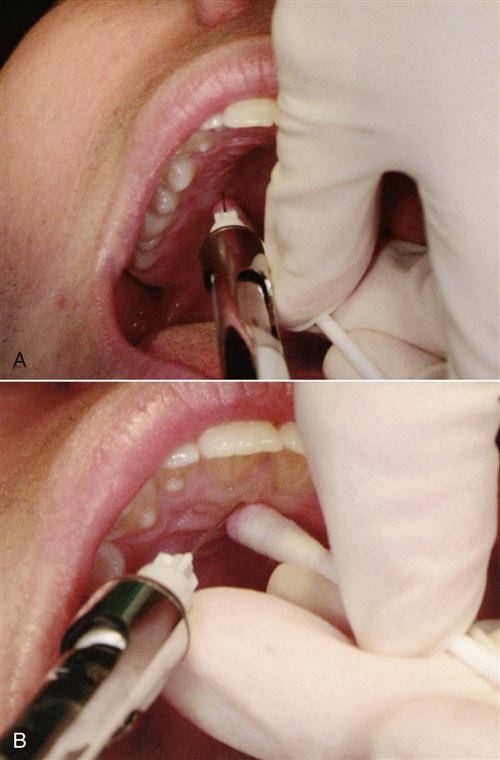
The location and the innervation of the tooth or teeth to be anesthetized will determine where topical anesthetic is placed and the type of injection to be given.
Maxillary Anesthesia
Local anesthesia injection techniques differ from mandibular approaches because of the porous nature of alveolar cancellous bone in the maxilla. This type of bone structure allows the anesthetic solution to diffuse through the bone and reach the apices of the teeth in a different manner.
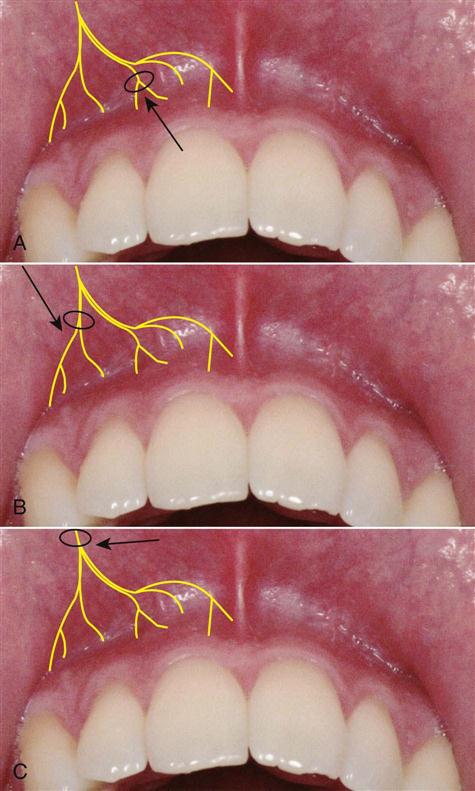
Three major types of local anesthetic injections may be given in the maxillary arch. Local infiltration is completed by injecting into a small, isolated area; field block refers to the injection of anesthetic near a larger terminal nerve branch. When two or three teeth are being restored, a field block is indicated. Nerve block occurs when local anesthetic is deposited close to a main nerve trunk. This type of injection is indicated for quadrant dentistry. Examples of these types of injections are the posterior superior alveolar, the inferior alveolar, and the nasopalatine nerves (Fig. 37-3).
Palatal Anesthesia
Local anesthesia in the palatal area may be necessary for procedures that involve the palatal soft tissues of the palate. Common palatal injections are the anterior (or greater) palatine nerve block, which provides anesthesia in the posterior portion of the hard palate, and the nasopalatine nerve block, which produces anesthesia in the anterior hard palate (Fig. 37-4).
For many patients, this procedure can be a very painful experience. It is best to advise patients that they may have some discomfort during the injection.
Mandibular Anesthesia
Because of the dense, compact nature of the mandibular bone, anesthetic solution does not diffuse easily through it. Therefore, block an/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses