Q. 2. Classify white lesions of the oral cavity. Describe the aetiology, clinical features and management of leukoplakia.
Or
Name some of the white lesions of oral mucosa. Describe the clinical features, differential diagnosis and treatment of leukoplakia of hard palate.
Or
What are the keratinizing lesions of the oral cavity? Write about oral leukoplakia.
Or
Define leukoplakia. Discuss the aetiopathogenesis, clinical features and treatment of oral leukoplakia.
Or
Enumerate the ‘white lesions’ of the oral cavity. Describe leukoplakia in detail, giving differential diagnosis.
Ans.
Classification of white lesions
I. Variations in structure and appearance of the normal oral mucosa
II. Nonkeratotic white lesions
ii. Burns (thermal, aspirin, dental medicaments, radiation mucositis and uraemic stomatitis)
iii. Caused by specific infectious agents (Koplik spots, syphilitic patches)
i. Acute pseudomembranous candidiasis (oral thrush)
ii. Acute atrophic candidiasis (antibiotic sore mouth)
iii. Chronic atrophic candidiasis (denture sore mouth and angular cheilitis)
IV. Keratotic white lesions with no increased potential for the development of oral cancer
iv. Focal epithelial hyperplasia
v. Psoriasiform lesions (psoriasis, Reiter syndrome, geographic tongue ‘ectopic geographic tongue’)
V. Red and white lesions with defined or uncertain precancerous potential
i. Leukoplakia (homogenous, nodular or speckled and verrucous)
iii. Oral lesions are with use of tobacco and alcohol (cigarette, cigar, and pipe smoking, snuff clipping tobacco and betel nut chewing, reverse smoking)
viii. Discoid lupus erythematosus
xi. Oral lichenoid reactions (erythema multiforme, lupus erythematosus, dermatomyositis, drug-induced lichenoid reactions, secondary syphilis and graft vs. host reactions).
This grouping provides a practical scheme for the clinician faced with for making decisions about particular lesions.
Leukoplakia
Aetiologic factors
Classification
Clinical types of leukoplakia are as follows:
Histological types
Leukoplakia is mainly categorized into two types:
i. Those that show no atypia (dysplasia).
ii. Those that show different degrees of atypia.
• A leukoplakia lesion may show severe atypia with malignant change throughout the depth of epithelial layer, but its basement membrane may still be intact, such lesion is referred to as carcinoma in situ or intraepithelial carcinoma. When intraepithelial carcinoma breaks through the basement membrane, it becomes an invasive SCC.
Leukoplakia is also divided into two types according to its spontaneous disappearance following removal of chronic irritant as follows:
Clinical features
i. Asymptomatic, discovered during routine oral examination.
ii. More common in older age group >35 years (40–70 years) of age range, more common in men.
iii. Frequent sites are lips, vermilion border, buccal mucosa, mandibular gingiva, tongue, oral floor, hard palate, maxillary gingiva, lip mucosa and soft palate. The floor of the mouth and lateral border of tongue are high rick sites for malignant transformation.
iv. Lesions may greatly vary in size, shape and distribution, the borders may be distinct or indistinct smoothly contoured or ragged.
v. The typical homogenous leukoplakia is characterized as white, well-demarcated plaque with an identical reaction pattern throughout the lesion.
vi. The surface texture can vary from smooth thin surface to leathery appearance with surface fissures referred to as ‘cracked mud’.
vii. The nonhomogeneous type of oral leukoplakia also known as erythroleukoplakia or speckled leukoplakia may have white patches or plaque intermixed red tissue elements.
viii. Verrucous or verruciform leukoplakias are the lesions in which white component is dominated by papillary projections similar to oral papillomas.
This variety of leukoplakia with more aggressive proliferation pattern and recurrent rate are designated as proliferative verrucous leukoplakia (PVL). This is more common in older women and lower gingiva is the predilection site.
ix. Malignant potential: Those lesions situated in the high-risk areas, such as floor of the mouth, ventral surface of tongue, margins of the tongue and retro molar regions have high risk for malignant transformation.
Differential diagnosis
Management
I. Elimination of aetiological factors
• No appropriate treatment has been established for Sanguinaria-induced leukoplakia. So, complete discontinuation of Sanguinaria containing products is mandatory and cessation of any other harmful habits like alcohol and smoking by the Patients which are well established risk factors.
• Vitamin therapy especially vitamin A and vitamin E, B complex, 13- cis-retinoic acid, antioxidant therapy.
• Cold knife surgical excision.
• Cryosurgery (liquid nitrogen or CO2 snow is used).
• Fulguration (electro-cautery or electro-surgery).
• Laser (light amplification by especially CO2 lasers Stimulated fusion of radiation).
• However, in the absence of evidence-based treatment, strategies for oral leukoplakias, surgery will remain the treatment of choice for leukoplakia and erythroplakia.
• A general recommendation may be to re-examine the site every 3 months for first 1 year irrespective of surgical excision.
• Follow up every 6 months to see whether there is any change in reaction pattern and relapse.
• Self-examination is reasonable approach if there is no relapse for 5 years.
• However, an initial biopsy is mandatory. If a histopathologic diagnosis of dysplasia is rendered, the condition should be treated in a fashion similar to the treatment of other potentially premalignant processes.
• All patients should be given careful clinical follow-up, with a biopsy of any recurrent or worsening lesion(s).
Q. 3. Enumerate oral precancerous lesions and conditions. Describe clinical features and management of oral submucous fibrosis.
Or
What conditions may produce trismus? Describe in detail the predisposing factors, clinical features, treatment of oral submucous fibrosis.
Or
Write the clinical features, differential diagnosis and management of oral submucous fibrosis.
Or
Describe in detail aetiology, clinical features and management of oral submucous fibrosis.
Or
Describe in detail the aetiology, clinical features, treatment plan and prognosis of submucous fibrosis.
Ans.
• The premalignant lesions are defined as morphologically altered tissue in which cancer is more likely to occur than in its apparently normal counterpart.
• The premalignant condition is defined as generalized state of body, which is associated with significantly increased risk of cancer.
For example, oral submucous fibrosis, syphilis, lichen planus, white sponge nevus, etc.
The following are the conditions that produce trismus:
Oral submucous fibrosis
Aetiology and pathogenesis
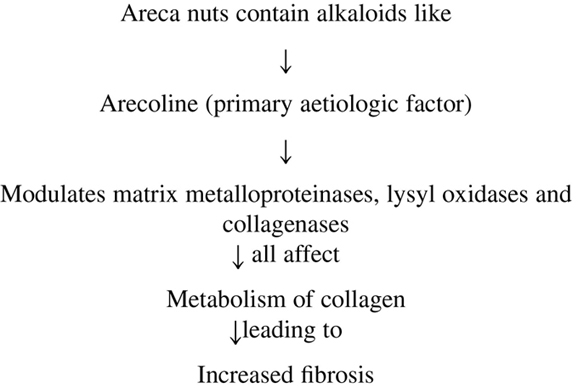
a. Betel nut, i.e., areca nuts (alkaloids)
b. Chillies capsaicin (active ingredient causing irritation)
• Areca nut, quid chewing habit and development of OSMF is dose dependant and the mechanism is described below:
• Vitamin B complex deficiency.
• Deficiency is precipitated by the defective nutrition due to impaired food intake.
For example, streptococcal toxicity.
• Klebsiella rhinoscleromatis may be causative factors in OSMF.
Clinical features
i. Age and sex: Equally affects both the sexes and patients are between second and fourth decade.
ii. Site: Most frequent locations are buccal mucosa (98%) and retromolar areas. Commonly involved sites are: soft palate, (49%) palatal fauces, uvula, tongue and labial mucosa.
iii. Prodromal symptoms: Onset of OSMF is insidious and is often 2- to 5-year duration. Most common initial symptom is burning sensation of oral mucosa, aggravated by spicy food followed by either hypersalivation or dryness of mouth.
iv. The first sign is erythematous lesions, sometimes in association with petechiae, pigmentations and vesicles.
v. Initial lesions are followed by paler mucosa, which comprise white marbling.
vi. In the later course of the disease, the most prominent clinical features appear, i.e. fibrotic bands located beneath an atrophic epithelium.
vii. ↑fibrosis leads to loss of resilience, which causes interference with speech, tongue mobility and a decreased ability to open the mouth.
viii. The atrophic epithelium may cause a smarting sensation and inability to eat hot and spicy food.
ix. Diagnosis of OSMF is based on clinical features and patients report of a habit of betel quid chewing.
An international consensus has been reached where at least one of the following characteristics should be present to diagnose OSMF, they are as follows:
Pathology
Early histopathological characteristics of OSMF are:
• Fine fibrils of collagen, oedema, hypertrophic fibroblasts, dilated and congested blood vessels and infiltration of neutrophilic and eosinophilic granulocytes.
• Down regulation of fibroblasts, epithelial atrophy and loss of rete pegs and early signs of hyalinization in concert with an infiltration of inflammatory cells.
Malignant transformation of OSMF has been estimated in the range of 7–13% and incidence over 10-year period is 8%.
Management
i. Stopping of chewing habits, especially areca nut as it is carcinogenic. If this is successfully implemented. Early lesions have a good prognosis as they may regress.
• Iodine, B-complex preparations (e.g., injection ranodine) Injection of arrsenotyphoid and iodine (arrsenotyphoid is a fibrin dissolving agent).
| Both | Topical—e.g., hydrocortisone injection along with procaine HCl intralesionally every fortnight. |
| Systemic—e.g., cortisone, hydrocortisone 25 mg tab in doses of 100 mg/day. Triamcinolone or 90 mg dexamethasone. |
• Increased vascularity at the affected site attributed to fibrolytic, antiallergic and anti-inflammatory action of corticosteroid.
• The fibrosis is prevented by decreasing fibroblastic production and deposition of collagen.
• It is an essential biogenic stimulator. Only the aqueous extract of placenta acts as biogenic stimulator. It accelerates cellular metabolism, stimulated regenerative process, aids in absorption of exudates, increases physiologic function of organs and significant enhancement of wound healing and it has notable anti-inflammatory effect. Dose—Intralesionally 2 mL of solution is deposited in five divided regions of the lesions at intervals of 3 days or about 15 days. If required the course is repeated after a month.
v. Hyaluronidase: It acts by breaking down the hyaluronic acid, i.e., the ground substance of connective tissues.
vi. Surgical procedures: When there is marked limitation of opening the surgery is the treatment method of choice.
a. Excision of fibrous bands followed by use of tongue flap as a graft or bilateral full thickness nasolabial flap.
b. New technique of bilateral palatal flaps to cover exposed area in combination with the bilateral temporalis myotomy and coronoidectomy.
c. LASER—with CO2 laser under GA incise the buccal mucosa and vaporize the submucosal connective tissue to the level of buccinator muscle.
d. Cryosurgery—local destruction of tissue by freezing it in sites.
vii. Oral physiotherapy: oral exercises are advised in early and moderately advanced cases.
viii. Diathermy: Microwave diathermy is useful in early and moderate lesions like mouth opening and ballooning of mouth.
Q. 4. Write an essay on oral candidiasis.
Or
Classify oral mucosal candidiasis. Write the aetiopathogenesis, clinical features, investigations and management of chronic atrophic candidiasis.
Or
Enumerate the various white lesions that can be scrapped. Describe the clinical features, differential diagnosis and treatment of candidiasis.
Or
Enumerate predisposing factors of candidiasis. Mention the various types and discuss in detail the treatment plan.
Or
Classify candidiasis. Write in detail about the aetiology, clinical features and management of oral thrush.
Or
Classify candidiasis and give clinical features, laboratory diagnosis tests and treatment of oral candidal infection.
Or
Treatment of acute pseudomembranous moniliasis.
Ans. Oral candidiasis is the most prevalent opportunistic infection affecting oral mucosa.
Most candida infections only affect mucosal linings, but the rare systemic manifestations may have fatal course.
Aetiology and pathogenesis
Predisposing factors to oral candidiasis
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses