Chapter 3
Local Anesthesia
Mode of Action of Local Anesthetics
Local anesthetic drugs achieve their action at the voltage-gated sodium channel. In simple terms they inhibit sodium entry into nerve cells. As the entry of sodium into the nerve cell during the firing cycle is the chief driver producing depolarization, blockade of sodium transfer causes inhibition of neural activity.
It should be pointed out that the sodium channel is not a singular structure and that at least nine different variations have been identified. In theory this means that very selective local anesthetics could be developed. At present the local anesthetics used clinically are not specific for peripheral sensory nerves and can affect transmission in any excitable tissue such as motor nerves, central nervous system, and cardiovascular tissue.
Techniques of Local Anesthesia for Oral and Maxillofacial Surgery
There are a number of different techniques that can provide local anesthesia in and around the mouth and jaws. These include methods that are used elsewhere in the body such as topical anesthesia, infiltration, and regional block techniques; however, there are methods that are unique to the mouth and jaws, such as intraosseous, intraligamentary, and intrapulpal injections.
Topical Anesthesia
Topical anesthesia can be useful when applied to the oral mucosa. It may be employed prior to local anesthetic injections in the mouth to lessen the discomfort of needle penetration.
Topical anesthetics for intraoral use are available in a number of formulations including creams, ointments and sprays. The local anesthetic agents most commonly used as topical anesthetics in the mouth are lidocaine and benzocaine. Oraqix® is a combination of lidocaine and prilocaine specifically designed for intraoral topical anesthesia.
Advances in topical anesthesia (for example the development of Oraqix® and incorporation of drugs into liposomes) have meant that some intraoral soft tissue procedures can be performed using topical anesthesia as the sole agent; however, anesthesia of the teeth and jaws is not at present possible by this method.
Infiltration Anesthesia
Infiltration anesthesia is useful in providing localized skin and mucosal anesthesia and can also be used to provide anesthesia for some teeth and part of the jaws. It is the technique of choice in the maxilla for dental pulpal anesthesia and can also be used for this purpose in the mandible of children for anesthesia of the deciduous dentition. It can be successful in the incisor teeth in the adult mandible and there is increasing evidence that some formulations (as described in the following paragraphcan be effective when infiltrated in the molar region of the mandible.
When used intraorally, access to the point of needle penetration is easiest when the patient has the mouth only partly open. The technique is performed by inserting the needle through reflected mucosa at the depth of the buccal sulcus; if bone is contacted the needle should be withdrawn slightly so that it is supraperiosteal. A supraperiosteal location is recommended as injection below the periosteum is painful at the time of injection and may cause postinjection discomfort. Following aspiration 1.0–2.0 mL of solution is deposited at a rate of 30 s/mL. This rate is slower than many practitioners use. Slow injection has a number of advantages. It reduces discomfort and increases success. In addition, a slow rate of injection may lessen the effects of systemic problems.
This method allows about 45 minutes of anesthesia of the dental pulps when a solution containing a vasoconstrictor (such as lidocaine with epinephrine) is used; soft tissue anesthesia is longer and the patient may have subjective anesthesia of the soft tissues for 1.5–2 hours.
Regional Block Anesthesia
Several regional block techniques are described to anesthetize structures in the jaws.
Mandibular Anesthesia
There are a number of methods used to anesthetize the lower jaw, teeth and associated structures (for example, articaine 4% with 1 in 100 000 adrenaline). It should be remembered that midline structures (such as lower central incisor teeth) often receive bilateral supply; therefore, these may not be satisfactorily anesthetized by a single regional nerve block.
Inferior Alveolar Nerve block (Halstead Technique)
This method anesthetizes the teeth and bone on one side of the mandible along with the soft tissues on the buccal aspect anterior to the mental foramen. The Halstead method achieves its effect by deposition of the solution in the pterygotemporal space on the medial aspect of the mandibular ramus, specifically in the region of the mandibular foramen. When successful this technique anesthetizes the inferior alveolar nerve, which supplies the teeth on the same side of the mandible, the bone of the mandible to the midline and the soft tissues of the lower lip to the midline as well as the reflected and attached gingivae from the premolar teeth to the midline. In addition, this injection usually anesthetizes the lingual nerve that supplies the anterior two-thirds of the tongue on one side.
The technique is illustrated in Figure 3.1. The patient has the mouth open wide and the operator places the thumb of the non-syringe hand in the mouth on the coronoid notch of the mandible; the index finger is extraoral at the same height on the posterior border of the ramus. The syringe is advanced to the point of needle penetration across the lower premolar teeth of the opposite side. The point of penetration of the needle is between the internal oblique ridge of the mandible (which was palpated by the operator’s thumb before resting on the coronoid notch) and the pterygomandibular raphe (which is visible). The height of needle penetration is halfway up the operator’s thumb nail. A long 35 mm needle no narrower than 27 gauge is used and advanced until bone is contacted; this is usually around 25 mm of needle insertion. After contacting bone the needle is withdrawn slightly, aspiration performed and 1.5–2.0 mL of solution deposited slowly.
