Vital Signs
Learning Outcomes
On completion of this chapter, the student will be able to achieve the following objectives:
• Pronounce, define, and spell the Key Terms.
• List the four vital signs routinely taken in the dental office.
• Describe how metabolism affects a patient’s vital signs.
• Discuss three types of thermometers.
• List common pulse sites used for taking a pulse.
• Describe the characteristics of the pulse that you would look for in taking a patient’s pulse.
• Describe the characteristics of respiration, and explain how they affect a patient’s breathing.
• Describe the best way to obtain accurate readings of respiration.
• Explain the importance of taking a patient’s blood pressure.
• Differentiate the Korotkoff sounds heard when one is taking a patient’s blood pressure.
• Discuss additional techniques used to assess a patient’s health status.
Performance Outcomes
On completion of this chapter, the student will be able to meet competency standards in the following skills:
• Take an oral temperature reading with a digital thermometer.
• Take a patient’s respiration.
• Take a patient’s blood pressure.
Electronic Resources
![]() Additional information related to content in Chapter 27 can be found on the companion Evolve Web site.
Additional information related to content in Chapter 27 can be found on the companion Evolve Web site.
![]() and the Multimedia Procedures DVD
and the Multimedia Procedures DVD
Key Terms
Antecubital (an-tee-KYOO-bi-tul) space Small groove or fold in the inner arm, at or “in front of” (ante) the elbow (cubitus).
Arrhythmia (uh-RITH-mee-uh) Abnormality and irregularity in the force or rhythm of the heartbeat.
Blood pressure (BP) Pressure exerted by the blood against the walls of the blood vessels.
Brachial (BRAY-kee-uhl) Relating to the arm (brachium), as in brachial artery.
Carotid (kuh-ROT-id) Relating to either of the two major arteries on each side of the neck that carry blood to the head.
Depth In respiration, the amount of air in a breath.
Diastolic (dye-uh-STOL-ik, dye-uh-STAHL-ik) The normal rhythmic relaxation and dilation of the heart chambers.
Electrocardiogram (ee-lek-tro-KAHR-dee-oe-gram) Instrument used in the detection and diagnosis of heart abnormalities. It generates a record of the electrical currents associated with heart muscle activity.
Korotkoff (kuh-ROT-kof) sounds Specific sounds heard when one is taking a blood pressure.
Metabolism (muh-TAB-uh-liz-um) Physical and chemical processes that occur within a living cell or organism and are necessary for the maintenance of life.
Oximetry (ok-SIM-uh-tree) Measurement of oxygen concentration in the blood.
Palpate (PAL-payt) To examine or explore by touching.
Pulse Rhythmic throbbing of the arteries produced by regular contractions of the heart.
Radial Related to the radius (bone) or forearm (antebrachium), as in radial artery.
Rate A quantity measured, as in breaths and heartbeats.
Respiration Act or process of inhaling and exhaling; breathing.
Rhythm A sequence or pattern, such as the heartbeat or breathing.
Sphygmomanometer (sfig-moe-muh-NOM-e-tur) Instrument for measuring blood pressure in the arteries.
Stethoscope Instrument used for listening to sounds produced within the body.
Systolic (sis-TOL-ik) Rhythmic contraction of the heart, especially of the ventricles.
Temperature Degree of hotness or coldness of a body or an environment.
Thermometer Instrument for measuring temperature.
Tympanic (tim-PAN-ik) Related to or resembling a drum, as in the tympanic membrane, or eardrum.
Volume Quantity or amount, as in force of a heartbeat.
Attention toward a patient’s immediate health should be the first priority of every healthcare provider. By taking a patient’s vital signs on a routine basis before dental treatment is provided, the dental team is confirming that the patient’s health status is at a level of well-being. It is crucial that you gain confidence in both the background knowledge and the practical application of taking a patient’s vital signs.
Vital signs consist of taking and recording a person’s temperature, pulse, respiration, and blood pressure. If this is the patient’s first visit, 6-month recall, or a medical emergency, the clinical assistant should routinely take and record the vital signs. This type of baseline information provides the dental team with assurance regarding the patient’s well-being and health status.
Factors that Affect Vital Signs
The human body is influenced by both emotional and physical factors. Prior to a dental appointment, for example, the patient may have had a hot or a cold beverage, either of which would alter the oral temperature. Or, a patient may be fearful of an upcoming injection; thus, his or her blood pressure and respiration may be higher than at a previous reading.
If a patient were to come directly to a dental appointment from a workout at the gym, what changes would you expect to see in the patient’s vital signs? If you predicted an elevation in the patient’s temperature, pulse, respiration, and blood pressure, you are correct. When an increase in metabolism occurs (such as during strenuous exercise), vital sign measurements also typically increase.
One of your responsibilities as a dental assistant is to inquire about and recognize these situations and help the patient relax before taking his or her vital signs. You may need to take these measurements more than once. If you think the patient is abnormally anxious, provide reassurance, wait several minutes, and then repeat the procedure.
Temperature
Body temperature is the degree of hotness or coldness of the body’s internal environment. The process of physical and chemical changes that take place in the production of the body’s heat is called metabolism. A healthy person’s temperature will vary slightly throughout the day because of the quantity of stimuli that it encounters. A person’s lowest body temperature occurs in the early morning hours, and the highest temperature occurs in the evening.
During an illness, a person’s metabolism increases for the purpose of elevating the body’s temperature. Most bacteria and viruses cannot survive in excess heat, and this is the body’s way of defending against such diseases. Have you ever wondered why you become chilled when you have a fever? When fever is present, the blood vessels closest to the surface of the skin constrict, producing “goose bumps.” The body’s reaction to these goose bumps is to make you shiver. A chain reaction then begins, causing the body to produce internal heat for warmth.
Temperature Readings
The thermometer is the instrument used to measure body temperature. Temperature readings are calibrated according to the Fahrenheit (F) or the Celsius (C) scale. The Fahrenheit scale is the reading most frequently used in the United States, and the Celsius scale is used most frequently in Canada and Europe.
The average range of oral temperature of a resting person is 97.6° F to 99° F (36.4° C to 37.3° C). The average body temperature is higher in infants and younger children than in adults.
Several areas of the body can be used to obtain a temperature reading. The thermometer can be placed under the tongue, in the ear, under the arm, or in the rectum. Temperature readings vary according to the body site used.
Types of Thermometers
Digital
Digital thermometers are more popular today because of their convenience (Fig. 27-1). These thermometers are battery operated, and function on the same theory as a glass thermometer, except that a timing system shows a digital reading after 30 seconds, rather than a line of mercury that expands (“rises”) along a marked scale. It is important to remember the timed feature of the digital thermometer because you may attain an inaccurate reading if the battery is low.
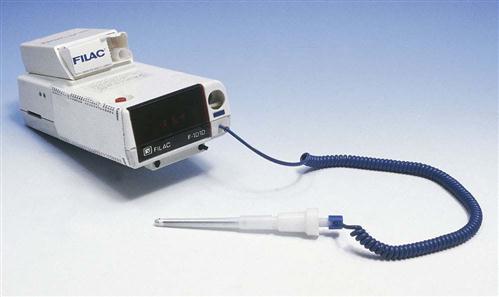
A disposable plastic sheath slides over the probe before insertion. Most digital thermometers emit a “beeping” sound that indicates completion, with the reading appearing on the digital screen. Procedure 27-1 reviews the use of a digital thermometer.
Tympanic
One of the newest techniques used to take a patient’s temperature involves the ear canal (a tympanic reading). The ear canal is a protected cavity, so the tympanic temperature reading is not affected by an open mouth, hot or cold drinks, or nose congestion. The tympanic thermometer has a much smaller probe, which is gently placed into the ear canal (Fig. 27-2). An infrared signal is bounced off the eardrum, and an accurate reading is provided within 2 seconds. The risk of spreading communicable diseases while taking a temperature tympanically is greatly reduced because the covered probe of the thermometer does not actually touch the eardrum. This approach has become very popular in younger children. The rapid measurement may be more accurate because less patient movement occurs.
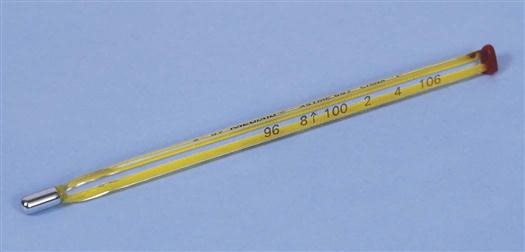
Glass
The glass thermometer is a glass tube with a small mercury bulb at the end that comes in contact with body tissue (Fig. 27-3). When it touches warm tissues of the body, the mercury expands and “rises” along a marked numeric scale. After 3 minutes, the mercury stops expanding and registers its highest reading.
Mercury thermometers historically have proved to be a useful measuring device over many years and can still be found in a few clinical settings. Mercury is a toxic substance that can harm both humans and wildlife. Many states have banned the use of mercury thermometers because of these health hazards. In 1998, the American Hospital Association (AHA) signed an agreement with the U.S. Environmental Protection Agency (EPA) to commit to the elimination of mercury from hospital waste. Furthermore, in July 2001, the American Academy of Pediatrics urged doctors and parents to stop using mercury thermometers.
Pulse
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses