Chapter 31
Mandibular Reconstruction
Whenever a portion of the mandible is resected, consideration must be given to subsequent reconstruction. Although most patients do receive mandibular reconstruction following resection, there is still a minority for whom no reconstruction may be the most practical alternative. These cases particularly include shorter lateral defects, not involving the symphysis and parasymphysis areas, in elderly or medically compromised patients. The subsequent deformity in the absence of reconstruction is often acceptable under these circumstances. However, at present, the “gold standard” for reconstruction is autogenous bone.
Marginal Resection
Marginal resection of the mandible may be indicated for the excision of a benign tumor, a superficial malignant tumor involving periosteum only, or for infection. In this case mandibular continuity is not disrupted. However, the mandible is at risk for subsequent fracture, particularly if radiation therapy has to be given. For this reason, reconstruction is often performed. Bony reconstruction will also enable subsequent insertion of osseointegrated implants, if indicated, to complete prosthodontic reconstruction. In a young patient reconstruction may not be necessary since some spontaneous regeneration of bone may occur, particularly if the periosteum is retained. However, the mandible may need to be reinforced with a reconstruction plate (usually around 2.4 mm in thickness with appropriate screws) to minimize the risk of fracture. Following marginal resection, reconstruction can be with corticocancellous blocks from the iliac crest (full thickness or partial thickness), which can be contoured so that they will mortice into place with minimal or no fixation (Fig. 31.1). For a lesion less than about 3 cm in size this can be carried out immediately from an intraoral approach; for defects greater than this, consideration should be given to carrying this out secondarily and possibly from an extraoral approach, to avoid the risk of graft failure due to infection secondary to salivary contamination. Subsequent soft tissue grafting is often necessary to supply attached mucosa for denture or implant insertion. This is often carried out by means of a split-thickness skin graft, and normally done as a secondary procedure following incorporation of the bone graft.
Segmental Resection
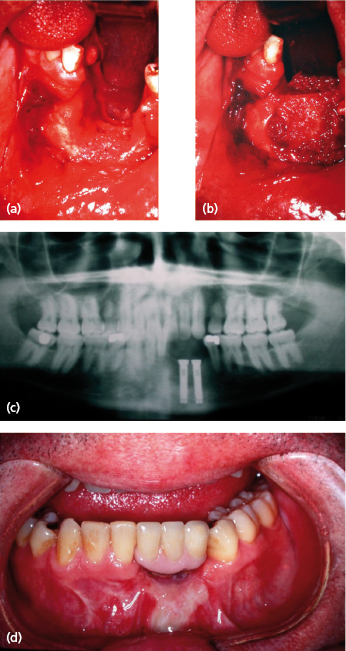
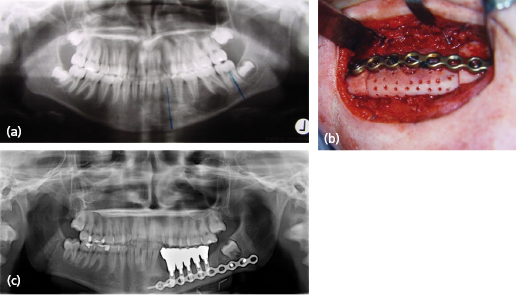
Segmental resection of the mandible with loss of mandibular continuity may be necessary for benign or malignant lesions, as well as for chronic infection. Temporary immediate reconstruction is often carried out by means of a reconstruction plate, but these are rarely satisfactory for long-term use. The usual history is for the plate to either exteriorize itself and become secondarily infected, or for screw loosening and mobility to occur. Depending on the forces placed on it, these problems will normally occur after some 18 months or 2 years. Plate fracture has also been reported (Fig. 31.2). In particular, reconstruction plates fail most frequently in the anterior mandible, but can survive in the long-term in the body and posterior parts of the mandible, particularly if these have adequate soft tissue coverage, which may have to be in the form of a soft tissue flap, such as a pectoralis major flap.

Nevertheless, it is generally more appropriate to reconstruct the mandible with non-vascularized autogenous bone. Non-vascularized autogenous bone is normally used as a secondary procedure. Immediate segmental reconstruction with non-vascularized autogenous bone from an intraoral approach has been associated with a high failure rate, although it was recommended by Obwegeser amongst others. The reasons for failure are generally wound breakdown intraorally and contamination of the wound with saliva, or primary infection due to oral contamination. Reconstruction is therefore more normally carried out secondarily. The most appropriate time to carry this out would appear to be some 6–8 weeks following primary resection for the following reasons:
- this gives the intraoral wound time to heal and gain some tensile strength;
- the wound bed has time to self-decontaminate;
- scarring and fibrosis have not had an opportunity to develop.
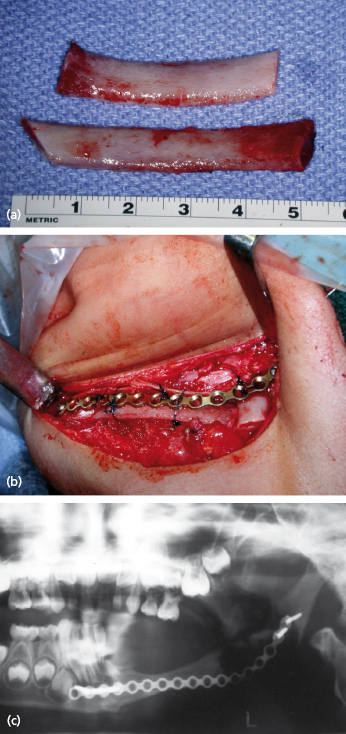
Resection is often carried out from a combined intraoral and extraoral approach, and temporary reconstruction is carried out with a titanium reconstruction plate (usually a 2.4 mm plate is adequate). Some 6–8 weeks later, definitive reconstruction is carried out from an extraoral approach using autogenous bone. Depending on the circumstances, this can be by the use of autogenous ribs (usually in a younger patient) (Fig. 31.3), corticocancellous blocks from the iliac crest (full thickness or partial thickness) (Fig. 31.4), or cancellous bone marrow in a carrier tray. The tray can be of titanium mesh or an allogenic bone tray (Fig. 31.5), or in exceptional circumstances, it may be an autogenous bone tray, since it may be possible to carry out a segmental resection of the mandible for a benign lesion, excise the lesion from the mandible, and reinsert it as its own carrier tray.
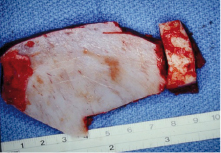
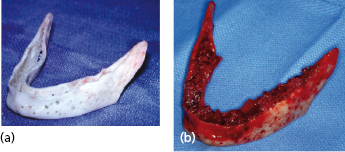
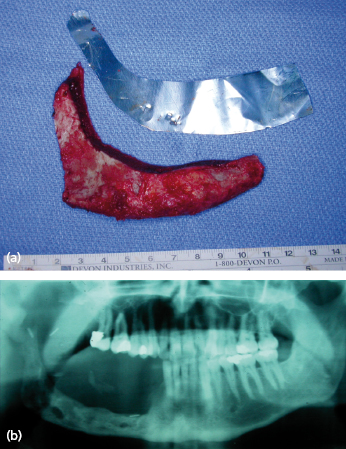
Over the years, many attempts have been made to reconstruct the mandible using the actual autogenous mandible that was previously resected. In the case of a benign lesion, it may be possible to resect the mandible, remove the lesion, and reinsert the mandible. In most cases this does mean hollowing the mandible out to resemble a tray, perforating the tray, and securing it with a reconstruction plate, and then completing the reconstruction with autogenous marrow within the tray. This gives the most esthetic reconstruction, since it is the patient’s own mandible and therefore the contour is the most acceptable. Figure 31.6 shows this technique used for a high-flow vascular malformation of the mandible. When this treatment is contemplated for aggressive lesions, or even malignant lesions, the resected mandible must be “sterilized” in some way to kill unwanted cells. In most cases the technique is just as described, in removing the lesion from the resected mandible, reducing the mandible to an autogenous tray and perforating it. Three different methods of sterilizing the mandible have been described. The first involves autoclaving the mandible; this will render the mandible non-vital, but most studies have shown that even with autogenous marrow grafting, excessive resorption normally occurs, and this technique is not widely practiced today. An alternative technique is to devitalize the mandible by means of cryotherapy, and for this the mandibular tray is immersed in liquid nitrogen at −196°C for 10 minutes. The mandible is then allowed to thaw and is refrozen. Studies have shown that liquid nitrogen predictably causes cell death below −20°C and that the most satisfactory results are achieved with a rapid freeze and a slow thawing process. Although described in the literature, the technique does not appear to be widely practiced today. The third technique involves gamma irradiation of the mandible which will successfully devitalize the mandible, and does not appear to result in excessive resorption when it is reinserted and rigidly fixed and grafted. If a source of radiation is locally available, this technique can be carried out in one session while the patient is asleep and at the same time as the initial resection. The mandible can be cleaned, placed in a sterile autoclave bag and receive around 50 Gy of radiation in less than 1 hour, in time for reinsertion into the patient. Otherwise, the procedure must be staged. Any of these techniques may result in a more acceptable contour than using an autogenous graft from another part of the body.
Studies have shown that segmental resections of up to 6 cm are associated with a high success rate when reconstructed by any of these techniques. Above 6 cm the failure rate starts to increase and when the resected area exceeds 9 cm the failure rate from a non-vascularized graft may be as high as 75%. Figure 31.7 shows a successful 10 cm non-vascularized graft even though it has undergone considerable resorption. Failure usually occurs because of failure of the bone graft to become vascularized and reincorporate, with subsequent infection and wound breakdown.
A number of factors have been identified which may improve or compromise bone healing and the incorporation of bone grafts on reconstruction. Platelet rich plasma (PRP), and possibly other platelet-derived and other growth factors, may enhance incorporation of bone grafts and also may enhance soft tissue healing. Early initial results were very promising, but some subsequent papers have cast doubts on the long-term success of these factors, which have decreased their popularity.
Bone morphogenic proteins (BMPs) have been identified but have only recently become commercially available. They have the ability to induce bone formation by recruiting osteoblastic stem cells to produce bone, thus possibly avoiding a bone graft. In the USA only BMP-2 is currently available, although in Europe BMP-7 (also known as osteoprotein or OP1) is also available. Although these show promise, it is not known which of these factors is going to prove the most effective, and whether more than one factor is necessary to get the maximum enhancement of bone incorporation, and even whether there is a cascade process involved. At the current time, BMP-2 can only be utilized on an acellular bovine collagen sponge which is compressible and limits its usefulness to procedures such as sinus grafting for implants.
When the bone graft has taken successfully, subsequent staged procedures include removal of the bone plate. This may be necessary to allow subsequent vestibuloplasty and implant insertion. It may be necessary if the patient can feel the plate or screws beneath the tissue, if the plate appears to be in danger of exteriorizing itself, or if subsequent resorption of the bone graft is anticipated due to the effects of stress shielding. Stress shielding remains controversial in the maxillofacial regions. In the long bones, particularly the humerus, this has been shown to be a real issue, in that when a rigid bone plate is removed after healing of a fracture of the humerus, it is not uncommon for refracture to occur since the bone plate has shielded the humerus from excessive forces, and therefore it has never fully remodeled and gained its premorbid strength. Although some studies have shown that stress shielding may be a factor in the healing of mandibular fractures, other studies have shown that it does not appear to be an issue. Nevertheless, there are some patients who do seem to show excessive resorption following bone grafting, and it is felt that the presence of a rigid reconstruction plate may mean that the bone graft is not subjected to physiological forces, and therefore resorbs at an excessive rate. In these cases, removal of the bone plate may be advisable before the resorptive process becomes too pronounced. Timing of the removal of the plate is often critical, since one cannot remove it prior to the bone graft incorporating, but one wishes to remove it before excessive resorption has occurred. A time of between 4 and 9 months is normally quoted following the grafting procedure before removal of the bone plate. Occasionally bone plates also have to be removed for other reasons, including infection, screw loosening, plate fracture, and exteriorization of the plate or the patient being able to feel the plate through the soft tissues. Occasionally plates also cause discomfort with extremes of temperature. Following removal of the bone plate, it would be possible to carry out vestibuloplasty if necessary and to allow for subsequent osseointegrated implant insertion.
Non-Vascularized Bone Grafting for Mandibular Reconstruction
Multiple sites have been advocated for obtaining bone that might be used for maxillofacial reconstruction. Some sites, such as the radius and ulna, are rarely used today. Cranial bone is used for post-traumatic reconstruction of the mid and upper face, but quantities are generally insufficient for mandibular reconstruction. The main sites used for non-vascularized mandibular reconstruction are ribs, the iliac bone, and the proximal tibia.
Ribs
Ribs can be used with a cartilage cap from the costochondral junction if they are required for temporomandibular joint (TMJ) reconstruction, or without cartilage for mandibular reconstruction, particularly in children. In an adult, a considerable length of rib can be obtained (often up to 15 cm) accepting the curvature of the rib. Ribs are normally taken between the fifth and eighth ribs (avoiding the ribs with considerable attachment of the pectoralis major muscle and also avoiding the free floating ribs). Ribs can be taken from either side with equal ease.
This procedure is normally only carried out under intubated general anesthesia with the ability to administer positive pressure ventilation in the event of a pneumothorax. The surgical procedure involves identifying the rib or ribs to be taken and an incision is made directly over the rib. In females, the incision is normally placed beneath the breast or developing breast so that it will be hidden beneath the breast in the erect position. The incision is taken thro/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


