Posterior Single-Tooth Replacement
Treatment Options and Indications
Carl E. Misch
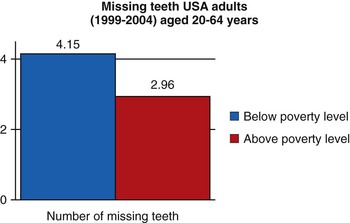
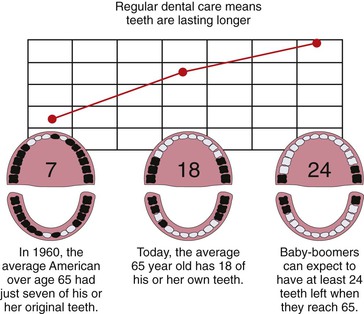
Seventy percent of the dentate population in the United States is missing at least one tooth. The average number of missing teeth above the poverty level in a U.S. survey from 1999 to 2004 was 2.96 teeth and below the poverty level was 4.15 teeth. Hence, income is not a major factor for the average tooth loss in the adult population (Figure 20-1). Single-tooth replacement will most likely comprise a larger percentage of prosthetic dentistry in the future, compared with past generations. In 1960, the average American older than age 55 years had just seven original teeth. Today the average 65-year-old adult has 18 original teeth, and baby boomers (those born between 1946 and 1964) can expect to have at least 24 original teeth when they reach 65 years of age (Figure 20-2).
The first adult teeth lost today are usually between the ages of 35 and 54 years. Almost 30% of the 50- to 59-year–old adults examined in a U.S. national survey exhibited either single or multiple posterior edentulous spaces bordered by natural teeth.1 This segment of the population has the most disposable income and is the least dependent on insurance companies to pay for dental care. Treatment to replace single teeth in the posterior regions represents nearly 7% of the annual dental care reimbursement from insurance companies and totals more than $3.2 billion each year.2,3 Because most companies often reimburse less than 50% for tooth replacement, the total costs of single-tooth replacement may approach $7 billion in the United States each year.
Posterior Missing Tooth
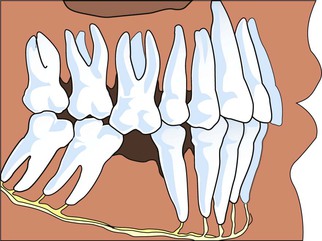
The first molars are the first permanent teeth to erupt in the mouth and often play a pivotal role in the maintenance of the arch form and proper occlusal schemes. These teeth are often the first to decay, and adult patients often have had one or more crowns fabricated to restore the integrity of the teeth and replace previous large restorations. Longevity reports of crowns have yielded very disparate results, with the mean life span at failure reported to be 10.3 years. The primary cause of failure of the crown is endodontic therapy, porcelain or tooth fracture (or both), or uncemented restoration. Teeth are at risk for extraction as a result of these complications, and coupled with decay, these complications are a leading cause of single posterior tooth loss in adults1–9 (Figure 20-3).
Posterior Single-Tooth Replacement Options
Evidence-based medicine is the conscientious, explicit, and judicious use of the best evidence in making decisions about the care of individual patients.10 Over the years, researchers have observed that external clinical evidence would both invalidate previously accepted treatment and allow replacement with new modalities that are more efficacious and safe.10 An evidence-based approach may be applied to the replacement of a posterior single tooth.
Five alternative treatment options exist for the replacement of a posterior single missing tooth (Box 20-1). The interocclusal space must be assessed carefully regardless of the treatment selected. Patients with insufficient vertical space may be contraindicated for any prosthesis without the prior correction of the occlusal plane and maxillomandibular relationships.
Removable Prosthesis
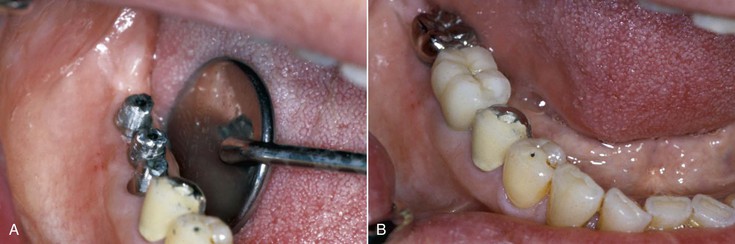
One option to replace a single missing posterior tooth is a removable partial denture (RPD) (Figure 20-4). A common axiom in restorative dentistry is to use a fixed prosthesis whenever possible.8 RPDs are usually indicated to replace spans of three or more posterior teeth or a missing canine and two or more adjacent teeth. Rarely does a patient consent to a RPD as an acceptable definitive substitute for one posterior single tooth.

The advantages of the removable restoration for multiple tooth loss include ease of daily care of the adjacent teeth, the ability to have a soft tissue replacement around the missing tooth in esthetic zones with gross defects, maxillary lip support in gross defects, minimal preparation of the abutment teeth, and reduced cost (Box 20-2). However, no reported advantages exist for a RPD replacing one posterior tooth.
Removable prostheses do not maintain bone. The maxillary posterior teeth are often in the esthetic zone (especially the maxillary premolars), and bone loss may compromise the esthetic result. Function is not improved with a removable prosthesis replacing one or two teeth. Therefore, esthetics and the fear of other teeth shifting in the arch are the two primary reasons for the patient to consent to wearing the restoration. Because of its bulk and usually the need for cross-arch stabilization, a RPD promotes more food debris and plaque accumulation on the adjacent teeth than any other treatment option (Box 20-3). Few clinical reports are available to assess the longevity survival rate, complications, or survival of adjacent teeth for a single-tooth RPD in the posterior regions of the mouth. From an evidence-based approach, this procedure is not indicated.
The plaque accumulation with the RPD increases the risk of decay and periodontal complications. Recently, Shugars et al.3 and Aquilino et al.11 have reported on survival rates of teeth adjacent to treated and untreated posterior-bounded edentulous spaces. When RPDs supported by adjacent teeth on each side were used to replace teeth, the survival rate of the posterior teeth adjacent to the edentulous space were poorer than with any other treatment option, with ranges from 17% to 44% abutment tooth loss at 4.2 to 13.5 years.3,11–14 Patients electing not to wear the RPD had greater survival of the adjacent teeth than those wearing the removable prosthesis.
In conclusion, an evidence-based evaluation for a posterior single-tooth replacement with a RPD as a definitive restoration is not indicated and may even accelerate the loss of the adjacent teeth. These devices are most often used as a transitional prosthesis in the esthetic zone.
Resin-Bonded Fixed Partial Denture
A second option to restore a single missing tooth bordered by posterior natural teeth is a resin-bonded fixed partial prosthesis. The primary advantages of this restoration are the minimal preparation of the adjacent teeth and reduced cost compared with a fixed partial denture (FPD) (Box 20-4).
Failure rates reported in the literature are greatly disparate, but the majority of reports indicate a failure rate of at least 30% within 10 years and as high as 54% within 11 months.6,15–17 It also appears that earlier perforated designs exhibited lower survival rates (Box 20-5).
The majority of resin-bonded FPD failure initially occur from cement failure (which often results in caries when partially retained), with different regions of the mouth exhibiting various retention rates. The highest survival rates occur in the maxillary anterior followed by mandibular anterior, maxillary posterior, and mandibular posterior teeth, respectively.18 Therefore, posterior tooth replacement is not as successful compared with an anterior resin-bonded restoration.
Debonding most often occurs during function, and because eating is often a social experience, this may cause the patient embarrassment and insecurity. The prosthesis may also become partially debonded and result in decay under the retainer. The selection of this option is usually driven by economics and the desire to maintain as much tooth structure as possible on the abutment teeth. This option is usually more accepted by the patient than the RPD, but it should be considered as a transitional restoration because of its high debonding rate and associated decay.
Maintenance of the Posterior Space
A third treatment option for a missing posterior tooth is to not replace the tooth but instead to maintain the missing space. A common doctrine has been to replace a missing tooth to prevent complications such as tipping, extrusion, increased plaque retention, caries, periodontal disease, and collapse of the integrity of the arch8,14 (Figure 20-5). It is speculated that these conditions cause the loss of additional teeth and have been cited as the second most common cause of missing teeth after the age of 30 years. Clinical studies evaluating the consequences of adjacent tooth loss indicate the loss of one or two teeth adjacent to a long-term edentulous space may range from 25% to less than 8% at 8 to 12 years.3,13,14 For example, Aquilino et al.11 reported an 18% 10-year tooth loss rate of adjacent teeth to a posterior missing tooth.
An indication for not replacing a single missing posterior tooth is a small intratooth space. When the space between the teeth is less than 6 mm, the adjacent teeth are often prevented from migration or extrusion from the existing occlusion. The existing occlusion often has each of the adjacent teeth with occlusal contact with two opposing teeth and as such prevents the tipping of adjacent teeth and the extrusion of the opposing teeth. This condition is most often observed with a missing mandibular second premolar when a third molar is present or after orthodontics when the first premolar was extracted. When the reduced amount of intratooth space should be closed, orthodontics or overcontoured crown(s) on adjacent teeth may correct the condition.
The location of a missing posterior tooth may influence the prosthodontic treatment plan. In general, when third molars are missing, the author suggests not replacing a second mandibular molar19 (Figure 20-6). The mandibular second molar is not in the esthetic zone of the patient. Ninety percent of the masticatory efficiency is generated anterior to the mesial half of the mandibular first molar, so function is rarely a primary reason to replace the second molar. A 10% greater occlusal force is measured on the second molar compared with the first. As a result, biomechanical stress–related complications are more of a risk, including abutment screw loosening. This tooth is more likely to exhibit working or nonworking interfaces during mandibular excursions. As a result of the increased forces and occlusal interferences, a greater incidence of porcelain fracture occurs. The crown height space (CHS) decreases as it proceeds posteriorly and represents a limited access for implant placement along with abutment screw and abutment insertion, especially when opposing natural dentition. A reduced CHS results in the abutment height being reduced, so the retention of the crown may be compromised. Cheek biting is more common in this region because of the proximity of the buccinator muscle (Box 20-6).
The course of the mandibular canal anterior to the mid first molar corresponds to the level of the mental foramen. However, in the region of the second molar, its course becomes highly variable with less available bone height and an elevated risk of paresthesia and neurovascular bundle damage during implant surgery and insertion. The bone quality in the second mandibular molar region is often inferior to other regions of the mandible, with an increased risk of bone loss or implant failure as a consequence.20 The submandibular fossa topography is deeper in the second molar regions compared with the premolar or first molar sites and mandates greater implant body angulation, with associated increased stresses at the crestal region of the implant, thereby increasing the risk of bone loss and abutment screw loosening. In addition, the facial artery is located in the submandibular fossa before it crosses the mandibular notch and crosses over the face. Perforation of the lingual plate in the region of the second molar may violate the facial artery and cause life-threatening bleeding. The mandible exhibits increased flexure and torsion in this area during opening or heavy biting on one side, and masticatory dynamics are less favorable. As a result, the implant may not integrate in a patient with moderate to severe bruxism or clenching. Finally, the cost of an implant or fixed prosthesis to replace the second molar often does not warrant the benefits achieved. As a consequence, the mandibular second molar is often not replaced when the third molar and second molar are the only posterior mandibular teeth missing.
The primary disadvantage of electing not to replace a mandibular second molar tooth is the potential extrusion and loss of the maxillary second molar or a loss of proper interproximal contact with the adjacent tooth with increased risk of caries, periodontal disease, or both. The extrusion of the maxillary second molar is usually not an esthetic or occlusal concern. When the mandible moves into an excursion, the maxillary second molar is behind the mandibular first molar and does not alter the mandibular pathway of movement even if the maxillary second molar extrudes. If extrusion of the maxillary second molar is a concern for the patient or doctor, then a crown on the mandibular first molar may include an occlusal contact with the mesial marginal ridge of the maxillary second molar, or the maxillary second molar may be bonded to the maxillary first molar.
On the other hand, a missing maxillary second molar opposing a mandibular second molar with extrusion may result in occlusal concern when the mandible moves into an excursion. The extrusion of a mandibular second molar results in an occlusal interference when the mandible moves into protrusive or lateral excursion. Hence, as a general rule, maxillary second molars are usually replaced with an implant when opposing a natural tooth (Figure 20-7).
The mandibular second molar is usually replaced when the third molar is in function and will remain present (Figure 20-8). In addition, some patients desire an intact dentition and wish to have the tooth replaced, whether or not they have a third molar (Figure 20-9). If the bone is abundant and no paresthesia or surgical risk is apparent, then the second molar may be replaced. However, this is usually the exception rather than the rule of treatment and usually replaces only a premolar-sized tooth.

The other indication to replace a mandibular second molar is when the force factors are extreme (e.g., severe parafunction) and the patient is also missing both molars. In these cases, two or three implants may be indicated to replace the missing teeth (Figure 20-10).
Fixed Partial Denture
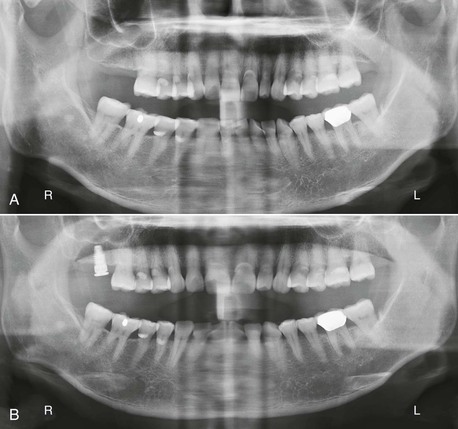
The treatment most commonly used for the replacement of a posterior single tooth is the three-unit fixed restoration (Figure 20-11). In 1990, more than 4 million FPDs were placed in the United States.21 This type of restoration can be fabricated within 1 to 2 weeks and satisfies the criteria of normal contour, comfort, function, esthetics, speech, and health. Because of these benefits, the FPD has been the treatment of choice for the past 6 decades.22,23 Few bone and soft tissue considerations exist in the missing tooth site. Every dentist is familiar with the procedure, and it is widely accepted by the profession, patients, and dental insurance companies (Box 20-7).
A three-unit FPD presents survival limitations to the restoration and to the abutment teeth.7 In an evaluation of 42 reports since 1970, Creugers et al.23 calculated a 74% survival rate for FPDs for 15 years. Walton et al.24 and Schwartz et al.25 reported mean life spans (50%) of 9.6 and 10.3 years, respectively. Scurria et al.26 performed a meta-analysis of several reports at 10 to 15 years and found 30% to 50% failure within these time frames. However, reports are very inconsistent with as little as 3% loss over 23 years to 20% loss over 3 years.4,5,23–26
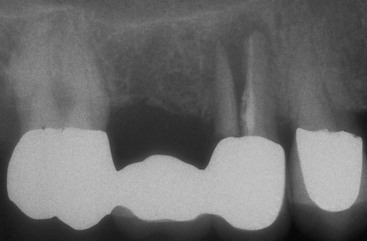
Caries and endodontic failure of the abutment teeth are the most common causes of prosthesis failure.22,24,26 Caries occurs more than 20% of the time and endodontic complications to the abutments of a FPD 15% of the time. Caries on the abutment crown primarily occurs on the margin next to the pontic (Figure 20-12). Fewer than 10% of patients floss on a regular basis, and those using a floss threader are even fewer.27 As a result, the pontic acts as a large overhang next to the crown and a reservoir for plaque. The long-term periodontal health of the abutment teeth may also be at greater risk as a result of the plaque increase, including bone loss.
When a vital tooth is prepared for a crown, a 3% to 6% risk of irreversible pulpal injury and subsequent need for endodontic treatment exists.28 Not only does tooth preparation present a risk for endodontics on each of the vital abutment teeth, but the crown margin next to the pontic is also more at risk of decay and the need for endodontics as a result. Up to 15% of abutment teeth for a fixed restoration require endodontic therapy compared with 3% to 6% of nonabutment teeth with crown preparations29 (Box 20-8).
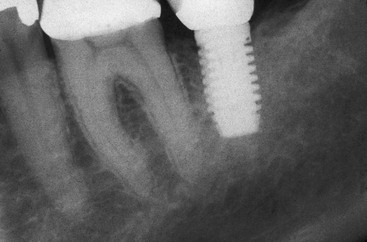
Unfavorable outcomes of FPD failure include not only the need to replace the failed prosthesis but also the loss of an abutment tooth and the need for additional pontics and abutment teeth in the replacement bridge. Root canal therapy is not guaranteed, and a meta-analysis reports a 90% success at the 8-year mark. Because 15% of FPD abutment teeth require endodontics, many abutment teeth may be lost. In addition, an endodontic posterior tooth abutment is at a greater risk of fracture. Reports indicate that abutment teeth for a FPD fail from endodontic complications (e.g., fracture) four times more often than those with vital pulps27,30,31 (Figure 20-13). The fracture of the tooth may result in failure of the prosthesis and abutment tooth.
The abutment teeth of a FPD may be lost from caries, endodontic complications, or root fracture at rates up to 30% for 8 to 14 years.3,13,14 Recent reports indicate 8% to 18% of the abutment teeth holding a FPD are lost within 10 years (Figure 20-14). This is most disturbing because 80% of abutments have no previous decay or are minimally restored before the fabrication of the FPD.6,32

Contraindications for a posterior fixed partial prosthesis primarily are related to the abutment teeth. When the abutment teeth have bone loss or short roots, the additional support required for the missing tooth with a FPD may place them at risk. A FP-3 prosthesis is more difficult to fabricate when the teeth and pontic areas have inadequate hard and soft tissue in the esthetic zone. A partial denture may be more esthetic under these conditions. On occasion, the patient does not want the natural teeth to be prepared for crowns because they are adequate in contour, health, and esthetics. The FPD cannot be fabricated without their preparation. In addition, young patients with abutment teeth that have not erupted into final position may be contraindicated for a FPD, especially when the large pulp horns in the clinical crowns are still present (Box 20-9).
Indications for a FPD include time, patient fear of surgery, adjacent tooth mobility, and unfavorable missing tooth size. A final prosthesis may be delivered within 2 weeks with a traditional FPD. An implant option most often requires several months. Rarely, is this the determining factor but on rare occasion may be significant. The patient may have a psychologic fear of implant surgery. This most often can be handled with conscious sedation. But if general anesthesia is required, a FPD may be more prudent.
When the teeth adjacent to a missing space have class II mobility and all other periodontal indexes are normal, a FPD may be the treatment of choice. A posterior space requirement for an implant option is most often greater than 6.5 mm in width and 9 mm in height. If a mandibular canal or maxillary sinus may not be modified by augmentation or the mesiodistal space is too narrow, a FPD is often the treatment of choice (see Box 20-7).
Single-Tooth Implants
The fifth treatment option to replace a posterior single missing tooth is a single-tooth implant (Figure 20-15). For years patients were advised to set their desires aside and accept the limitations of a FPD. The primary reasons for suggesting the FPD were its clinical ease and reduced treatment time. However, a RPD is faster, easier, and less expensive. If this concept of faster, easier, and cheaper was expanded, then extractions would replace endodontics, and dentures could even replace orthodontics (the teeth are straight and white). The primary reason to suggest or perform a treatment should not only be related to treatment time, cost, or difficulty to perform the procedure but also should reflect the best possible long-term solution for each individual.
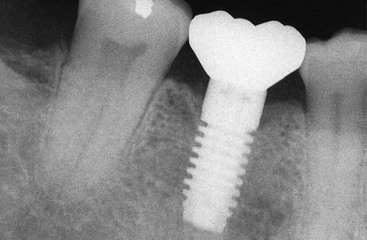
Before 1990, few long-term studies focusing on single-tooth implant replacement with osseointegrated implants in any region of the mouth had been published. Early reports indicated that single-tooth implant results were less predictable than they have become in the past 10 years. For example, in 1990, Jemt et al.33 reported a 9% implant failure within 3 years of prosthesis completion on 23 implants (21 in the maxilla, two in the mandible). In 1992, Andersson et al.34 published a preliminary report of a prospective study of 37 implants resto/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses