Maxillary Posterior Edentulism
Treatment Options for Fixed Prostheses
Carl E. Misch
Maxillary posterior partial or complete edentulism is one of the most common occurrences in dentistry. Seven percent of the adult population in the United States (12 million people) are missing all of their maxillary teeth and have at least some mandibular dentition—a condition that occurs 35 times more frequently than complete mandibular edentulism opposing maxillary teeth.1,2 The complete edentulous rate of the adult population is 10.5%. Therefore, 30 million people in the United States or 17.5% of the adult population are missing all of their maxillary teeth. In addition, 20% to 30% of the adult partially edentulous population older than 45 years of age are missing maxillary posterior teeth in one quadrant, and 15% of this age group are missing maxillary dentition in both posterior regions.2 In other words, approximately 40% of adult patients are missing at least some maxillary posterior teeth. Therefore, the maxillary posterior region is one of the most common areas to be involved in an implant treatment plan to support a fixed or removable prosthesis.
The maxillary posterior edentulous region presents many unique and challenging conditions in implant dentistry. However, existing proven treatment modalities make procedures in this region as predictable as in any other intraoral region. Most noteworthy surgical methods include sinus grafts to increase available bone height, onlay grafting to increase bone width, and modified surgical approaches to insert implants in poorer bone density.3 This chapter addresses the treatment planning concepts specific to the maxillary posterior partial or complete edentulous regions.
Implant Treatment Plan–Related Factors
Several conditions make the posterior maxilla unique in the development of an ideal treatment plan. These items include bone width, crown height space (CHS), bone density, bone height, occlusal forces, implant size, implant number, and implant design (Box 22-1).
Bone Width
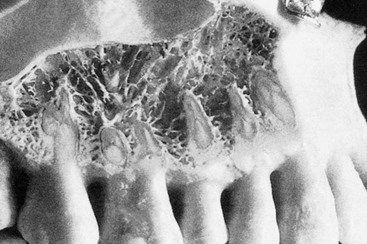
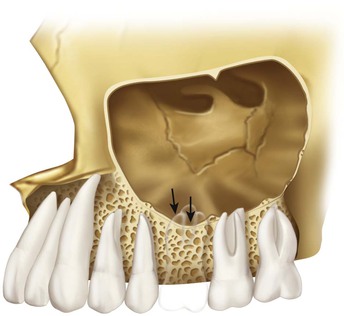
The dentate posterior maxilla has a thinner cortical plate on the facial compared with the mandible. In addition, the trabecular bone of the posterior maxilla is finer than in other dentate regions (Figure 22-1). The loss of maxillary posterior teeth results in an initial decrease in bone width at the expense of the labial bony plate. The width of the posterior maxilla decreases at a more rapid rate than in any other region of the jaws.4 The resorption phenomenon is accelerated by the loss of vascularization of the alveolar bone and the existing fine trabecular bone type. However, because the initial residual ridge is so wide in the posterior maxilla, even with a 60% decrease in the width of the ridge, adequate-diameter root form implants usually can be placed.
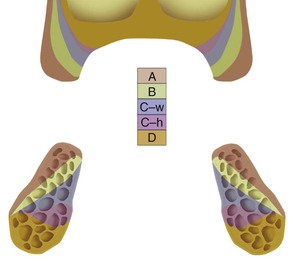
Unlike the resorbed atrophic mandible, the maxillary posterior resorbed ridge progressively shifts toward the palate until the ridge is resorbed into a medially positioned narrower bone volume5 (Figure 22-2). This results in the buccal cusp of the maxillary final restoration in the moderate to severe atrophic ridges often being facially cantilevered to satisfy esthetic requirements at the expense of biomechanics for occlusal loading (Figure 22-3).
Crown Height Space
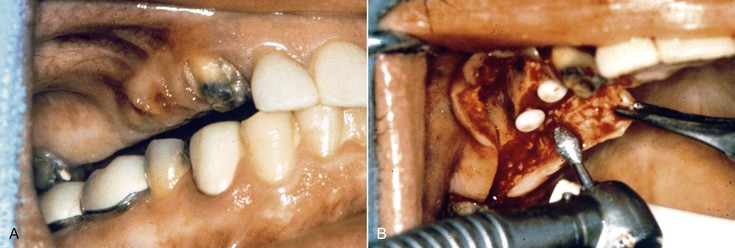
The CHS should be evaluated before implant placement. After the occlusal plane is properly restored or modified, the CHS ideally should be greater than 8 mm for a fixed restoration and 12 mm for an implant overdenture. It is not uncommon for excess tissue thickness to be present in this region, and when less clinical space is available for prosthodontic reconstruction due to gingival thickness, a gingivectomy is first considered. However, if tissue reduction cannot correct the clinical crown height problem, osteoplasty or vertical osteotomy of the maxillary posterior alveolar process is indicated to restore the correct ridge orientation before surgery (Figure 22-4). This procedure may reduce the available bone height. Sinus grafting to restore vertical height is very predictable. Therefore, after an osteoplasty, a sinus floor grafting is often required to increase the CHS and still allow implants of adequate length to restore the patient.
Poor Bone Density
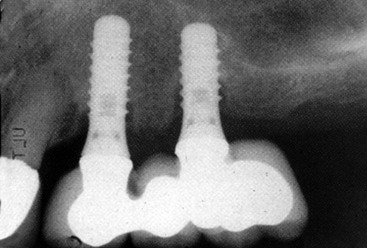
In general, the bone quality is poorest in the edentulous posterior maxilla compared with any other intraoral region.6 A literature review of clinical studies from 1981 to 2001 reveals the poorest bone density may decrease implant loading survival by an average of 16% and has been reported as low as 40%.7 The cause of these failures is related to several factors. Bone strength is directly related to its density, and the poor density bone of this region is often five to 10 times weaker compared with bone found in the anterior mandible.8 Bone densities directly influence the percent of implant–bone surface contact, which accounts for the force transmission to the bone. The bone–implant contact (BIC) is least in D4 bone compared with other bone densities (Figure 22-5). The stress patterns developed in poor bone density migrate farther toward the apex of the implant. As a result, bone loss is more pronounced and more often occurs along the implant body rather than only crestally as in other denser bone conditions. Type IV (D4) bone also exhibits the greatest biomechanical elastic modulus difference when compared with titanium under load.8 This biomechanical mismatch develops a higher strain condition to the bone, which may be in the pathologic overload range. As such, strategic choices to increase bone–implant contact are suggested.

In the posterior maxilla, the deficient osseous structures and an absence of cortical plate on the crest of the ridge further compromise the initial implant stability at the time of insertion (Figure 22-6). The labial cortical plate is thin, and the ridge is often wide. As a result, the lateral cortical BIC to stabilize the implant is often insignificant. Therefore, initial healing of an implant in D4 bone is often compromised, and clinical reports indicate a poorer initial healing success than with D2 or D3 bone.
Bone Height
Local anatomical conditions of the edentulous alveolar ridges in the posterior maxilla may be unfavorable for implant placement. The available alveolar bone height is lost in the posterior maxilla as a result of periodontal disease before tooth loss. The maxillary molar regions have distal furcation involvement frequently because the furca is directly under the distal contact and has no facial or palatal access for hygiene. The furca is also narrower than many dental curettes, and it is difficult to eliminate calculus after it has formed. As a result, periodontal disease is common and is associated with loss of bone height before tooth loss.
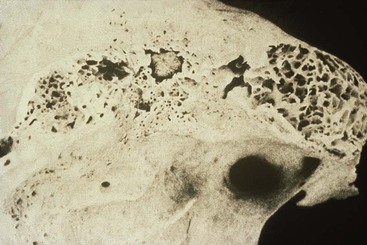
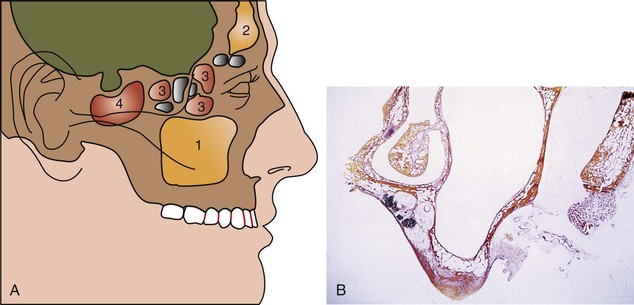
Although the maxillary sinus maintains its overall size while the teeth are present, an expansion phenomenon of the maxillary sinus occurs with the loss of posterior teeth9 (Figure 22-7). The antrum expands in both inferior and lateral dimensions. This expansion after loss of posterior teeth may even invade the canine eminence region and proceed to the lateral piriform rim of the nose. It also expands toward the crest of the edentulous ridge, often until only a thin layer of cortical bone separates the antrum from the crest of the residual ridge (Figure 22-8). The sinus expansion is more rapid than the crestal bone height changes. The dimension of available bone height of the posterior maxilla is greatly reduced as a result of dual resorption from the crest of the ridge and pneumatization of the sinus after the loss of teeth. As a result of the inferior sinus expansion, the amount of available bone in the posterior maxilla greatly decreases in height. As a consequence, knowledge of the maxillary sinus and bone augmentation to the antral floor is necessary to develop an ideal treatment plan.
Maxillary Sinus Anatomy
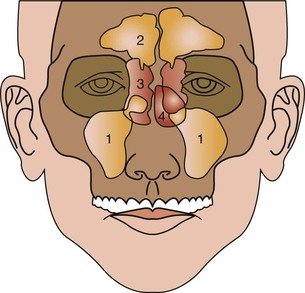
The maxillary sinuses were first illustrated and described by Leonardo da Vinci in 1489 and later documented by the English anatomist Nathaniel Highmore in 1651. The maxillary sinus or antrum of Highmore lies within the body of the maxillary bone and is the largest and first to develop of the paranasal sinuses (Figure 22-9). Adult maxillary sinuses are pyramid-shaped, air-filled cavities that are bordered by the nasal cavity. There is much debate about the actual function of the maxillary sinus. Possible theorized roles of the sinus include weight reduction of the skull, phonetic resonance, participation of warming and humidification of inspired air, and olfaction. A biomechanical adaptation of the maxillary sinus directs forces away from the orbit and cranial cavity when a blow is delivered to the midface.10
Expansion of the Maxillary Sinus
A primary pneumatization of the maxillary sinus occurs at about 3 months of fetal development by an outpouching of the nasal mucosa within the ethmoid infundibulum. At that time, the maxillary sinus is a bud situated at the infralateral surface of the ethmoid infundibulum between the upper and middle meatus.11 Prenatally, a secondary pneumatization occurs. At birth, the sinus is still an oblong groove on the mesial side of the maxilla just above the germ of the first deciduous molar, and the sinus cavities are filled with fluid.9 Postnatally and until the child is 3 months old, the growth of the maxillary sinus is closely related to the pressure exerted by the eye on the orbit floor, the tension of the superficial musculature on the maxilla, and the forming dentition. As the skull matures, these three elements influence its three-dimensional development. At 5 months, the sinus appears as a triangular area medial to the infraorbital foramen.12
During the child’s first year, the maxillary sinus expands laterally underneath the infraorbital canal, which is protected by a thin bony ridge. The antrum grows apically and progressively replaces the space formerly occupied by the developing dentition. The growth in sinus height is best reflected by the relative position of the sinus floor. At 12 years of age, pneumatization extends to the plane of the lateral orbital wall, and the sinus floor is level with the floor of the nose. During later years, pneumatization spreads inferiorly as the permanent teeth erupt.
The main development of the antrum occurs as the permanent dentition erupts and pneumatization extends throughout the body of the maxilla and the maxillary process of the zygomatic bone. Extension into the alveolar process lowers the floor of the sinus about 5 mm. Anteroposteriorly, the sinus expansion corresponds to the growth of the midface and is completed only with the eruption of the third permanent molars when the young person is about 16 to 18 years of age.13 The adult sinus has a volume of approximately 15 mL (34 mm × 33 mm × 23 mm) (Figure 22-10).
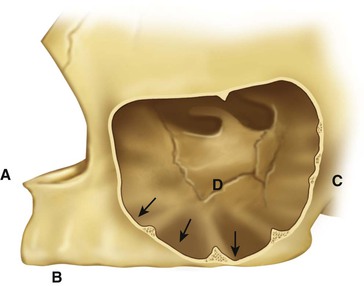
In an adult, the sinus appears as a pyramid of five bony walls, the base of which faces the lateral nasal wall and the apex of which extends toward the zygomatic bone (Figure 22-11). The floor of the maxillary sinus cavity is the opposing landmark of available bone height and reinforced by bony or membranous septa joining the medial or lateral walls with oblique or transverse buttresslike webs. They develop as a result of genetics and stress transfer within the bone over the roots of teeth. These have the appearance of reinforcement webs in a wooden boat and rarely divide the antrum into separate compartments. These elements are present from the premolar to the molar region and tend to disappear in the maxilla of the long-term edentulous patient when stresses to the bone are reduced. Karmody et al. found that the most common oblique septum is located in the superior anterior corner of the sinus or infraorbital recess (which may expand anteriorly to the nasolacrimal duct).14 The medial wall of the maxillary sinus is juxtaposed with the middle and inferior meatus of the nose.

After periodontal disease, tooth loss, and sinus expansion, frequently less than 10 mm of available bone remain between the alveolar ridge crest and the floor of the maxillary sinus, resulting in inadequate bone quantity for implant placement. A limited review of the literature reveals implants that were 9 mm or less in height may have a 16% lower survival rate compared with implants longer than 10 mm.7 Therefore, the height of bone is of primary importance for predictable implant support. This limited dimension is compounded by the decrease in bone density and the problem of the resultant medial posterior position of the ridge after resorption of bone width. As a result, failure and complications in the long term of many endosteal implant systems are reported.
High Occlusal Forces
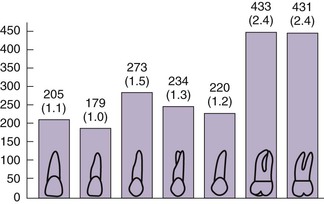
The occlusal forces in the posterior region are greater than in the anterior regions of the mouth. Studies have shown that the maximum bite force in the anterior region ranges from 35 to 50 lb/in2. The bite force in the molar region of a dentate person ranges from 200 to 250 lb/in2. As a consequence, to resist these higher bite forces, the maxillary molars of the natural teeth have 200% more surface area than even the premolars and are significantly wider in diameter (Figure 22-12). Both of these features reduce the stress to bone, which also reduces the strain of the bone during occlusal loading. Following this natural selection, implant support should be greater in the posterior molar region than any other area of the mouth.3 The decrease in bone quantity and quality and increased forces should be considered in the treatment plan of this region of the mouth.
Implant Size
Implant treatment plans should attempt to simulate the conditions found with natural teeth in the posterior maxilla. Because stresses occur primarily at the crestal region in good bone quality, biomechanical designs of implants to minimize their noxious effects should be implemented.15 Implant diameter is an effective method to increase surface area at the crestal region.16 Ideally, division B implants (narrower diameter) are not used in the posterior maxilla. Instead, implants of at least 4 mm in diameter are suggested, and 5- to 6-mm implants are encouraged in the molar region.
The length of the implant is directly related to the implant width, design, amount of the forces, and bone density. Because implant success after loading is reduced in implants 10 mm and shorter, it is logical to plan for longer implants in the region. In general, 4-mm threaded root form implants should be at least 12 mm in length when the bone density is poor (D3). This usually provides adequate BIC to dissipate the loads applied to the prosthesis. When the bone density is very poor (D4), 5-mm implants (or two implants per tooth) are suggested, also at least 12 mm in length.
Implant Number
Key Implant Number
The key implant positions for a posterior maxilla primarily relate to (1) no cantilever, (2) no three adjacent pontics, and (3) the first molar rule. The key implant positions are determined before the available bone evaluation. Hence, when the second premolar, first molar, and second molar are missing, three key implant positions are required: the first premolar and second molar (rule 1) and the first molar (rule 3).When the first premolar, second premolar, and first molar are missing, the key implant positions are the first premolar and first molar (rules 1 and 3).
A common treatment plan is to cantilever a first molar from two or more implants placed in the premolar region. As previously stated, the first molar region has twice the bite force as the premolar region. As a result, a molar with 2.4 times more surface area is placed in that location. When a cantilever replaces the molar, the highest bite force is then multiplied to the anterior implants. Uncemented restorations, screw loosening, crestal bone loss, and implant failure risk are increased (Figure 22-13). The “no cantilever” rule for fixed prostheses should especially apply to the molar regions of the mouth.
Additional Implants
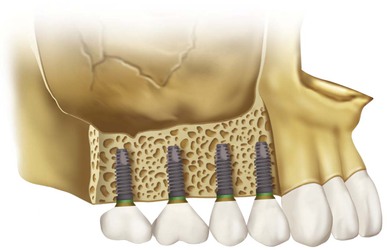
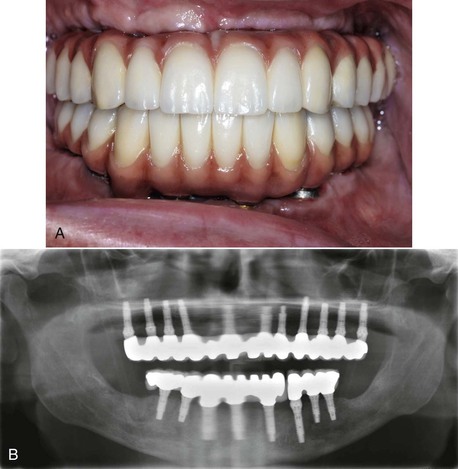
Additional implants are used when the bone density is poor or the patient force factors are large. For example, when the bone density is D4 or the patient is a bruxing male, an additional implant is required. Implant number is an excellent method to decrease crestal stresses. As a general rule in this area, one implant is often used for each missing tooth (Figure 22-14). If stress factors are magnified or the ideal implant diameter is reduced, two implants for each missing molar are suggested. Implants should always be splinted together to reduce stresses to the bone, reduce abutment screw loosening, and increase retention for the prosthesis. In general, more implants are indicated in the maxilla compared with the mandible (Figure 22-15).
Implant Design
Implant design can increase surface area of support. A threaded design implant has 30% to 200% greater surface area compared with a cylinder implant of the same size. Although more difficult to place, the threaded implant in poorer density bone is strongly encouraged. Biomechanical aspects of thread designs also affect the total increase in the surface area (i.e., thread pitch, shape, and depth).17
Roughened surface conditions or hydroxyapatite coating on the implant has been shown to increase the rate of osseous adaptation to implants and provide greater initial rigid fixation. In addition, an increase of surface-to-bone contact and amount of lamellar bone and the relatively greater strength of the coronal bone around the roughened-surface implants occur when compared with machined or smooth titanium implants.18,19 Therefore, coatings or roughened surfaces on implant bodies are suggested in the compromised D3 or D4 bone density (Figure 22-16).
Dental Contraindications for Implant Treatment
A key to the long–term success of posterior maxillary implants is the presence of adequate anterior teeth or implants. Therefore, the treatment plan should provide for the maintenance or restoration of healthy anterior teeth or division A bone in the premaxilla for implant placement. A minimum of a healthy natural canine tooth or implant abutments in the canine region for each posterior quadrant is required before posterior implants are considered.
A rule in traditional prosthetics is that a fixed prosthesis is contraindicated when the canine and two adjacent teeth are missing. Therefore, when the canine and both premolars are missing, a fixed restoration is contraindicated. A patient missing a first premolar, canine, and lateral is also contraindicated for fixed prostheses. When the patient is missing a canine, lateral, and central incisor, the patient is also contraindicated for a fixed prosthesis.
A removable prosthesis that is completely implant supported and has no movement under function is considered a fixed prosthesis for the implant support. Therefore, the rigid implant />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses