Generic Root Form Component Terminology
Carl E. Misch
An endosteal implant is an alloplastic material surgically inserted into a residual bony ridge, primarily as a prosthodontic foundation.1 The prefix endo means “within,” and osteal means “bone.”2 The major subcategory of endosteal implants covered in this text are root form implants. The term endosseous is also used in the literature, and because the term osseous also indicates bone, either term is acceptable. However, endosteal, periosteal, and transosteal are preferred. Many endosteal implant designs have been used in the past, including tapered pegs, pin shapes, and plate forms.3,4 Today an endosteal implant in the shape of a single rooted tooth is the design most often used in the restoration of partial or complete edentulous patients.
Implant dentistry is the second oldest discipline in dentistry (oral surgery [exodontia] is the oldest). Root form implant history dates back thousands of years and included ancient civilizations. For example, 4000 years ago the Chinese carved bamboo sticks in the shape of pegs and drove them into the bone for fixed tooth replacement. The Egyptians used precious metals with a similar peg design 2000 years ago. A skull was found in Europe with a ferrous metal tooth inserted into a skull with a tooth peg design that dated back to the time of Christ. Incas from Central America around 600 ad took pieces of sea shells and, similar to the ancient Chinese, tapped them into the bone to replace missing teeth5 (Figure 2-1). In other words, history demonstrates it has always made sense to replace a tooth with an implant, with the approximate shape of a tooth. In reality, if the lay public were given a choice to replace a missing tooth with an implant or to grind down several adjacent teeth and connect them with a prosthesis to replace a missing tooth and then attempt to make the adjacent teeth look similar to the condition before their preparation, the implant would be the obvious choice.
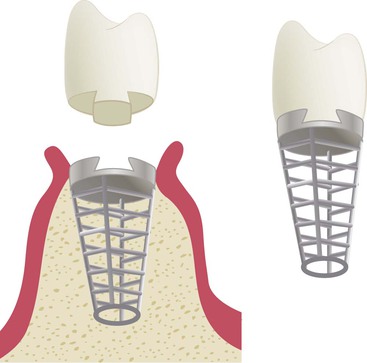
Maggiolo introduced the more recent history of implant dentistry in 1809 with use of gold in the shape of a tooth root.6 In 1887, Harris reported the use of teeth made of porcelain into which lead-coated platinum posts were fitted.7 Many materials were tested, and in the early 1900s, Lambotte fabricated implants of aluminum, silver, brass, red copper, magnesium, gold, and soft steel plated with gold and nickel.8 He identified the corrosion of several of these metals in body tissues related to electrolytic action. The first root form design that differed significantly from the shape of a tooth root was the Greenfield latticed-cage design in 1909, made of iridoplatinum9 (Figure 2-2). This was also the first two-piece implant, which separated the abutment from the endosteal implant body at the initial placement. The surgery was designed to use a calibrated trephine bur to maintain an inner core of bone within the implant body. The implant crown was connected to the implant body with an antirotational internal attachment after several weeks. Reports indicate this implant had a modicum of success. Seventy-five years later, this implant design was reintroduced by Straumann in Europe and later by Core-Vent in the United States.10,11
Surgical cobalt-chromium-molybdenum alloy was introduced to oral implantology in 1938 by Strock (Boston, MA) when he replaced a single maxillary left incisor tooth12 with a root form, one-piece implant that lasted more than 15 years. A direct bone–implant interface to titanium was initially called bone fusing and was first reported in 1940 by Bothe and coworkers.13 In 1946, Strock designed the first titanium, two-piece screw implant that was initially inserted without the permucosal post (Figure 2-3). The abutment post and individual crown were added after complete healing.14 The desired implant interface described by Strock was a direct bone–implant connection, which was called ankylosis. The first submerged implant placed by Strock was still functioning 40 years later.15
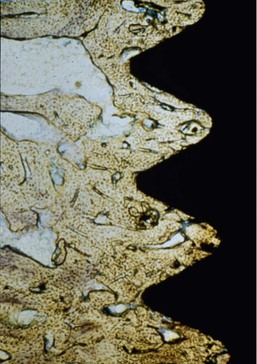
Brånemark began extensive experimental studies in 1952 on the microscopic circulation of bone marrow healing. These studies led to a dental implant application in the early 1960s in which a 10-year implant integration was established in dogs without significant adverse reactions to hard or soft tissues. Implant clinical studies in humans with the Brånemark philosophy began in 1965, were followed for 10 years, and were reported in 1977.16 The term osseointegration (rather than bone fusing or ankylosis) was defined by Brånemark as a direct contact of living bone with the surface of an implant at the light microscopic level of magnification17 (Figure 2-4). The terms bone fusing, ankylosis, and osseointegration may be interchangeable and may address the microscopic bone–implant interface. The percentage of direct bone–implant contact was not initially addressed and has been found to be highly variable.
Rigid fixation is the clinical result of a direct bone interface but has also been reported with a fibrous tissue interface.18 Rigid fixation is a clinical term that implies no observable movement of the implant when a force of 1 to 500 g is applied. Today the term osseointegration has become common in the implant discipline and describes not only a microscopic condition but also the clinical condition of rigid fixation. The prefix osteo (e.g., osteoblast, osteotomy) also is widely used by the profession and may describe this condition as osteointegration.
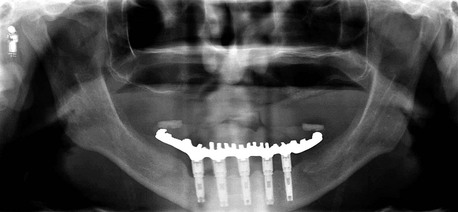
The osseointegration concepts of Brånemark have been promoted more than those of any other previous person in dental history. The documentation of past clinical case studies, research of surgery and bone physiology, healing of soft and hard tissues, and restorative applications from Brånemark’s laboratory were unprecedented. Adell et al. published the Brånemark 15-year clinical case series report in 1981 on the use of implants in completely edentulous jaws.17 Approximately 90% of the reported anterior mandibular implants that were in the mouths of patients after the first year of loading were still in function 5 to 12 years later. Lower survival rates were observed in the anterior maxilla. In the initial Brånemark clinical reports, no implants were inserted into partially edentulous patients or the posterior regions of the mouth of edentulous patients, and all reported prostheses were cantilevered fixed restorations (Figure 2-5).
The use of dental implants in the treatment of complete and partial edentulism has become an integral treatment modality in restorative dentistry.19–21 The 1988 National Institutes of Health consensus panel on dental implants recognized that restorative procedures using implants differ from those of traditional dentistry and stressed the necessity for advanced education.22 During the past 15 years, implant dentistry has become a routine method to replace teeth in a restorative practice.
Many practitioners are taught the use of a specific manufacturer’s implant system rather than the theory and comprehensive practice of implant dentistry. The increasing number of manufacturers entering the field use trade names for their implant components (often unique to a particular system), and such names have proliferated to the point of creating confusion. Several different terms or abbreviations now exist that describe similar basic components.23–28
To make conditions worse, in the team approach to implant treatment, the widening referral base often requires that the restoring practitioner be knowledgeable regarding many implant systems. With the required knowledge of multiple systems and the lack of uniformity in component names, communication is hampered among manufacturers, dentists, staff, laboratory technicians, students, and researchers. In addition, the incorporation of implant dentistry into the curriculum of most predoctoral and postdoctoral programs further emphasizes the need for standardization of terms and components in implant dentistry.29
Generic Prosthetic Component Terminology
A generic language for endosteal implants was developed by Misch and Misch in 1992.30 The order in which these terms is presented follows the chronology of insertion to restoration. In formulating the terminology, five commonly used implant systems in the United States were referenced. Fifteen years later, the dramatic evolution of the U.S. implant market has resulted in changes in nearly all the implant lines and component designs.31–33 In 2000, the U.S. market alone had to choose from more than 1300 different implant designs and 1500 abutments in various materials, shapes, sizes, diameters, lengths, surfaces, and connections. More than ever, a common language is needed. In pharmacology, the variety of pharmaceutical components makes it impossible to list them all by proprietary names, but a list by category of drugs is useful. Likewise, implant components still can be classified into broad application categories, and practitioners should be able to recognize a certain component category and know its indications and limitations.
This book incorporates a generic terminology, first introduced by Misch and Misch for endosteal implants, that blends a continuity and familiarity of many implant systems with established definitions from the terms of the Illustrated Dictionary of Dentistry and the glossaries from Terms of the Academy of Prosthodontics, American Academy of Implant Dentistry, and International Congress of Oral Implantologists.1,2,34,35
Generic Implant Body Terminology
Root form implants are a category of endosteal implants designed to use a vertical column of bone, similar to the root of a natural tooth. Although many names have been applied, the 1988 National Institutes of Health consensus statement on dental implants and the American Academy of Implant Dentistry recognized the term root form.1,22,35
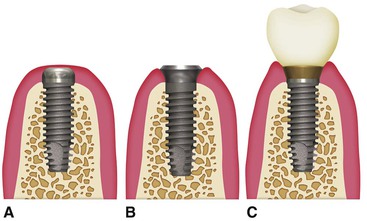
The most common root form design has a separate abutment and implant body, which permits only the implant body placement during bone healing (Figure 2-6). A second procedure is required to attach the implant abutment. The design and surgical philosophy is to achieve clinical rigid fixation that corresponds to a microscopic direct bone-to-implant interface without intervening fibrous tissue occurring over any significant portion of the implant body after healing.
Over the years, three different surgical approaches have been used for the two-piece implant systems: one stage, two stage, and immediate restoration (loading) (Figure 2-7). The two-stage surgical process places the implant body below the soft tissue until the initial bone healing has occurred. During a second-stage surgery, the soft tissues are reflected to attach a permucosal element or abutment. During a one-stage surgical approach, the implant body and the permucosal element above the soft tissue are both placed until initial bone maturation has occurred. The abutment of the implant then replaces the permucosal element without the need for a secondary soft tissue surgery. The immediate restoration approach places the implant body and the prosthetic abutment at the initial surgery. A restoration (most often transitional) is then attached to the abutment (often out of occlusal contacts in partially edentulous patients) within 2 weeks of the surgical appointment.
An implant body especially designed for one surgical method may also be selected. For example, a permucosal element may already be attached to the implant body by the manufacturer to facilitate a one-stage surgical approach. An implant body also may have a prosthetic abutment, which may be part of the implant body, for the one-piece implant to be inserted and restored at the initial surgery. The latter was the original concept first introduced.12
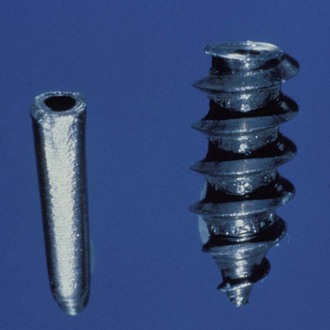
There are three primary types of root form body endosteal implants based on design: cylinder, screw, or combination30 (Figure 2-8). Cylinder root form implants depend on a coating or surface condition to provide microscopic retention to the bone. Most often the surface is either coated with a rough material (e.g., hydroxyapatite, titanium plasma spray) or a macro retentive design (e.g., sintered balls). Cylinder implants are usually pushed or tapped into a prepared bone site. They can be a paralleled wall cylinder or a tapered implant design. Screw root forms are threaded into a slightly smaller prepared bone site and have the macroscopic retentive elements of a thread for initial bone fixation. They may be machined, textured, or coated. There are three basic screw-thread geometries: V-thread, buttress (or reverse buttress) thread, and power (square) thread designs.36 Threaded implants are primarily available in a parallel cylinder or tapered design. Micro or macro thread features; variable thread pitch, depth, and angle; and self-tapping features can be combined to create a myriad of implant designs in this category. The threaded implants may also have a microscopic connection to the bone as a result of its surface condition. Combination root forms have macroscopic features from both the cylinder and screw root forms. The combination root form designs also may benefit from microscopic retention to bone through varied surface treatments (machined, textured, and the addition of coatings).37–45 As a general rule, the combination implant designs have a press-fit surgical approach (as the cylinder implants) and a macroscopic implant design for occlusal loads (as a series of plateaus or holes in the body). Root forms also have been described by their means of insertion, healing, surgical requirements, surface characteristics, and interface.28,46
Implant Body Regions
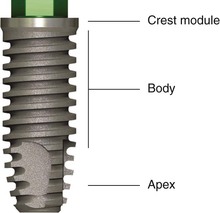
The implant body may be divided into a crest module (cervical geometry), a body, and an apex (Figure 2-9). Each section of an implant body has features that are of benefit in the surgical or prosthetic application of the implant.
Implant Body
An implant body is primarily designed for either surgical ease or prosthetic loading to the implant–bone interface. Years ago, the implant body was the primary design feature. A round implant permits round surgical drills to prepare the bone. A smooth-walled cylinder or combination implant allows the implant to be pressed or tapped into position, similar to a nail into a piece of wood. A tapered cylinder fits into the top section of the osteotomy before engagement of the bone for further ease of placement.
A cylinder or press-fit implant design system offers the advantage of ease of placement even in difficult access locations. The cover screw of the implant also may be attached to the implant before implant placement. For example, in the very soft D4 bone of the posterior regions of the maxilla, the surgeon must rotate a threaded implant design into place. Very soft bone may strip during a threaded implant insertion. This may result in lack of initial fixation, and the implant will not be rigid. A tapered cylinde/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses