Chapter 18
Endodontic decision making
The outcome of endodontic treatment
Evaluation of the outcome of endodontic therapy has a long tradition and numerous investigations based on radiographic examination have been published. Strindberg published a study with great impact on subsequent research in 1956 (68). He launched a system of criteria based on the absence or presence of radiographic rarefactions around the apex of the evaluated root. Basically, Strindberg held that a periapical radiolucency diagnosed at the end of a predetermined healing period should be considered a sign of biological treatment “ failure”. Although Strindberg found that complete periapical healing sometimes did not occur until 10 years after treatment, he recommended a 4-year follow-up period as a cut-off before a final classification be made. The system provided a simple distinction between healthy and diseased roots and has been widely used ever since as a tool to assess the general outcome of endodontic treatment but also to investigate the factors that might influence postoperative healing (Fig. 18.1).
A more detailed system for radiographic diagnosis of the periapical tissues was launched by Ørstavik et al. in 1986 (47). Based on a study by Brynolf (11) in which the histological and radiographic pictures of periapical biopsy specimens were compared, a five-level score was constructed. The score is intended to represent a disease progression from normal periapical structures (score 1) to severe apical periodontitis with exacerbating features (score 5). In recent years the so-called periapical index (PAI) has often been used as an alternative to the Strindberg type of classification.
Investigations assessing the outcome of endodontic therapy often are designed as so-called follow-up studies. In these studies a cohort of patients is treated and followed clinically and radiographically for a certain period of time. Ideally such studies should be made prospectively and factors of interest randomized, but for ethical and practical reasons a retrospective (looking back in files and records) non-randomized approach has more often been used. However, this scientific strategy might bias the data produced and limit the confidence in conclusions made.
A substantial body of data has been collected from follow-up studies through the years. The accumulation of knowledge is impeded by the large variation among the investigations concerning factors such as case selection, sample size, treatment procedures, recall rate, length of observation period and radiographic interpretation. Regardless of the limitations, the studies clearly demonstrate that endodontic treatment can be a highly successful procedure. When teeth without apical periodontitis (irrespective of the pulp being vital or necrotic) are treated lege artis, a successful outcome might be expected in as many as 95% of cases. When treatment “fails”, i.e. periapical inflammation develops, it is most often caused by microorganisms contaminating the root canal during treatment or postoperatively via defective margins of fillings and crowns.
Compared with vital pulp cases, teeth with necrotic pulp and apical periodontitis are associated with less probability of treatment success. In such cases microorganisms are present initially that, owing to the complexity of the root canal system, may not invariably be combated successfully. However, thorough cleaning, medication and obturation of the canal will produce periapical healing in 80–85% of cases.
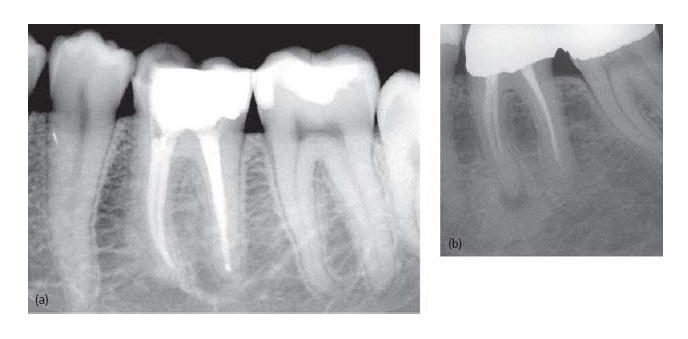
Fig. 18.1 Evaluation of treatment outcome according to Strindberg (68). (a) A 4-year follow-up of a first lower molar. The patient has no clinical symptoms and no signs of pathology are visible in the radiograph. The case is classified as a “success”. (b) This tooth was treated 5 years ago for apical periodontitis. The periapical lesion has decreased but is still visible on the radiograph. The case is classified as a “failure”.
Factors influencing treatment outcome
Although endodontic treatment is usually successful, some cases will fail and it is the responsibility of the individual clinician to minimize this number. Therefore, knowledge of the various factors that will influence treatment outcome is of supreme importance. Such “prognostic” factors might be found in the situation that precedes endodontic treatment (preoperative factors) or might be associated with the treatment per se (operative factors). Also, elements of the postoperative situation might exert influence on the long-term outcome (Core concept 18.1, Key literature 18.1).
