The Special Needs and Medically Compromised Patient
Learning Outcomes
On completion of this chapter, the student will be able to achieve the following objectives:
• Pronounce, define, and spell the Key Terms.
• Describe the stages of aging in the older population.
• Describe orally related conditions that affect the older patient.
• Describe the importance of the medical history for the medically compromised patient.
• Describe the major medical disorders that can affect a patient’s oral health.
• Describe the type of dental management a medically compromised patient would receive.
Performance Outcome
On completion of this chapter, the student will be able to meet competency standards in the following skill:
Electronic Resources
![]() Additional information related to content in Chapter 29 can be found on the companion Evolve Web site.
Additional information related to content in Chapter 29 can be found on the companion Evolve Web site.
Key Terms
Alzheimer’s (AHLTS-hie-merz) disease A form of progressive mental deterioration that occurs in middle to older age.
Anemia (uh-NEE-mee-uh) A shortage of red blood cells or hemoglobin in the blood, resulting in paleness and weakness.
Angina (an-JYE-nah) Severe chest pain associated with an insufficient supply of blood to the heart.
Arthritis (ahr-THRYE-tis) Inflammation of a joint or many joints, resulting in pain and swelling.
Atrophy (AT-ruh-fee) A wasting away or deterioration.
Bacteremia (bak-tur-EE-mee-uh) Presence of bacteria in the blood.
Bronchitis (bron-KYE-tis) Inflammation of the mucous membranes of the bronchial tubes.
Dementia (duh-MEN-shuh) A mental disorder characterized by loss of memory, concentration, and judgment.
Diabetes mellitus (dye-uh-BEE-teez MEL-e-tus, me-LYE-tus) Metabolic disorder characterized by high blood glucose and insufficient insulin.
Emphysema (em-fi-ZEE-muh) Abnormal increase in the size of the air spaces in the lungs, resulting in labored breathing and an increased susceptibility to infection.
Endocarditis (en-doe-kahr-DYE-tus) Inflammation of the endocardium.
Epilepsy (EH-pi-lep-see) Neurologic disorder with sudden recurring seizures of motor, sensory, or psychic malfunction.
Hemophilia (hee-moe-FIL-ee-uh) Blood coagulation disorder in which the blood fails to clot normally.
Hyperthyroidism (hye-pur-THYE-roid-iz-em, hye-pur-THYE-roi-di-zem) Condition that results from excessive activity of the thyroid gland.
Hypothyroidism (hye-poe-THYE-roid-iz-em, hi-poe-THYE-roi-di-zem) Condition that results from severe thyroid hormone insufficiency.
Leukemia (loo-KEE-mee-uh) A progressive disease in which the bone marrow produces an increased number of immature or abnormal white cells.
Myocardial infarction (mye-oe-KAHR-dee-ul in-FAHRK-shun) Condition in which damage occurs to the muscular tissue of the heart, commonly caused by obstructed circulation; also referred to as a heart attack.
Seizure A sudden attack, spasm, or convulsion that occurs in specific disorders.
Xerostomia (zeer-oe-STOE-mee-uh) Loss of saliva production causing a dry mouth.
Today, just about every dental practice cares for patients with special needs. With major advances in medicine, people are living longer and are surviving medical disorders that in the past would have resulted in disability or premature death. It is estimated that 2% of the national population have some type of disabling condition. These include developmental disabilities, neuromuscular disorders, immunocompromising conditions, cognitive impairment, mental disorders, and trauma.
It is the responsibility of the dentist and the dental team to become knowledgeable and to identify the challenges that face these patients. Patients who enter your dental practice may be ill, in pain, or physically challenged. Your job will be to use good judgment when working with these patients, which may mean bypassing some of the usual routines that take place during an appointment. The dental team and the patient’s medical team must work together to modify dental treatment according to the patient’s needs.
Role of the Dental Assistant
The dental assistant’s role in caring for the special care patient can be divided into three major areas:
The Aging Population
With a declining birth rate and increased longevity, the aging population is the fastest-growing segment of the U.S. population. People age 65 and older make up 13.7 percent of the population and represent about one in every eight persons in the United States. It is estimated that by 2050, people age 65 and older will make up 21 percent of the U.S. population.
Stages of Aging
Aging refers to the irreversible and inevitable changes that occur with time. Most oral conditions that develop in older adults were once believed to be the result of aging, not of disease. Current science is showing that this is not the case. In diagnosis and treatment planning, it is helpful to differentiate signs and symptoms caused by aging from those caused by disease.
Older adults, or persons older than age 65, vary in their psychological and physiologic stages. In agreement with their varying attitudes, characteristics, and needs, older adults can be divided into three categories:
Oral Health of the Aging
The aging population is faced with special oral health issues, and the goal of the dental team for these patients is to factor this into the treatment planning phase (Fig. 29-1). The condition of a patient’s mouth can affect self-esteem, esthetics, nutrition, social interaction, and personal comfort. A person’s general health can actually deteriorate because of poor oral health.

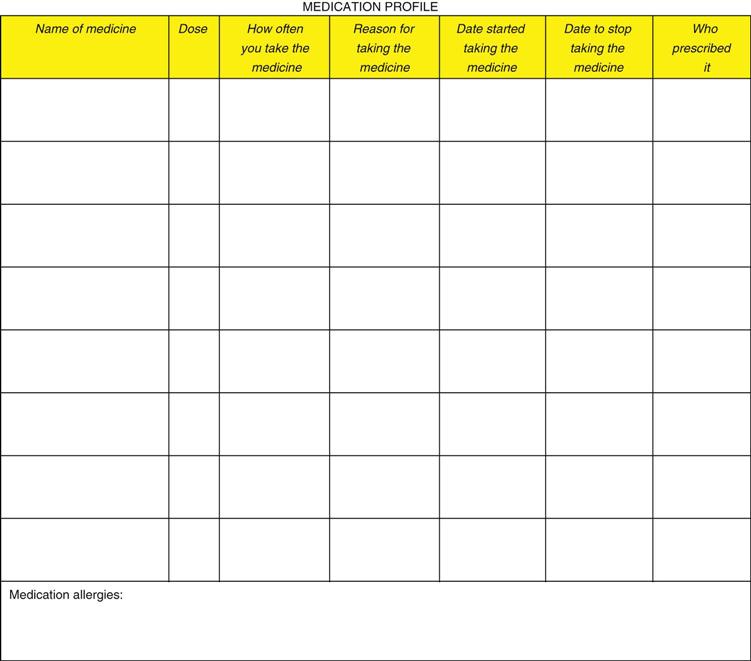
Along with the medical history, it is essential that a medication profile be completed for each patient. One of the hallmarks of disease is the list of prescriptions a patient is taking. These drugs not only indicate the patient’s disease state; they also have potential adverse effects that, along with drug interactions, must be taken into consideration during treatment planning. A medication profile can indicate the severity of a patient’s medical condition (Fig. 29-2).
Oral Health Conditions
The most commonly reported oral health–related conditions that affect the aging population are xerostomia, periodontal disease, tooth decay, dark and brittle teeth, and bone resorption.
Xerostomia
Also known as dry mouth, xerostomia is the result of medical disorders and medications that cause a decreased flow of saliva. More than 400 drugs have the potential to cause dry mouth as an adverse effect. In addition to drug adverse effects, xerostomia is frequently associated with alcoholism, autoimmune disorders, Parkinson’s disease, psychological disorders, dehydration, radiation to the salivary glands, diabetes, Sjögren’s syndrome, and oral breathing.
Periodontal Disease
Periodontal conditions are an increasing problem in the aging population. More than 50 percent of older people may be affected by periodontal disease, and most are unaware of it. As a larger number of older people retain their teeth, periodontal disease will increase (Fig. 29-3). Periodontal disease can be prevented by better oral hygiene and more frequent visits to the hygienist.
Tooth Decay
Studies have shown that older patients have a higher risk of root caries and recurrent decay around old or worn restorations. With aging, often the gums recede, exposing the roots of the teeth. In contrast to the crowns, the roots of the teeth are not protected by enamel, so decay can quickly develop on root surfaces (Fig. 29-4). Root caries can sometimes be prevented by dietary adjustments and changes in oral hygiene care.
Dark and Brittle Teeth
As we age, teeth may darken and become more brittle. This is a result of deposits of secondary dentin that have gradually reduced the size of the pulp chamber. These teeth can then become more susceptible to fracture (Fig. 29-5).
Bone Resorption
When teeth are missing, the patient is partially to fully edentulous. Portions of the alveolar ridge will become compromised and lost (Fig. 29-6). Bone resorption can affect whether the patient will wear a removable prosthesis, as well as the patient’s speech and diet (see Chapter 52).
The Special Needs Patient
Providing dental care to patients with a physical or medical disorder will require increased awareness and attention, and possibly modification of clinical care by the dentist and dental staff. Once the health and medication histories have been obtained from the patient, this information must be used effectively. Each patient should be assessed before treatment can be provided.
An easy technique to use with your patients is to categorize each patient according to how treatment is anticipated to proceed, and what changes are to be made by the dental team:
Specific Disorders of the Medically Compromised Patient
A basic understanding of how a disorder can affect a person’s oral health is important to prevent tooth loss or other complications. Symptoms of more than 100 diseases can indirectly affect a patient by causing a person to be less capable of caring for his or her mouth.
Specific medical and physical disorders are categorized to help you learn and understand the disease and how to care for that specific patient in your practice.
Developmental Disorders
Developmental disorders are the result of an impairment that occurred during the developmental phase (prenatal through age 18) of a person. This impairment can occur prenatally, during birth, or postnatally. Disorders causing a developmental disability can be chromosomal abnormalities such as mental retardation and Down syndrome, autism, cerebral palsy, fetal alcohol syndrome, postnatal infection, or birth anoxia. Many patients with developmental disorders are routinely seen in a pediatric dental office. The pediatric dentist receives extensive education and training on seeing and treating these types of special patients. For more information on oral conditions and clinical management, refer to Chapter 57, Pediatric Dentistry.
Mental Retardation
Mental retardation is impairment in intellectual and adaptive functioning. The cause is not always known; rarely a single cause is identified. Some of the known causes are chromosomal abnormalities, prenatal conditions (rubella, alcohol use, and d/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses