Chapter 33 Anterior Single-Tooth Replacement: Surgical Considerations
Single-tooth replacement will most likely comprise a larger percentage of prosthetic dentistry in the future, compared with past generations. In 1960 the average American older than 55 years had just seven original teeth. Today, the baby boomers (those born between 1946 and 1964) can expect to have at least 24 teeth left when they reach 65 years of age.
ALTERNATE TREATMENT OPTIONS FOR ANTERIOR SINGLE-TOOTH REPLACEMENT
The alternatives to restore a single, maxillary anterior missing tooth include a traditional FPD; a cantilever FPD (for a missing lateral incisor); a removable partial denture (RPD); an acid-etched, resin-bonded prosthesis; or a single implant–supported restoration. These options were presented in Chapter 16. Maxillary single-tooth replacement is one of the most challenging restorations in dentistry. However, in light of all the advantages of single-implant longevity, bone maintenance, reduced abutment teeth complications, and increased survival of adjacent teeth, single-tooth implants have become the treatment of choice.
The single-tooth implant has the highest success rate compared with any other treatment option to replace missing teeth with an implant restoration (e.g., overdentures, short-span FPD, full-arch FPD, single-tooth implant).1–11 In 2005, Misch et al.7 reported on 276 anterior maxillary single implants used to restore missing teeth from agenesia. In 255 adolescent patients, the implants were monitored for a range of 2 to 16 years, with a 98.6% implant and crown survival rate. In the same year, Wennstrom et al.8 reported on a 5-year prospective study with 45 single-tooth implants, with a 97.7% implant survival rate with minimal bone loss. In 2006, Zarone et al.11 reported on lateral maxillary agenesis replacement with 34 implants, with a 97% survival rate at 39 months. A review of the literature by Goodacre et al.6 found single-tooth implant studies had the highest survival rate of any prosthesis type and averaged 97%.
More recently, a trend toward single-stage and immediate-extraction implants has emerged, appearing especially attractive in the maxillary anterior region, where preferably the soft tissue drape is present before the tooth extraction and patients are more anxious to get a fixed replacement. Kemppainen et al.,12 in a prospective study of 102 single-tooth implants in the anterior maxilla, reported a 99% success rate using one-stage and two-stage implants. Other studies have recommended one stage and immediate load with some success in specific situations.13–15
CHALLENGING ESTHETICS
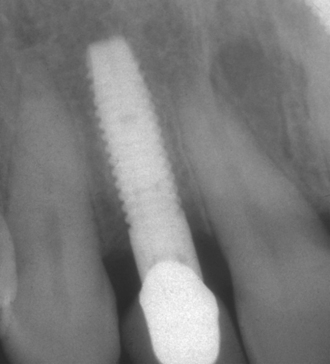
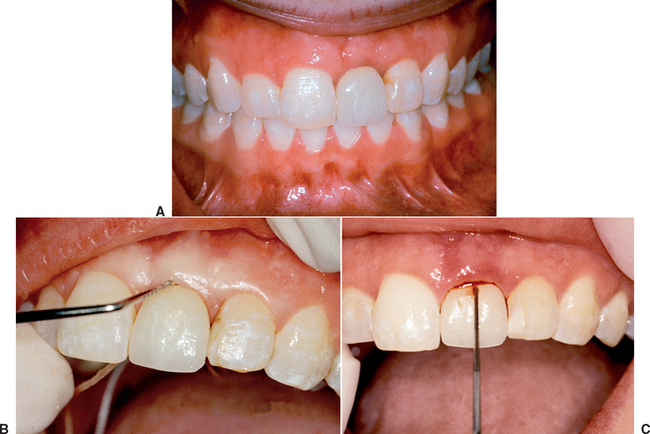
The esthetics of a maxillary anterior single crown on a natural tooth is often one of the most difficult challenges in restorative dentistry. It is even greater on an implant abutment (Figures 33-1 and 33-2). The implant is often 5 mm or less in diameter and round in cross section. A natural maxillary anterior crown cervix region is 4.5 to 7 mm in mesiodistal cross section and is never completely round. In fact, the natural central incisor and canine teeth are often larger in their faciopalatal dimension at the cement-enamel junction (CEJ) than in the mesiodistal dimension. Because the bone is lost first in the faciopalatal width, the greater width of implants in this dimension would require even greater augmentation than presently advocated. As a result, the cervical esthetics of a single-implant crown must accommodate a round-diameter implant and balance hygiene and esthetic parameters. Additional prosthetic steps and components with varied emergence profiles or customized tooth-colored abutments are often required to render the illusion of a crown on a natural abutment.
Bone Height
The position of the interproximal crest of bone is an important anatomical consideration, especially for the development of the interproximal soft tissue height.16,17 Becker et al.18 classified the range of interproximal bone height above the midfacial scallop from less than 2.1 mm (flat) to scalloped (2.8 mm) to pronounced scalloped (<4.1 mm). The flat anatomy should correspond to a square-shaped tooth, the scalloped to an ovoid-shaped tooth, and the pronounced scalloped to a triangular-shaped tooth (Figure 33-3). However, these relationships do not always exist. When a flat interdental-to-crest dimension is found on triangular teeth, the interproximal space will usually not be filled with soft tissue, because the dimension of the interproximal contact to the bone will be greater than 5 mm (Figure 33-4).21
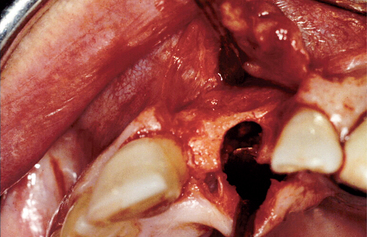
Often the osseous crest may be more apical than ideal, in both the implant site and the adjacent tooth roots. Under these conditions, ideal crown contour, soft tissue emergence, and interproximal tissue conditions are less likely (Figures 33-5 and 33-6). Bone and soft tissue changes after maxillary anterior tooth loss are rather rapid and of considerable consequence. As a result, many maxillary anterior edentulous sites require at least some bone and/or soft tissue modification before, in conjunction with, and/or at implant uncovery. Under perfect conditions, the implant body should not be inserted until the bone and soft tissue are within normal limits.

Figure 33-6 The lateral incisor implant crown from Figure 33-5. The interproximal distal papilla is acceptable as a result of the canine crestal bone level. The mesial papilla is depressed, and a “black hole” is evident. This is related to the crestal bone level on the central incisor. In addition, the triangular tooth form translates into a more incisal interproximal crown contact position, which further enhances the triangular defect. The distal bone loss on the central also increases the risk of root exposure (as shown).
Mesiodistal Space
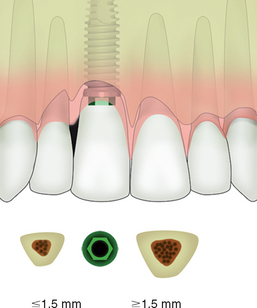
An adequate mesiodistal space is necessary for an esthetic outcome of an implant restoration and the interproximal soft tissue of the adjacent teeth. A traditional two-piece implant should be at least 1.5 mm from an adjacent tooth. When the implant is closer than this to an adjacent tooth, any bone loss related to the microgap, the biological width, and/or stress might cause the implant and adjacent tooth to lose bone. This may compromise interproximal esthetics and/or sulcular health of the implant and natural tooth19–21 (Figure 33-7).
One-piece dental implants may be fabricated in 2.5-to 3.0-mm22–24 diameters to accommodate a reduced mesiodistal dimension criterion. These implant designs do not have a microgap, and the vertical defect is narrower than most two-piece implant systems. As such, they may be placed as close as 1 mm from an adjacent tooth, and therefore can accommodate a 5-mm mesiodistal missing tooth space. However, because these implants have the abutment post attached to the implant body, they must be immediately restored the day of surgery. These implants are addressed in Chapter 35.
Faciopalatal Width
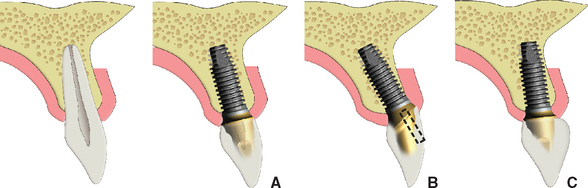
Most of the conditions that lead to single-tooth loss result in the loss of some or all of the facial bone in the region of the missing tooth. In addition, a 25% decrease in faciopalatal width occurs within the first year of tooth loss and rapidly evolves into a 30% to 40% decrease within 3 years. As a result, even an intact alveolus 6 to 8 mm wide is often inadequate in width after 1 year for a Division A root form implant in a central incisor position, and after 3 years it almost never presents adequate available bone for the proper-size implant. The bone width loss is primarily from the facial region, because the labial plate is very thin compared with the palatal plate, and facial undercuts are often found over the roots of the teeth (Figure 33-8). A bone graft is often necessary to restore the proper anatomy of the ridge and to avoid a compromised implant position more palatal and apical.