Preoperative factors
In most studies general factors such as age, gender and health have not been demonstrated to influence the treatment outcome significantly. When local factors have been considered some investigators reported that certain teeth appeared to be more favorable than others, but a systematic pattern among the studies and teeth has not been found. The only preoperative factor that consistently has proven to influence significantly the treatment result is the diagnosis of apical periodontitis. Studies have reported a 10-25% lower healing rate when radiographic signs of periapical disease are present compared with when they are not.
Operative factors
The apical extent of the root canal preparation is one of the major prognostic factors. The instrumentation ideally should be terminated at the constriction of the canal, which is normally located 1–2 mm from the root apex. Sjögren et al. (65) reported periapical health to be restored in 94% of teeth with apical periodontitis when the preparation and root filling ended within 0–2 mm of the radiographic apex. On the other hand, when preparations were made to a shorter distance from the apex, only 68% healed.
- Apical periodontitis
- Extent of canal preparation
- Quality of seal
- Procedural error
- Coronal leakage
- Post preparation
Over-instrumentation of the root canal should be avoided. When the instrument passes through the apical foramen it may induce displacement of infected dentin into the periapical tissues. Attached to dentin chips, microorganisms are protected from the defense mechanisms of the host and may therefore survive and impair the potential for healing (76). More importantly, repeated overinstrumentation may enlarge the apical foramen and alter its original anatomy. Consequently, the root canal preparation will lose its apical resistance form, which will often result in overfill combined with an inadequate apical seal of the canal (Fig. 18.2).
Overfill of the root canal has been found to be associated with a decreased healing rate in teeth with apical periodontitis. The sustained lesion is probably caused not so much by the material itself (gutta-percha is well tolerated by the tissues) but more by intracanal microbes. Numerous outcome studies have proven the significance of the quality of the root filling seal. An inadequate apical seal will allow tissue fluids to leak into the root canal and supply microorganisms with substrate, and also let bacterial products seep out into the periapical tissues. On the other hand, a defective coronal seal might provide the oral microorganisms with an avenue for a postoperative infection of the root canal, resulting in “late” or sustained periapical inflammation.
Fig. 18.2 The negative influence of overinstrumentation. A repeated instrumentation through the apical foramen will result in a “tear-drop” anatomy and hinder a good-quality root filling seal.

If negative prognostic factors accumulate, the chance of success will decrease substantially (19). For example, if an apical periodontitis case is overinstrumented and provided with a defective seal, the probability of healing will be low. In an epidemiological study Bergenholtz et al. (8) found that 55% of overfilled roots with defective seals were associated with periapical radiolucency. On the other hand, when root fillings ended within 2 mm of the apex and were assessed as adequate, only 12% demonstrated periapical radiolucency.
Procedural errors such as perforations, broken instruments and ledge formations will not directly impede periapical healing. However, the prognosis of the treatment is decreased if the complication obstructs the cleaning of an infected canal.
Postoperative factors
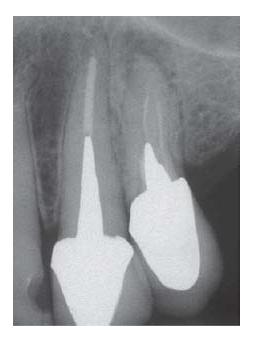
Data from recent studies indicate that the quality of the restoration of the tooth might exert an influence on the outcome of endodontic treatments (52). Microorganisms may enter via defective margins and colonize a poorly sealed root canal (60) (Fig. 18.3). Furthermore, leaking saliva may dissolve the sealer and break the resistance against reinfection (63). However, provided that instrumentation and root fillings are carefully performed, the problem of coronal leakage may not be of great clinical importance (58).
The placement of a post in the root canal does not influence the outcome of endodontic treatment per se. However, the post preparation might break the root filling seal either by disturbing the adaptation of the material to the dentinal walls or by leaving too little gutta-percha remaining. Studies have shown that not less than 3 mm should remain in the apical part of the canal (35).
Prevalence of endodontic “failures”
Assessment of the technical quality and the outcome of endodontic treatment at a population level has a long tradition in the Scandinavian countries. Studies have reported a relatively high frequency of defective root fillings. It has been reported consistently that 25–35% of endodontically treated teeth are associated with periapical radiolucencies (8, 17, 21, 50). Similar findings during recent years have been reported from other areas of Europe and North America as well as in Asia (12, 14, 15, 26, 39, 61, 62, 74) (see also Chapter 17). The most frequently adopted study design, the cross-sectional survey, does not disclose the dynamics of the periapical reactions and therefore does not provide direct information on the frequency of “failed” treatments. However, in a followup study, Petersson et al. (48) found about equal numbers of healing and developing periapical radiolucencies in a cohort followed over a period of 11 years. Obviously there is a contradiction between what is possible with endodontic therapy (85–90% success) and what is actually obtained (60–70% success). It is an important task for the profession to try to close this gap.
Fig. 18.3 In the first left upper premolar, an acute periapical lesion developed 1 year after placement of the post and crown. The root filling seal is defective and microorganisms probably have entered the canals either via microleakage or during the restorative procedures.
At present the number of potential retreatment cases is huge; in Sweden (9 million inhabitants) it can be estimated to be about 2.5 million. However, the attitude to the clinical management of such cases has been found to vary substantially among clinicians (5, 25, 49, 54, 55, 66).
Variation in the management of periapical lesions in endodontically treated teeth
Variation in health care procedures was recognized early, at the beginning of the 20th century. In a classical study (4) of 1000 11-year-old schoolchildren in New York City it was found that 650 children had undergone tonsillectomy. The remaining 350 children were sent to a group of physicians. A total of 158 children were selected for tonsillectomy. Those rejected (182) were sent to another group of physicians and 88 of them were then suggested for tonsillectomy. After that, the remaining children were examined by a third group of physicians, and then only 65 children remained for whom tonsillectomy had not been suggested. At that point the study was interrupted owing to a shortage of physicians to consult. This report inspired investigators to challenge the clinical consensus of a variety of medical (and dental) procedures. Troubled over the results of these studies, Eddy (18) concluded:
“Uncertainty creeps into medical practice through every pore. Whether a physician is defining a disease, making a diagnosis, selecting a procedure, observing outcomes, assessing probabilities, assigning preferences, or putting it all together, he is walking on a very slippery terrain. It is difficult for nonphysicians, and for many physicians, to appreciate how complex these tasks are, how poorly we understand them, and how easy it is for honest people to come to different conclusions.”
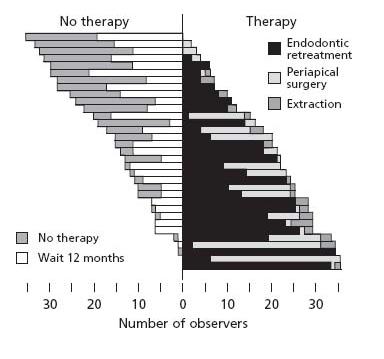
The large variation among clinicians when suggesting the treatment or retreatment of endodontic cases was first demonstrated by Smith et al. (66). Several reports have confirmed that the mere diagnosis of a persistent periapical radiolucency in an endodontically treated tooth does not consistently result in suggestions for retreatment among clinicians (48, 49, 54) (Key literature 18.2). For example, Reit and Gröndahl (55) found that only 39% of persistent periapical lesions diagnosed by practitioners were followed by a retreatment decision.
Owing to their complexity, clinical decision problems have attracted interdisciplinary attention. In addition to interest from health professionals, philosophers, psychologists and economists have also contributed (16). Two main areas of research and thinking can be identified: descriptive and prescriptive. Descriptive projects aim at mapping out and explaining how clinicians reason and make decisions. Prescriptive, or normative, projects, on the other hand, are concerned with how decisions should or ought to be made.
Clinical decision making: descriptive projects
In studies of clinical reasoning several models have been suggested and used (16). Some investigators have focused on the artistic, or intuitive, aspects of clinical practice (51). In the tradition of “judgment analysis”, researchers have tried to reveal the pieces of information or “cues” used at conscious or unconscious levels that influence a person’s decision-making policy. This approach has been applied in several domains (10), including judgments of third molar removal (29). In a series of innovative investigations Kahneman et al. (28) explored a proposition that people most often rely on a small number of heuristic principles to make decisions.
Attempts have been made to explain the observed variation in the management of periapical lesions in endodonticall/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses