Chapter 26
Traumatic Dental Injuries
Traumatic dental injuries (TDI) are the most common of the oral and maxillofacial injuries. More or less all clinicians, general practitioners and specialists, meet such patients, either in the emergency phase or later as a consequence of the trauma. The prognosis for some TDI depends very much on correct early emergency management at the place of accident and at the clinic immediately after the accident. This chapter presents how to diagnose, classify, and treat TDI with emphasis on the emergency phase.
Epidemiology of Traumatic dental Injuries and Relation to Oral and Somatic Injuries
Oral injuries (dental, soft tissue, and bone) caused by trauma occur very frequently. They are most common during the first 12 years of life and are rare after the age of 30. In contrast, other bodily injuries are most frequently seen at ages 15–25 years and occur throughout life (Fig. 26.1).
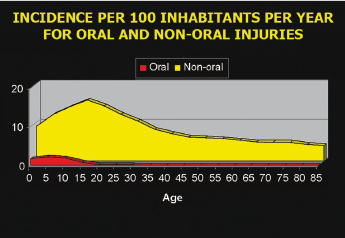
Of all patients presenting with oral injuries, TDI is the most common oral injury (92%), followed by orofacial soft tissue injuries (28%); whereas fractures of the maxillofacial bones are relatively rare and seen in only 6% of such patients. The annual incidence of TDI is 1–2% of the population. The prevalence is high and every fourth boy and every fifth girl will have already sustained dental injuries by the age of 14. One in five children has sustained a TDI to the permanent teeth before leaving school and one in four adults has evidence of TDI. Due to the high number of injured individuals and often complex treatment, TDI are associated with high costs for society and the individual.
The prognosis of treatment for some dental injuries, and especially for avulsed teeth, depends very much on early and correct management at the place of the accident and during emergency treatment at the clinic.
Examination and Diagnosis of Dental Injuries
History taking is important with regard to when, where, and how the injury occurred, as well as to the patient’s general health and possible medication. Be alert to other injuries and symptoms indicating more serious injuries. It is also of value to ask what has been done before the patient reached the clinic, such as any treatment carried out elsewhere and how avulsed teeth have been stored.
A brief summary is given here of the important issues for emergency examination and for TDI. For an overview of evaluation of patients with more severe maxillofacial injuries, see Chapter 27. As for oral and maxillofacial injuries, it is important to examine and treat TDI in a systematic way. “Examine from the outside towards the inside and treat from the inside towards the outside” is a helpful principle for a systematic approach for examining oral injuries. Suturing of lips should ideally be carried out after intraoral emergency examination and emergency treatment has been performed, otherwise it may be difficult to enter the oral cavity once edema has started to develop.
The possibility of inhaling or swallowing teeth at the time of injury should always be considered when teeth, parts of the teeth, or prosthetic appliances are missing. This is especially important in the unconscious patient; if there is reason to suspect inhalation or swallowing of a tooth or dental appliance, it is important that radiographs of the chest and the abdomen are considered. Inhalation of foreign bodies is normally associated with symptoms such as coughing but may also occur in a conscious patient without producing symptoms.
Examination of crowns of teeth should be carried out in order to look for presence and extent of fractures and pulp exposures. Crown–root fractures in the molar and premolar regions should be expected when there has been an indirect trauma such as a blow to the chin. Crown–root fractures in one quadrant are very often accompanied by similar fractures on the same side of the opposing jaw. For this reason it is therefore necessary to examine occlusal fissures of all molars and premolars to detect possible fractures (Fig. 26.2).

The fracture surface should be carefully examined for the extent of fracture in dentin and pulp exposures (Fig. 26.3). When pulp is exposed, the size and location should be recorded. In some cases, the dentin layer may be so thin that the outline of the pulp can be seen through the dentin wall. One should take care not to perforate the thin dentinal layer during the examination.

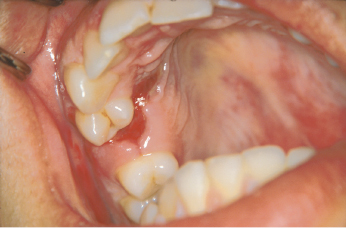
Displacement and avulsion of teeth are usually evident by visual examination; however, minor abnormalities can often be difficult to detect. In such cases, it is helpful to examine the occlusion as well as radiographs taken at various angulations. In cases of tooth luxation, the direction of the dislocation as well as extent should be recorded. It is important to remember that, apart from displacement and interference with occlusion, laterally luxated and intruded teeth present very few clinical symptoms (Fig. 26.4). Moreover, these teeth are normally firmly locked in their displaced position and do not usually demonstrate tenderness to percussion. While radiographs can be of assistance, diagnosis is confirmed by the percussion tone, when tapping on the tooth with the handle of an instrument. A high, bony percussion tone is registered compared to the normal sound of uninjured teeth. In contrast, when a Le Fort I level midface fracture is present a change in percussion sound to a crack-like sound can be noticed.

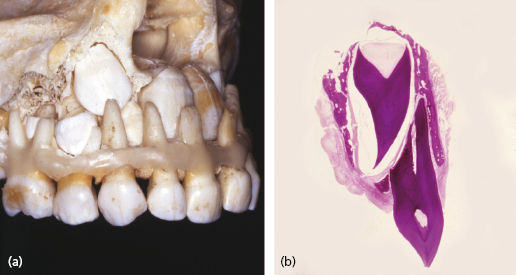
In the primary dentition, it is of utmost importance to diagnose the direction of dislocation of the apex of a displaced primary tooth, since this tooth is located in close relationship to the permanent successors and can impinge on the development of the permanent successor (Fig. 26.5). This diagnosis is often best made by palpating the alveolar process from a vestibular approach.
The patient may also react with pain to percussion of a tooth which is indicative of damage to the periodontal ligament. As with all examination techniques used at the time of injury, the percussion test should be started on a non-injured tooth to ensure a reliable patient response. In smaller children, the use of a fingertip can be a gentler diagnostic tool.
Patients can usually detect and guide the examiner to the place where there has been a change in the occlusion. Abnormalities in occlusion can indicate fractures of the jaw, alveolar process or a lateral luxation (Figs 26.6, 26.7, 26.8). All teeth should be tested for abnormal mobility, both horizontally and axially. It should be remembered that erupting teeth and primary teeth undergoing physiologic root resorption always exhibit some mobility. The typical sign of alveolar fracture is movement of adjacent teeth when the mobility of a single tooth is tested (Fig. 26.6). Palpation of the alveolar process is important for detection of fractures with dislocations.


When mobility of a tooth is detected it is not possible to discriminate between luxation injuries and root fractures without radiographic examination (Figs 26.9, 26.10). The site of the root fracture will have an influence on the degree of mobility.


Pulp testing following traumatic injuries is a controversial issue. These procedures require cooperation and a relaxed patient, in order to avoid false reactions. However, this is often not possible during initial treatment of injured patients, especially children. The interpretation of pulpal sensibility tests performed immediately after traumatic injuries is complicated by the fact that sensitivity responses can be temporarily or permanently decreased, especially after luxation injuries. However, repeated testing has shown that normal reactions can return after a few weeks or months. Moreover, teeth which have been loosened can elicit pain responses merely from pressure of the pulp testing instrument. It is therefore important to reposition and immobilize such teeth, e.g. root-fractured or extruded incisors, prior to pulp testing. Another important factor to consider when testing the pulp is the stage of eruption; teeth under root development sometimes show an unreliable response. Teeth undergoing orthodontic movement display higher excitation thresholds. If local anesthetics are to be administered for various treatment procedures, pulp testing should be performed prior to doing this. Pulpal sensibility testing is difficult in the emergency situation but it is helpful, as such tests have a strong predictive value for later pulp healing complications. For this reason it is important to carry out a sensibility test within the first week after trauma to establish a point of reference for evaluating pulpal status at later follow-up examinations.
Radiographic Examination of TDI
This is an overview of suitable examinations for patients who have been subjected to dentoalveolar trauma.
Dental Films
All injured teeth should be examined radiographically to diagnose injuries and to reveal the stage of root formation which is important for the choice of treatment method. The ideal method is the use of different angulations for each traumatized tooth, using a standardized projection technique. Thus, a traumatized anterior region of the maxilla is covered by one occlusal film, projected steeply superiorly, and three periapical exposures perpendicular to the long axes of the teeth, where the central beam is directed between the central incisors and for each lateral incisor. This procedure ensures diagnosis of even minor dislocations or root fractures. It is important to bear in mind that a steep occlusal exposure is of special value in the diagnosis of root fractures and lateral luxations with oral displacement of the crown.
Most root fractures are disclosed by radiographic examination provided that they are steeply superiorly projected. A widening of the periodontal space is seen in lateral and extrusive luxations, whereas intruded teeth often demonstrate a lack of periodontal space.
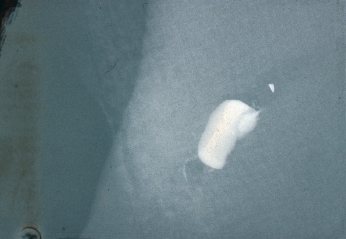
Extraoral radiographs may be of value for determining the direction of dislocation of intruded primary incisors. Dislocated tooth fragments within a lip laceration can be demonstrated radiographically by the use of an ordinary film placed between the dental arches and the lips (Fig. 26.11). A short exposure time is advocated for this situation.
Panoramic Technique
This method gives an excellent overview of the dentoalveolar region. It is especially useful in cases where a jaw fracture is suspected.
Computed Tomography Scanning
This is a very useful method in the diagnosis of maxillofacial fractures; however, the resolution is not high enough and radiation exposure is too high to make it useful for dental trauma diagnosis. Cone-beam CT has high enough resolution to be a valuable tool for diagnosis of different dental injuries (Fig. 26.12).

Classification and Clinical Findings
TDI can be classified in many ways but the following system based on World Health Organization classification, modified by Andreasen, is well suited to the clinical situation; following this system facilitates treatment.
Injuries to the Hard Dental Tissues and the Pulp
A schematic overview of hard tissue injuries is presented in Figure 26.13.
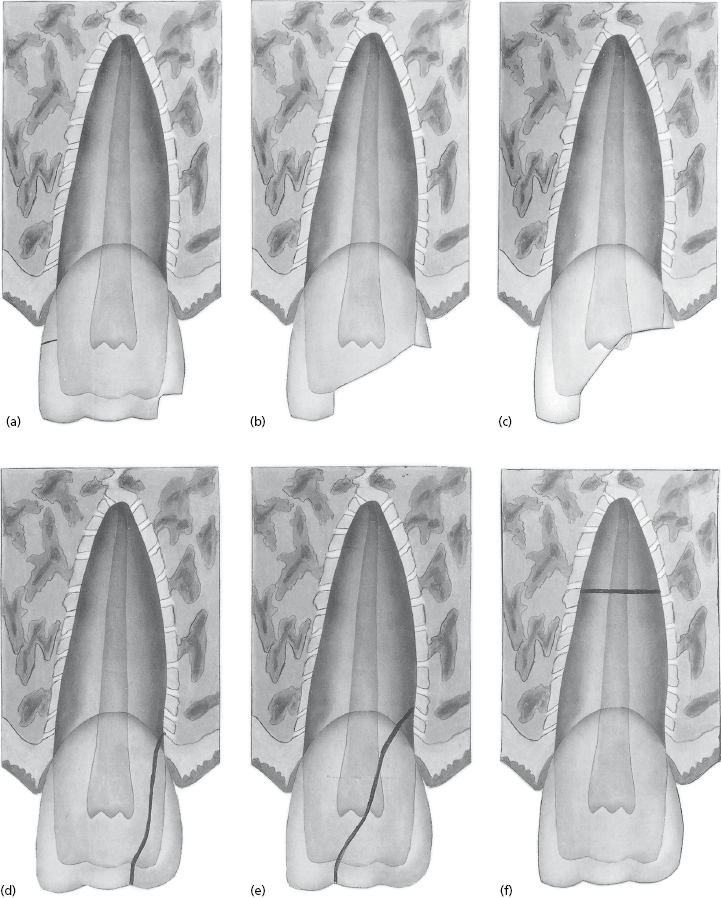
Crown Infraction
This is incomplete fracture of the enamel without loss of tooth substance (Fig. 26.13a mesial side). Various patterns of craze lines can be detected depending on the location and direction of trauma, e.g. vertical, horizontal, or oblique lines.
Uncomplicated Crown Fracture
This is a fracture with loss of tooth substance (Fig. 26.13a distal and Fig. 26.13b). It involves enamel or enamel and dentin without pulp exposure. The exposed dentin usually gives rise to symptoms such as sensitivity to hot and cold stimuli and mastication.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


