Chapter 32
Diagnosis and Non-surgical Management of Orofacial Pain
There are multiple causes of orofacial pain separate from temporomandibular disorders, including a number of medical and dental conditions.
Medical Conditions which can Mimic Orofacial Pain
Intracranial Disorders
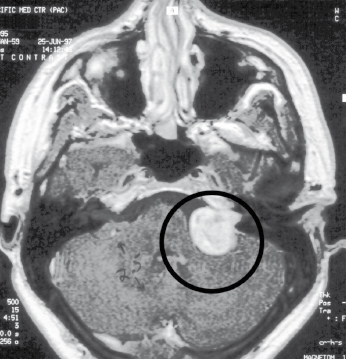
Disorders of the intracranial structures, such as neoplasia, aneurysm, abscess, hemorrhage or hematoma, and edema can usually be easily differentiated from orofacial pain (Fig. 32.1). They should be considered first in the diagnostic process, because they can be life-threatening and require immediate attention. The characteristics of serious intracranial disorders include new or abrupt onset of pain, pain that increases in severity, interruption of sleep by pain, pain precipitated by exertion or positional change, and neurologic deficits. One vascular pain disorder, temporal arteritis – a giant cell arteritis – may be misdiagnosed as myofascial pain involving the temporalis muscle. If treatment is delayed, temporal arteritis can lead to a sudden loss of vision.
Neurovascular Headache Disorders
Headache is a common complaint reported by patients suffering from musculoskeletal jaw disorders.
Primary Headache
Primary headache disorders associated with orofacial pain include migraine headaches, migraine-variant headaches, cluster headaches, chronic paroxysmal hemicrania, and tension-type headaches.
Secondary Headache
Secondary headache disorders are defined as headaches that develop secondary to another condition or mechanism. These could include physical exertion, cold stimuli, trauma, infection, metabolic disorders, or substance withdrawal.
Neuropathic Pain Disorders
Neuropathic pain is a disorder resulting from injury, peripheral and/or central, in the pain transmission system and is usually present in the absence of an ongoing primary source for the pain. Neuropathic pain disorders are divided into either paroxysmal (episodic) or continuous painful conditions.
Paroxysmal Disorders
The paroxysmal conditions associated with orofacial pain include: trigeminal neuralgia, glossopharyngeal neuralgia, and the more rare conditions of nervous intermedius neuralgia and superior laryngeal neuralgia.
Continuous Disorders
The continuous neuropathic pain disorders associated with orofacial pain are primarily deafferentation pain syndromes related to compression or distortion, demyelination, infarction, or inflammation of the cranial nerves. Acute herpes zoster, chronic postherpetic neuralgia, diabetic neuropathy, and neuromas are examples of continuous neuropathic pain syndromes.
Headache Attributed to Associated Extracranial Pain Disorders
Extracranial pain disorders associated with orofacial pain include pain related to the eyes, ears, nose, sinuses, throat, intraoral structures, neck, jaw, and cranial bones.
Intraoral Pain Disorders
Intraoral pain disorders include odontogenic pain, and pain conditions associated with mucogingival tissues, tongue, and salivary glands.
Musculoskeletal, Cervical and Temporomandibular Disorders
Musculoskeletal conditions affecting the jaw (TMD) and neck are the major cause of non-odontogenic pain in the orofacial region. They include cervical spine and temporomandibular joint (articular) disorders; and cervical and masticatory muscle (non-articular) disorders.
Temporomandibular Disorders
Temporomandibular disorders (TMD) were referred to as a syndrome in the past. Common terms were “TMJ”, “TMJ syndrome”, or “TMJ pain–dysfunction syndrome”. Presently they are considered to be a collection of various distinct articular or muscular conditions affecting the jaw, often with similar signs and symptoms, but different underlying mechanisms. The common clinical presentation is any combination of jaw, face, head, or ear pain, TMJ noises such as clicking, popping or crepitus, or grating, and/or limited jaw opening, jaw catching, and locking. Related symptoms, without proven cause and effect, include global headaches, neck pain, tinnitus, ear fullness or perceived hearing loss, and dizziness. Pain in the TMJ region is reported in approximately 10% of the population over 18 years of age (8–15% for women and 3–10% for men). The gender ratio varies between cross-sectional studies from anywhere from 4 : 1 to 2 : 1 female to male. The peak age is approximately 35–45 years (the child-bearing years of females).
Although the etiology of the various subsets of TMD was in the past thought to directly relate to occlusal discrepancies and improper jaw relationships, presently the number of related contributing factors for each specific diagnosis is uncertain and many times unknown. It is now generally felt that malocclusion is not directly correlated to the various subsets of TMD. Contributing etiologic factors include trauma, possibly parafunction, gender and hormonal factors, systemic factors, overuse of the masticatory system, and psychosocial and behavioral factors. Recent evidence suggests a specific gene expression, primarily in females, implicated as a risk factor for persistent orofacial pain.
Classification of Articular Disorders
TMJ disorders include congenital, developmental, or acquired disorders, disc derangement disorders, condylar dislocation, inflammatory disorders, non-inflammatory disorders, ankylosis, and fracture of the condylar process.
Disc Derangements
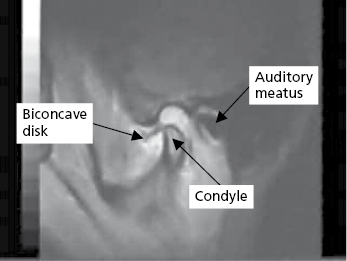
Disc derangement disorders represent an abnormal anatomical relationship or misalignment of the articular disc and condyle. Recent studies are revealing, however, that there is a great deal of variation in the disc position even in individuals without joint pain, joint noise, or jaw dysfunction. Stretched or torn collateral discal ligaments are thought to be the reason why discs become displaced, although there is still uncertainty regarding the natural history of these derangement conditions. Articular discs are typically displaced anteriorly and medially (Fig. 32.2), but can also be positioned laterally, or even posteriorly.
Condylar Dislocation
Condylar dislocation or open lock is a hypermobility condition of the jaw. It occurs when the condyle inadvertently becomes positioned anterior and superior to the articular eminence, during jaw opening or protrusion, and is unable to return to a closed position. It can be caused by trauma, extended periods of mouth opening such as a long dental appointment, or can b/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


