Chapter 23
Principles of Oral Cancer Management
Epidemiology and Risk Factors
The incidence of oral squamous cell carcinoma, particularly in younger patients, is increasing in North America and the UK. In certain regions of the world, such as India, oral cancer is one of the most common malignancies. In these regions of the world the use of betel nut and betel quid clearly contribute to the high incidence of oral cancer. However, the etiology in the western portions of the world is less clear. Survival rates for oral cancer patients have not changed significantly. The roles of tobacco and alcohol are firmly established as risk factors for oral cancer. However, approximately 33% of oral squamous cell carcinoma patients were never smokers. Our understanding of the role of smokeless tobacco in oral carcinogenesis has gone through considerable evolution over the last three decades. The conclusion of a recent review of 32 relevant studies published between 1920 and 2005 concluded that smokeless tobacco, at most, plays only a minor role in the development of oral cancer. There has been considerable confusion regarding the role of human papillomavirus (HPV) in the development of oral cancer. Based on the available studies there is a lack of reproducible molecular data supporting the role of HPV in the development of oral cancer. This is in contrast to oropharyngeal carcinogenesis where HPV has a much stronger etiologic role.
Histologic Grading, Tumor Staging, and Clinical Behavior
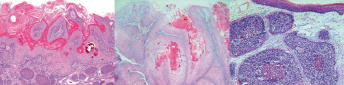
Ninety-five percent of oral cancers are squamous cell carcinoma (SCC). Different histologic variants of SCC include verrucous SCC, basaloid SCC, and papillary SCC (Fig. 23.1). Clinicians and investigators have attempted to use the combination of clinical information and histologic findings to predict the behavior of oral SCC. The histologic features that have been evaluated include tumor differentiation, tumor thickness, tumor size, and tumor invasive pattern.
Proliferative Verrucous Leukoplakia
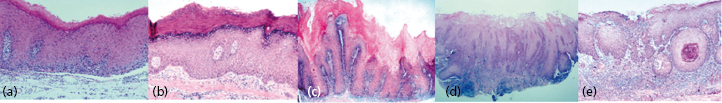
Most oral SCCs are preceded by clinically evident precancerous oral lesions, most often oral epithelial dysplasia, which appears as white (leukoplakia) or red patches (erythroplakia) that are characterized microscopically by varying degrees of dysplasia (from mild to severe). Other oral SCCs are preceded by proliferative verrucous leukoplakia (PVL), a condition which is persistent, recurrent, and multifocal (Fig. 23.2). Dysplasia has an unpredictable transformation rate to oral SCC that is thought to be approximately 16%, whereas the transformation rate for PVL is much higher (50–70%). In contrast to oral dysplasia, PVL is not associated with tobacco or alcohol consumption. In addition, whereas dysplasia is more common in men, the female to male ratio for PVL is about 4 to 1. At initial presentation, PVL lesions are white, irregular areas on the attached gingiva, buccal mucosa, and tongue. Histologically, PVL exhibits no dysplasia or mild dysplasia. In spite of the bland clinical and histologic appearance of early lesions, PVL is characterized by relentless growth and irreversible progression through a continuum of lesions, namely, hyperkeratosis, verruciform hyperkeratosis, verrucous hyperplasia, verrucous carcinoma, and ultimately SCC (Fig. 23.3). Repeated surgical excisions of all clinically and histologically appearing abnormal tissue can slow the transformation to carcinoma. However, such treatment results in significant disfigurement and morbidity.

Preoperative Assessment, Staging, and Work-Up
Most oral cancers are painful, and it is the most common presenting symptom. For oral cancer patients, pain severely limits oral function including eating, drinking, and talking. Pain is rated as the oral cancer patient’s worst symptom and is the primary determinant of a poor quality of life. Opioids, such as morphine, are the only drugs that have any efficacy for oral cancer pain. Morphine provides minimal relief, does not restore oral function and progressively larger doses are required; therefore, tolerance rapidly develops. Pain management should be tailored to provide relief when patients are required to function. Total resection of the oral cancer produces near complete relief. Overall, approximately 50% of oral cancer patients will not be cured with surgery, chemotherapy, or radiation therapy.
The tobacco history should be reviewed and the patient should be classified as a never smoker, non-smoker, or smoker. If the patient is a smoker or non-smoker the pack-years of use should be calculated. If the patient is a non-smoker the time since the patient’s last cigarette should be determined. While there is conflicting data in the literature as to whether marijuana use contributes to oral carcinogenesis, patients should be asked whether and how much marijuana they use.
Systematic palpation of the neck should be performed on every patient at every visit. Palpation of the neck should be performed on one side of the neck at a time and should always be performed from behind the patient. The sensitivity of clinical examination to detect metastasis, however, is little better than 50%. A panoramic radiograph should be performed in almost all cases of oral cavity SCCs. Even if the carcinoma does not involve the maxilla or the mandible, the dentition should be evaluated prior to surgery to determine whether extractions will be required at the time of surgical resection if postoperative radiation therapy is anticipated. Nasopharyngoscopy can be easily and painlessly performed with proper preparation of the nasopharyngeal membranes with local anesthetic and a topical vasoconstrictor. Nasopharyngoscopy can be used to evaluate the nasopharynx, base of tongue, and supraglottic structures.
The significant limitations of imaging for detecting carcinoma need to be considered when evaluating the oral cancer patient, par/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