Implant Size
The first factor that influences the size of an implant is the mesiodistal dimension of the missing tooth. The average mesiodistal dimension of a central incisor is 8.6 mm for a man and 8.1 mm for a woman, a lateral incisor is 6.6 mm for a man and 6.1 mm for a woman, and a canine is 7.6 mm for a man and 7.2 mm for a woman. Obviously, the implant body should not be as wide as the natural tooth or clinical crown. Otherwise, the emergence contour and interdental papillae region cannot be properly established.
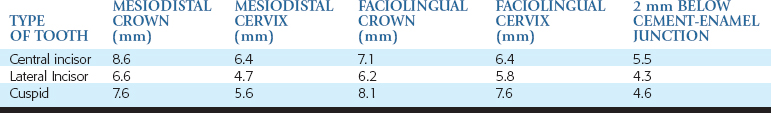
The mesiodistal dimensions of the maxillary central incisor at the cervix (preferably 1 mm below the free gingival margin) averages 6.4 mm, the lateral incisor dimension is 4.7 mm, and canine natural teeth at the cervix are 5.6 mm (Table 33-1).25,26 However, these dimensions are also too large for an implant.
The second factor that determines the mesiodistal implant diameter is the necessary distance from an adjacent tooth root.20 Initial vertical bone loss around an implant during the first year of loading is variable and ranges from 0.5 to more than 3.0 mm.
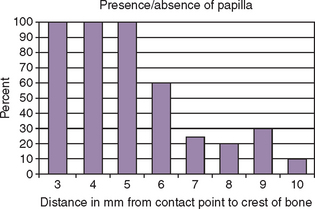
The height of the interseptal (interimplant) bone in part determines the incidence of presence or absence of the interdental papillae between the teeth.21 When the distance from the interseptal bone to interproximal contact is 5 mm or less, the papilla fills the space. When the distance is 6 mm, a partial absence of papilla is seen 45% of the time, and at 7 mm the risk of a compromise in the interproximal space is 75%. Therefore the intraseptal bone height is relative to the maintenance of the interdental papilla and should be preserved. As a consequence, the implant should be at least 1.5 mm from the adjacent teeth whenever possible, and the interseptal bone on the adjacent teeth should be within 5 mm of the desired interproximal crown contact position.
The next dimension that determines the width of an anterior implant is the faciopalatal dimension of bone. The width of bone should allow at least 1.5 mm on the facial aspect of the implant so that if a vertical defect forms around the crest module, then that defect would not become horizontal and change the cervical contour of the facial gingival. Because of its initial reduced volume, facial bone tends to be labile, and its resorption is responsible for most of the compromised long-term esthetic results in the anterior maxilla.27–29 The faciopalatal width dimension is not as critical on the palatal aspect of the implant, because it is dense cortical bone, more resistant to bone loss, and not within the esthetic zone. Facial bone grafting at the time of implant insertion is frequently needed, because the bone volume in width is often compromised (Figures 33-9 to 33-11).

Figure 33-9 An implant placed in the central incisor position, with less than 1.5 mm of bone on the facial.
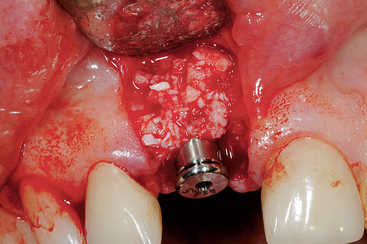
Figure 33-10 A layer of freeze-dried bone (MinerOss) is placed over the autograft on the facial bone over the implant.
The width of the implant should not only mimic the emergence of a natural tooth, but also help to preserve the bone and health of the adjacent teeth. The natural intraroot distance of the two central incisors distance is approximately 2 mm. However, the natural roots of the central to lateral and lateral to canine are usually less than 1.5 mm apart and often only 0.5 mm of space exists between them. As a consequence, the archetypal size of the single-tooth implant is usually smaller in diameter than the natural tooth root.
IMPLANT BODY POSITION
Mesiodistal Position
The maxillary anterior single-tooth implant should be located precisely in three planes. From a mesiodistal aspect, the implant most often is placed in the middle of the space, with equal amount of interproximal bone toward each adjacent tooth. On occasion, the central incisor implant is positioned slightly to the distal of the intratooth space (Figure 33-12). The incisive foramen is variable in size and position. When a central incisor implant is planned and the foramen between the existing central incisor root and implant site is larger than usual, the remaining bone may be inadequate. The foramen may also expand off to one side of the midline within the bony canal. When the central incisor implant is placed, the implant may encroach on the canal and result in a probing pocket depth of 10 mm or greater on the mesiopalatal surface of the implant. As a precaution, the surgeon should reflect the palatal tissue when placing a maxillary central incisor implant, probe the foramen, and if necessary, place the implant in a more distal position. This usually requires a smaller-diameter implant than usual to remain 1.5 mm or more from the lateral incisor. On occasion, the contents of the foramen must be removed and a bone graft inserted, to decrease the size of the incisive canal (Figure 33-13).
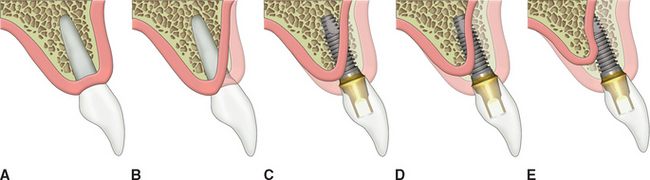
Implant Angulation
The implant center is positioned in the faciopalatal center of the edentulous ridge and the midmesiodistal position. The implant body angulation from this point is considered next. In the literature, three faciopalatal angulations of the implant body are suggested: (1) a facial angulation so that emergence of the final crown will be similar to adjacent teeth, (2) under the incisal edge of the final restoration, and (3) within the cingulum position of the implant crown (Figure 33-14).
Facial Implant Body Angulation
Researchers often theorize that a maxillary anterior implant body angulation be positioned at the facial emergence of the final crown. The facial implant position is predicated on the concept that the facial emergence of the implant crown at the cervical should be in the same position as a natural tooth. At first, this makes some sense. However, the crown of a natural tooth has two planes, and its incisal edge is palatal to the facial emergence of the natural tooth by 12 to 15 degrees (Figure 33-15). This is why anterior crown preparations are in two or three planes. The implant body is more palatal than a natural root, so 1.5 mm of bone exists facially. In addition, because the implant is narrower in diameter than the faciopalatal root dimension, when the implant body is oriented as a natural tooth and has a facial emergence, a straight abutment is not wide enough to permit the two or three plane reduction to bring the incisal edge of the preparation more palatal. As a result, the incisal edge of the preparation remains too facial. Therefore when the implant is angled to the facial emergence of a tooth, an angled abutment of 15 degrees must be used to bring the incisal edge more palatal.
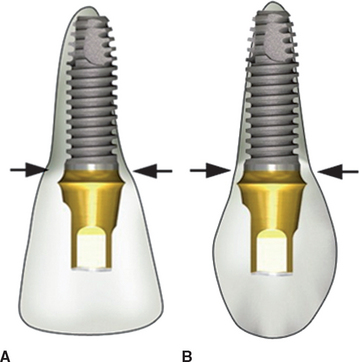
Most two-piece angled abutments have a design flaw that compromises facial cervical esthetics (Figure 33-16). The metal flange facial to the abutment screw is thinner than a straight abutment and may result in fracture (especially because angled loads are placed on the facial-positioned implant). The manufacturers thicken the profile of the abutment on the facial aspect to reduce the risk of fracture. However, this design flaw brings the cervical facial margin more facial and wider than the implant body, which is already as facial as the adjacent tooth. As a result, the implant crown margin is facially overcontoured. The restoring doctor then has to prepare the facial aspect of the abutment metal flange for esthetics, which weakens it and makes it prone to fracture. Because the doctor modified the abutment, the implant company is held harmless but, nonetheless, the patient and doctor are at risk.
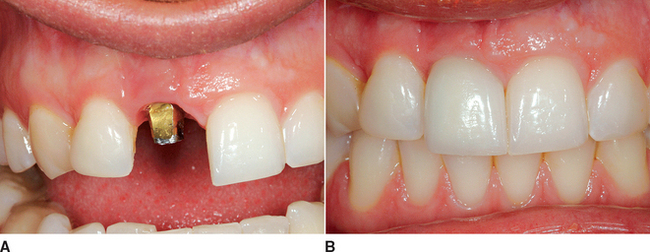
When the surgeon attempts to align the implant body with the facial aspect of adjacent teeth, the implant may inadvertently be inserted too facial. No single method exists to restore proper esthetics when the implant abutment is located above the free gingival margin of the adjacent teeth. At best, the final crown appears too long and too facial. Soft tissue grafts and/or bone augmentation do not improve the condition once the implant is already incorrectly inserted (Figure 33-17).
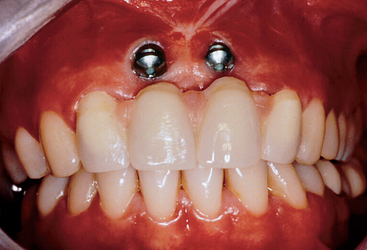
Figure 33-17 When implants are placed too facial, no prosthetic method is available to improve the poor esthetic condition.
The natural maxillary anterior teeth are loaded at a 12- to 15-degree angle, because of their natural angulation in comparison with the mandibular anterior teeth. This is one reason the maxillary anterior teeth are wider in diameter than mandibular anterior teeth (which are loaded in their long axis). The facial angulation of the implant body often corresponds to an implant body angulation, which leads to 15 degrees off axial loads and increases the force to the abutment screw-implant-bone complex by 25.9%, compared with a long axis load. These offset loads increase the risks of abutment screw loosening, crestal bone loss, and cervical soft tissue marginal shrinkage. As a result, implants angled too facially compromise the esthetics and increase the risk of complications (Figure 33-18).
Cingulum Implant Body Angulation
A second angulation suggested in the literature is more palatal, with an emergence under the cingulum of the crown. This may also be the result of an implant insertion in a width-deficient ridge (Division B), because the bone is lost primarily on the facial (see Figure 33-8, C). This position is often the goal when a screw-retained crown is used in restoration. The prosthesis fixation screw (to retain a maxillary anterior crown) cannot be located in the incisal or facial region of the crown for obvious reasons.
The cingulum implant position may cause a considerable health compromise. The implant body is round and usually 4.0 to 5.5 mm in diameter. The labial cervical contour of the implant crown must be similar to the adjacent teeth for the ultimate esthetic effect. Because the long axis of the implant for a screw-retained crown must emerge in the cingulum position, this most often requires a facial projection of the crown or “buccal correction” facing away from the implant body. The facial ridge lap must extend 2 to 4 mm and is often similar in contour to the modified ridge lap pontic of three-unit fixed prosthesis (Figure 33-19).
The modified ridge lap crown has become a common solution to correct the esthetics of the restoration when the implant is placed in narrow bone or follows a palatal angulation position.30,31 However, plaque control on the facial of the implant is almost impossible. Even if the toothbrush could reach the gingival sulcus, no hygiene device could be manipulated to a right angle to proceed into the facial gingival sulcus. As a result, although an acceptable esthetic restoration may be developed, especially with the additional cervical porcelain, the hygiene requirements and present implant dentistry standards render this approach unacceptable (Figure 33-20).
IDEAL IMPLANT ANGULATION
The third implant angulation in the literature describes the most desirable implant angulation. A straight line is determined by connecting two points. The clinician determines the line for the best angulation by the point of the incisal edge position of the implant crown and the midfaciopalatal position on the crest of the bone. The center of the implant is located directly under the incisal edge of the crown so that a straight abutment for cement retention emerges directly below the incisal edge (Figure 33-21). Because the crown profile is in two planes, with the incisal edge more palatal than the cervical portion, the incisal edge position is perfect for implant placement and also accommodates some of the facial bone loss that often occurs before implant placement. The facial emergence of the crown mimics the adjacent teeth, proceeding from the implant body under the tissue. The angle of force to the implant is also improved, which decreases the crestal stresses to the bone and abutment screws (Figure 33-22). When in doubt, the implant surgeon should err toward the palatal aspect of the incisal edge position, not to the facial aspect, because it is easier to correct a slight palatal position in the final crown contour compared with the implant body angled too facial.
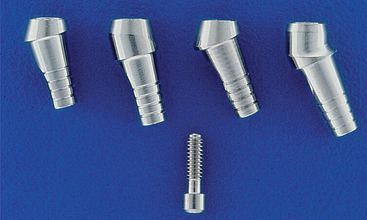
The implant abutment selected for a maxillary anterior single-tooth implant is almost always for a cemented restoration. Single anterior crowns do not require readily retrievable restorations. In addition, a greater range of corrective options exists with a cement-retained crown for implants not well placed. The location of the cervical margin of a cemented crown can be anywhere on the abutment post or even on the b/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses