Chapter 20
Multi-disciplinary orthodontics
Orthodontic treatment is often part of a multi-disciplinary team approach for dental patients.
These patients fall into three main categories of combined need:
- Restorative
- Surgical
- Cleft
Some patients, for example patients with a cleft condition, may require treatment from all three categories.
RESTORATIVE
Some simple cases are multi-disciplinary between the general dental practitioner (GDP) and the orthodontist but more severe cases are seen at an orthodontic/restorative multi-disciplinary clinic for full assessment.
Microdontia
These patients sometimes have conical or ‘spiky’ teeth. The most common tooth affected is the upper lateral incisor. These teeth are sometimes referred to as peg-shaped. These irregularly shaped teeth have to be built up either with facings, veneers or crowns. Sometimes, several teeth are affected.
Hypodontia
These patients do not have all the teeth needed to make up the full dentition. They rarely have both the deciduous (baby) and permanent tooth missing. If this is just a single tooth, it may be possible to close the space orthodontically. If the span is too wide, then it is necessary to have some type of replacement.
This could be:
- adenture
- abridge
- an implant
Some patients with hypodontia have several missing teeth, even three or more per quadrant. Sometimes, hypodontia and microdontia are found in the same patient. Orthodontic treatment can be invaluable in correcting the existing permanent teeth into position to facilitate the restoration of spaces left by the absence of a number of teeth.
SURGICAL
Some patients are born with:
- A facial deformity
- skeletal pattern imbalance
- problems with condyles
- un favourable growth (especially in the mandible)
These may require corrective jaw surgery.
It may also be necessary to have surgery on:
- ectopic teeth which need surgical uncovering and exposure
- teeth which need transplanting to a more favourable position
- a thick, fleshy frenum
- supernumerary, submerged or impacted teeth
A frequent interface between the orthodontist and the maxillo-facial surgical team comes when the patient requires an osteotomy. This is a procedure to correct a skeletal discrepancy of mandible/maxilla. Patients are seen on a combined clinic. At these clinics, the patients are also given information leaflets (Figure 20.1).
Most osteotomies are carried out inside the mouth. Sometimes, bone is harvested from another site, often from the hip (the iliac crest) for use in the procedure.
These are carried out after the patient has finished most of their growth. In the case of the face, this is later for boys than girls.
They can be:
- maxillary
- mandibular
- both (known as bimaxillary)
Figure 20.1 Leaflet for orthognathic surgery. (Reproduced with the kind permission of the British Orthodontic Society.)
The maxillary (mid face) osteotomies include:
- Le Fort I (involving the tooth-bearing maxilla)
- Le Fort II (involving the maxilla and the nose)
- Le Fort III (involving the maxilla, nose and cheeks)
The mandibular (lower face) osteotomies include:
- sagittal split (centred at the angles and ascending ramus of the mandible)
- genioplasty (when the tip of the chin is repositioned)
For many patients, these operations will alter their appearance. This is one of the reasons the patient may be offered an appointment with a clinical psychologist at this stage.
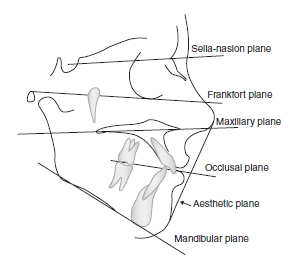
Figure 20.2 Drawing showing Frankfort plane.
For these patients, the orthodontist and maxillo-facial surgeon need to see patients together to formulate a treatment plan.
As part of this, the orthodontist will take radiographs, including a lateral and, occasionally, a postero-anterior (PA) cephalogram on which to reproduce a tracing.
There are many reference points on a tracing.
Skeletal measurements can be recorded:
- horizontally, vertically, antero-posterior (front to back)
- transverse, across width (less commonly used)
For the purposes of a basic guide, it would be useful as a baseline to see the:
- Frankfort plane (Figure 20.2) – as the horizontal measurement
- maxillary plane – as a line from the posterior border to the anteriorpoint of the hard palate
- occlusal plane – as a line between the teeth in occlusion
- mandibular plane – as the lower border of the mandible
- aesthetic plane – as a line along the soft tissue profile from the tip of the nose to the tip of the chin
Tracing can be done either:
- manually
or
- using computer software
In order to make a manual tracing, the operator will need:
- tracing film (usually 8 × 10)
- atooth-tracingtemplate
- triangle
- cephalometric protractor and template (joined)
- metric scale rule
- yellow graph pencil
- a light box
When using the manual method the clinician will:
- manually place the lateral cephalometric (side view of the head) radiograph on the light box (with the nose facing to the right)
- place the tracing paper over this
- then using a series of recognised hard tissue coordinate points, trace lines between these points and measure the relevant angles
- using a tooth template, protractor and pencil, then produce a tracing which will accurately show the pre-surgical measurements of the patient and this helps form the proposed orthodontic and surgical planning
NB: Soft tissue profiles are not so predictable but as a guide, follow the bone changes by 50%.
When using a computer, the operator needs to trace the reference points which are plotted by the software program. This calculates the angles and measurements, which, when printed out are shown together with line tracings.
In addition, the laboratory technician:
- may also be asked to make a Kesling set-up
- This is done by taking a set of work models, cutting off and ‘resetting’ the teeth in their projected position
Orthodontic treatment will then be planned and carried out/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


