Chapter 22
Potentially Malignant Disorders of the Oral Mucosa
Many terms have been used to describe oral premalignancies that may have a potential to transform into cancers of the oral mucosa. These include “precancer”, “premalignant”, “precursor lesions”, “intraepithelial neoplasia”, and “potentially malignant”. The World Health Organization (WHO) Collaborating Center proposed that oral mucosal presentations recognized as precancerous can be classified into two major groups: as precancerous lesions and precancerous conditions. A precancerous lesion was defined as “a morphologically altered tissue in which oral cancer is more likely to occur than in its apparently normal counterpart”. On the other hand, a precancerous condition is defined as “a generalized state associated with a significantly increased risk of cancer”. This classification was based on the concept that the origin of malignancy in the oral mucosa of a patient with a precancerous lesion would correspond with the specific local site of precancer; whereas a malignancy may arise in any part of the oral mucosa in a precancerous condition.
Precancerous lesions include leukoplakia, erythroplakia, and palatal keratosis associated with reverse smoking, and precancerous conditions include sideropenic dysphagia, lichen planus, oral submucous fibrosis, syphilis, discoid lupus erythematosus, xeroderma pigmentosum, and epidermolysis bullosa.
There may need to be some modification of this concept since it is now known that even clinically normal-looking oral mucosa in patients with a precancerous lesion on one side of the oral cavity may have dysplasia or molecular abnormality on the contralateral side, suggesting the possibility of malignant transformation, and that cancer could subsequently develop in the normal-appearing mucosa.
Histology (Grading of Dysplasia)
Histological changes that may be observed in potentially malignant disorders of the oral mucosa can be expressed as oral epithelial dysplasia. Although the clinical appearance of oral epithelial dysplasia is variable, oral squamous malignancies of the lining mucosa are known generally to develop from dysplastic surface epithelium of the oral mucosa. The grade of epithelial dysplasia can be expressed in several categories, such as no dysplasia, mild dysplasia, moderate dysplasia, and severe dysplasia. The relationship of epithelial dysplasia in various grades to the subsequent development of cancer has not been fully clarified. However, it is generally believed that any degree of epithelial dysplasia, even a mild form, indicates an increased risk, and severe dysplasia suggests a very high risk of the subsequent development of cancer.
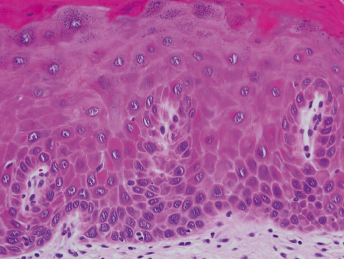
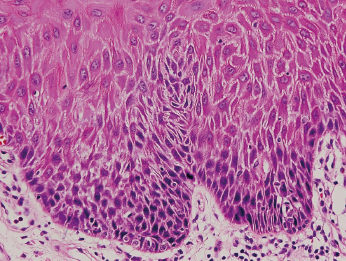
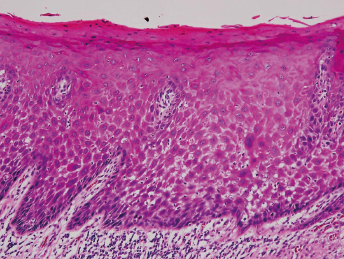
Histologically, grade 1 (mild dysplasia) demonstrates general architectural disturbance limited to the lower third of the epithelium accompanied by cytological atypia (Fig. 22.1). Grade 2 (moderate dysplasia) demonstrates architectural disturbance extending into the middle third of the epithelium (Fig. 22.2). Grade 3 (severe dysplasia) starts with greater than two-thirds of the epithelium showing architectural disturbance with associated cytological atypia. However, architectural disturbance extending into the middle third of the epithelium with sufficient cytological atypia is upgraded from moderate to severe dysplasia (Fig. 22.3).
The term carcinoma in situ (CIS) denotes that malignant transformation has occurred but invasion is not present.
Potential molecular biological markers or molecular genetics of potentially malignant disorders of the oral mucosa, which may have special association with progression of oral epithelial dysplasia to carcinoma, have been studied. Loss of heterozygosity (LOH) at 3p and 9p increase the risk of progression of dysplasia to squamous cell carcinoma (SCC). Mutation of p53 tumor suppressor gene is one of the most common genetic events in carcinogenesis. Although LOH at the p53 loci appears to be associated with progression, mutation of the p53 gene is rare in dysplasia and appears to be a late event. The p53 protein and other markers of apoptosis appear in basal and parabasal layers of dysplastic lesions that progressed to SCC.
Potentially Malignant Disorders of the Oral Mucosa
Leukoplakia
The WHO working group defines leukoplakia as: “The term leukoplakia should be used to recognize white plaques of questionable risk having excluded (other) known diseases or disorders that carry no increased risk for cancer.”
Leukoplakia itself has no specific histology, it may show atrophy or hyperplasia (acanthosis), and may or may not demonstrate epithelial dysplasia.
Oral leukoplakia occurs most frequently on the lip vermillion, buccal mucosa, lateral border of tongue, floor of mouth, and gingival mucosa. The clinical finding of leukoplakia has been reported using various terms, but classification into two types is generally accepted: homogeneous and non-homogeneous leukoplakia, based on surface color and morphologic characteristics. Homogeneous leukoplakias look uniformly flat and thin (Fig. 22.4). Non-homogeneous leukoplakias include several subtypes:
- Speckled type – mixed appearance of white and red, but still retaining predominantly white character.
- Nodular type – small polypoid outgrowths with rounded red or white excrescences.
- verrucous type – wrinkled or corrugated surface appearance.
- Erythroleukoplakia is one type of non-homogeneous leukoplakias. It is very similar to speckled type leukoplakia and appears white and red, with red areas of minimal keratin production interspersed among the background of white areas with thickened keratin. The red areas of erythroleukoplakia are larger than in speckled type leukoplakia, and eryt/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


