Chapter 3
Articulatory System Examination

Examination of the articulatory system should be a routine that you perform for all new patients and at regular intervals for existing patients, even those whom you know well. Symptoms of a temporomandibular disorder can come and go, and the patient may present complaining of the recent onset of a symptom such as a click which, by chance, was not present at the time of your previous examination. The three components to examine are the temporomandibular joints, the mandibular muscles and the occlusion.
Examination of the Temporomandibular Joints
Range of Movement 
Examination of the range of movement involves examining the interincisal opening, both pain-free and maximum (Figure 3.1) and lateral excursions of the mandible.
Figure 3.1 Measurement of incisal opening.
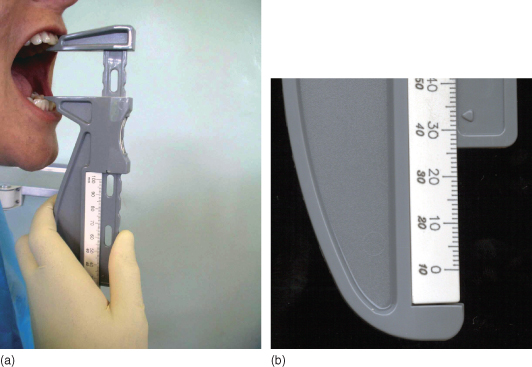
The lower limit of normal range of incisal opening is regarded as being approximately 35 mm for female patients and 42 mm for male patients. The opening is usually measured from incisal tip to incisal tip. It does not matter whether or not the overbite is included in your measurement regimen as long as you are always consistent in either including the overbite or excluding it so that your measurements are comparable and reproducible.
The range of lateral mandibular excursions (lower limit 8 mm on either side) should be measured from upper incisal midline to lower midline, with the patient moving the mandible first to one side then to the other (Figure 3.2).
Figure 3.2 Measurement of lateral jaw movement.
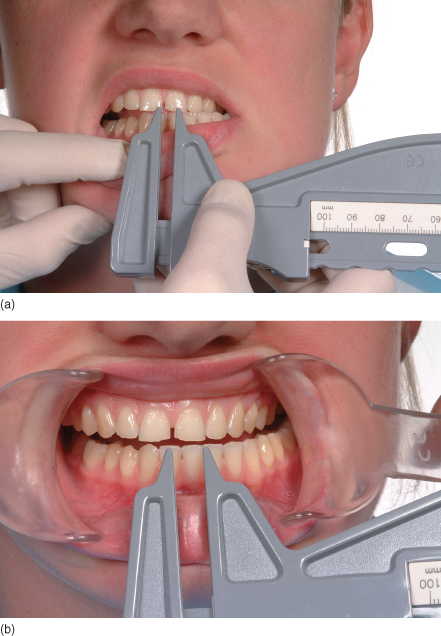
Any starting discrepancy in the incisal midlines when the patient is in centric occlusion should be taken into account.
Pathway of Jaw Opening 
Stand in front of your patient and ask him or her to repeatedly open and close the mouth as far as comfortably possible. Carefully watch the pathway and range of jaw movement. You can learn a lot from looking!
The mandible can open in a straight pathway or with a transient or lasting deviation. The mandibular pathway can be observed by standing in front of the patient and asking the patient to repeatedly open and close the mouth. Limitation or deviation of mandibular movement can be caused by two principal factors: either pain in the mandibular muscles or temporomandibular joint (TMJ), or a physical obstruction to movement. Much can be gained from examining the patient slowly opening and closing the mouth (Figure 3.3).
Figure 3.3 Diagrammatic representation of mandibular movements.
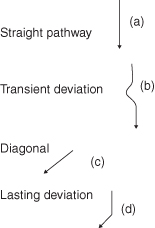
If the pathway is straight throughout the whole range of mandibular movement, this indicates that both joints are acting synchronously (Figure 3.3a).
If there is a deviation to one side and then back to the midline, or alternatively first to one side then across to the other and back to the midline, with the mandibular incisal midline coinciding with the maxillary incisal midline at maximum opening, this would imply that there has been a temporary obstruction to smooth mandibular movement, possibly due to disc displacement with reduction (Figure 3.3b).
If the mandible moves obliquely from the start of the opening cycle to the end of the opening cycle, this may imply that there are adhesions within the joint, with one condyle moving less well than the other throughout the range of movement (Figure 3.3c).
If the mandible moves vertically during the first phase of movement and then has an abrupt lateral deviation, this could imply that there is disc displacement without reduction. In this instance the mouth opens normally until the head of the condyle on the affected side encounters the disc in the unexpected and displaced position. Further translation of the condyle is prevented, thereby resulting in marked lateral deviation (Figure 3.3d).
Let us now consider the features of lateral movements. If there is disc displacement without reduction on one side and not the other, let us assume that this is the right side; the patient will be able to move the mandible to the right very much more freely than to the left because, on right lateral excursion, the right condyle pivots in the fossa and lateral jaw movement is attainable. If, however, as is usually the case, the intra-articular disc is displaced anteromedially, lateral movements of the mandible to the left side will be reduced because the condylar movement will be blocked by the disc, thereby severely limiting mandibular excursion in this direction.
Maxillary and Mandibular Midlines 
If a patient has a straight pathway or transient mandibular deviation during opening, then at maximum opening the upper and lower midlines will coincide. In the case of a patient with disc displacement without reduction, the maxillary and mandibular incisal midlines will remain coincident until the point at which the head of the condyle encounters the displaced disc and a lateral shift will then occur. There will then be an obvious discrepancy between the upper and lower centre lines at maximum opening (Figure 3.4).
Figure 3.4 Lasting deviation to the left. (a) mouth closed; centre lines coincident. (b) mouth open; mandibular deviation to the left.
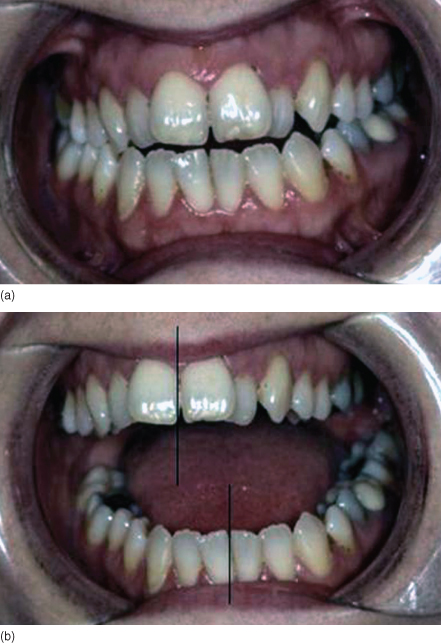
When there are adhesions in the joint, either between the disc and fossa or the disc and the head of the condyle then from the start of opening the maxillary and mandibular incisal centrelines will not coincide.
TMJ Tenderness 
TMJ tenderness can be elicited by different examination techniques: lateral palpation in the immediate preauricular area, intra-auricular palpation via the external auditory meatus or manipulation of the mandible to a retruded position.
Lateral Palpation
The lateral aspect of the joint is palpated by pressing gently over the immediate preauricular area, both at rest and during motion (Figure 3.5).
Figure 3.5 Lateral palpation of the temporomandibular joint.
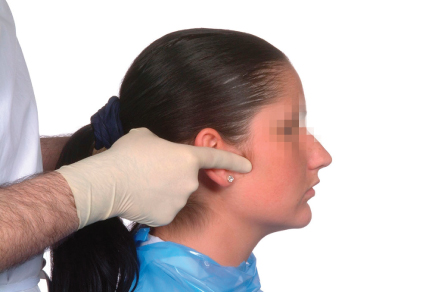
Tenderness is thought to indicate the presence of inflammation in the capsule. Anatomically this area is not as well innervated as the posterior part of the joint, and more useful information can be obtained by intra-auricular palpation.
Intra-Auricular Palpation
TMJ pain and tenderness are mainly related to the area of the posterior bilaminar zone of the disc and the posterior aspect of the capsule. Examination of this area can be achieved more readily and reliably by intra-auricular palpation. This involves placing the little finger in the external auditory meatus on one side at a time and applying gentle forward pressure, while asking the patient to open and close the mouth (Figure 3.6).
Figure 3.6 Intra-auricular palpation of the temporomandibular joint.

Be aware that, if there is acute disc displacement, this method of examination can be very uncomfortable for the patient.
Examination by Manipulation of the Mandible
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