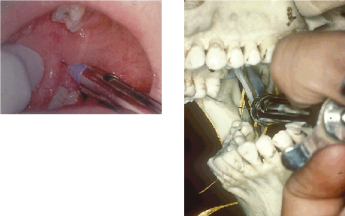
Two common problems with this method are either contacting bone too soon (after 5–10 mm of insertion) or failure to touch bone. The former (actually due to striking the internal oblique ridge of the mandible) is corrected by withdrawing the needle away from the bone, but not completely out of mucosa, and swinging the barrel of the syringe over the mandibular teeth of the side being anesthetized. The needle is then advanced about 25 mm and swung back again over the opposite premolar teeth; the rest of the injection is completed as described in the preceding paragraph. This is a modification of the indirect method of performing an inferior alveolar nerve block. If bone is not contacted after about 30 mm of insertion, the needle should be withdrawn until approximately 15 mm is still in tissue and the syringe swung over the molar teeth of the side not being injected, and then advanced until bone is contacted. Failure to contact bone may lead to injection into the parotid gland, affecting the intraparotid portion of the facial nerve, leading to hemifacial paresis.
When a vasoconstrictor solution, such as lidocaine with epinephrine, is used this technique will anesthetize the hard tissues including the teeth for around 45 minutes; however, subjective soft tissue numbness may be apparent for up to 3 hours. When the so-called long-acting solutions are employed anesthesia of the teeth can last for 6–8 hours.
Gow-Gates Technique
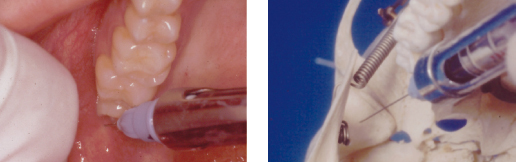
In addition to the anesthesia of the inferior alveolar nerve this method may anesthetize the lingual, long buccal, mylohyoid and auriculotemporal nerves. This may be of value in countering accessory nerve supply to the teeth and jaw. This approach deposits solution more superiorly than the Halstead technique and that is the reason why more branches of the mandibular nerve are affected by this injection. The target is the mandibular condyle (Fig. 3.2). As with the Halstead approach the patient has the mouth open wide. The syringe is advanced in a plane parallel to a line visualized between the corner of the mouth and the intertragal notch. The syringe, fitted with a long needle, is introduced into the mouth across the maxillary canine tooth of the opposite side to that being injected and advanced across the palatal cusps of the maxillary second molar on the side to be injected. This technique is often more successful in anesthetizing teeth than the Halstead approach. This may be the result of affecting nerves other than the inferior alveolar nerve that might supply the teeth.
Akinosi–Vazirani Technique
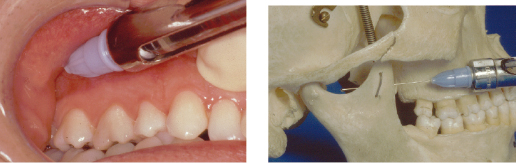
This technique (Fig. 3.3) differs from the methods described earlier in two respects. Firstly, it is administered with the patient’s mouth closed and so is useful in individuals who cannot fully open their mouth and is helpful in individuals with large or uncontrollable tongues when it is difficult to get access to the insertion point of a Halstead block. Secondly, there is no bony end-point for needle insertion. As is normal for all of the methods used to anesthetize the mandibular nerve, a long needle no narrower than 27 gauge is required. The syringe is introduced intraorally in the buccal sulcus along a plane level with the mucogingival junction of the maxillary mucosa. It is advanced at this level towards the posterior aspect of the maxilla until the hub of the needle is adjacent to the distal surface of the maxillary second molar. At this point the needle will have entered the mucosa and reached the correct depth of insertion. Aspiration is performed and 2.0 mL of solution injected slowly. If the anterior aspect of the mandibular ramus is contacted the barrel of the syringe can be swung more laterally or the patient instructed to move their lower jaw over to the side being injected. This method anesthetizes the inferior alveolar nerve, lingual nerve, nerve to mylohyoid, and occasionally the long buccal nerve.
Mental and Incisive Nerve Block
This injection anesthetizes the teeth and jaw from the premolars anteriorly as well as the soft tissues of the lower lip and chin to the midline on one side. Anesthesia of the first molar tooth is achieved in some cases. It relies on the deposition of solution around the mental nerve as it exits the mental foramen and the entry of solution into the foramen to block the incisive branch that supplies the lower anterior teeth on the same side. The usual method is intraoral although an extraoral approach may also be used. The needle is inserted at the depth of the buccal sulcus between the premolar teeth and advanced to a zone below the premolar apices. Around 1.5 mL of solution should be deposited and after injection the tissues should be massaged to encourage entry of solution into the mental foramen.
Long Buccal Nerve Block
If the long buccal nerve has not been anesthetized by the methods which are described under the heading Regional block anesthesia (for example, if the Halstead technique was used) then this nerve must be anesthetized separately if required. The area supplied is the buccal gingivae and mucosa and part of the cheek in the mandibular molar region. The nerve can be anesthetized by either buccal infiltration in the zone of interest or by a regional block. The regional block is achieved by depositing 0.5 mL of solution in the region of the coronoid notch of the mandible (the point at which the thumb rests during the Halstead technique).
Maxillary Anesthesia
Several regional block techniques are used in the maxilla. These are described as follows.
Maxillary Nerve Block
There are intraoral and extraoral approaches to the maxillary nerve block. The intraoral methods are the tuberosity approach and the greater palatine foramen approach. The maxillary nerve block anesthetizes the teeth and bone of the maxilla on one side together with the buccal and palatal mucosa, the skin and mucosa of the upper lip, the lower eyelid, and the lateral aspect of the nose.
Tuberosity Approach
This is administered by depositing solution high in the buccal sulcus in the plane of the distal surface of the maxillary second molar tooth. The needle is advanced at an angle of 45° superiorly, posteriorly and medially to a depth of 30 mm, at which point 2.0 mL of/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


