Chapter 17
Use of Autogenous Bone Material for Implant Rehabilitation in the Bone Deficient Maxilla
Introduction
Surgical techniques today enable us to reconstruct bone-deficient regions equally well in the maxilla and the mandible. Bone grafting techniques, using autogenous bone from the iliac crest, mandibular symphyseal region, mandibular angle or cranium, can provide material for reconstruction purposes. Onlay grafting is especially indicated for defects, thin ridges and as a complement to inlay grafting. Inlay grafting, in combination with orthognathic surgery, has a predictable outcome. The sinus lifting technique is especially useful for reconstruction in the bone deficient posterior maxilla.
Background
Functional rehabilitation with dental implants has been in practical use for over 40 years with extremely good results. Early long-term studies over 15 years, in rehabilitation of edentulous mandibles, show success rates of over 90%. Edentulous, resorbed mandibles were the most problematic situations and these were also where fixed implant bridge solutions were most indicated. The long-term results have been remarkably good, which today means that it is possible to have immediate loading in most edentulous mandibles. The maxillary region is more problematic, especially with regard to the anatomic situation, where the maxillary sinus and nasal cavity occupy large areas. The cortical structure of the bone tissue in the maxilla is not the same as in the mandible, due to factors such as muscle influence on the mandible. The fact that the mandible is the mobile part of the chewing system explains some of the differences between the two jaws. The edentulous maxilla may require much more augmentation than the edentulous mandible, in order to be suitable for implant rehabilitation. There is a spectrum of surgical techniques available today which enable us to solve all kinds of bone-deficient situations, equally satisfactorily in the maxilla and the mandible.
Bone Graft Sources
The most frequently used regions for bone graft harvesting are the mandibular angle region and the chin region when there is only need for a limited amount of bone graft. For larger reconstructions the iliac bone is by far the most used source for autogenous bone graft.
Cortical bone graft can be harvested from the mandibular chin on the buccal side. By use of a Lindeman drill or a round burr, or an oscillating saw, a piece of bone can be taken with due consideration to the incisor roots and the mental foramina (Fig. 17.1). It is recommended not to perforate the lingual cortex in order to avoid bleedings from the floor of the mouth.
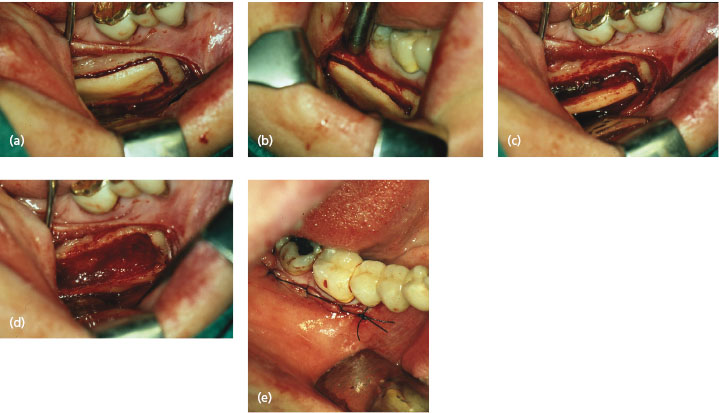
When harvesting bone graft from the angular region, the surgical approach is similar to the sagittal split approach. An incision is made outside the molar region extending up on the anterior ramus. The buccal part of the crest is exposed and a bone incision made outside the teeth into the marrow space. Vertical bone cuts are made on both sides of the horizontal and another one at the bottom of the planned graft area about one centimeter above the mandibular base.
The bone graft is splitted out with a chisel. With the right technique there should be no interference with the nerve canal (Fig. 17.1).
When there is a need for larger amount of bone graft you have to harvest from the iliac bone (Fig. 17.2). While harvesting bone graft from the mandible is made in local anesthesia harvesting from the iliac bone has to be made in general anesthesia.
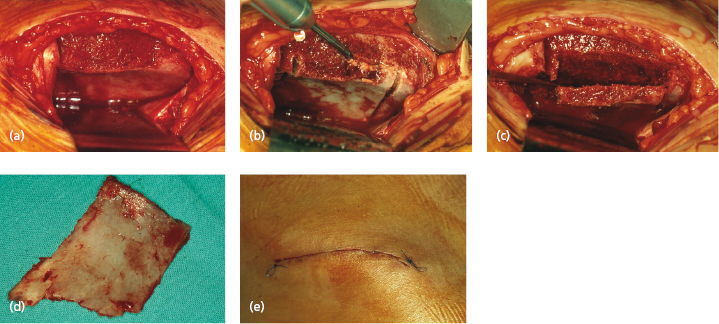
There are several different approaches to the iliac bone but it is an advantage for the patient to have an unchanged contour of the iliac crest after the surgical procedure.
In our experience the periosteum together with the upper part of the selected graft region (Fig. 17.2) is cut and bent aside and the medial surface of the iliac bone exposed. An oscillating saw can be used to take the desired amount of graft; bleedings are stopped eventually by use of bone wax and the wound closed. The upper loose bony part of the crest can now be fixated with plate screws and the skin incision sutured. A drain can be used for the first 24 hours.
Aspects of Bone Graft Behavior
Autogenous bone graft material is the gold standard for reconstruction of bony defects in the facial skeleton, such as tumor resections, congenital defects or atrophy of the jaws. Fresh, immediately harvested bone graft is by far the most reliable. The bone graft may then be replaced by new bone by osteoconduction or by osteoinduction through surviving osteogenic cells. The microvascular system in the bone graft may also make minor anastomosis with the surrounding vital tissue and revascularize the graft material. The predictability of the graft volume has not always been certain. Postoperative resorption may radically reduce the volume by up to 50–70% of the graft when it is in a passive state. Several factors may be of importance in maintaining as much bone graft volume as possible. Recent literature reviews indicate that the embryonic origin is important for the graft survival. Membranous bone should be superior to endocondral bone with less resorption over time. The revascularization of the graft is extremely important for starting new bone formation. Another important factor in preserving bone graft volume is rigid fixation of the graft, probably because this creates an appositional phase earlier, and thereby promotes improved osteoconduction.
The recipient bed for the bone graft may also be of importance for graft survival and volumetric changes. The influence of the bone graft recipient site on the survival of onlay bone grafts has been studied in several publications. The degree of contact between bone graft and recipient site as well as the orientation of the bone graft may have a significant effect on remodeling of vascularized bone grafts. Cortical preparations of the recipient bone marrow site allow exposure of osteogenic stem cells to the graft and may improve bone healing. Several publications support the theory that perforated bone is superior to unperforated. The perforations may increase initial healing of the bone graft, but there is no evidence that they help to maintain bone graft volume. Osteopromotive membranes have been used to improve bone graft survival and stability; these allow free diffusion of tissue fluid and prevent cellular ingrowth from adjacent connective tissue.
Block or Particulated Bone
Bone block grafts are structurally stable and initially resistant to resorption. The autogenous bone block will be almost totally necrotic after the grafting procedure and needs revascularization to survive. Incorporation of the graft is initiated by an inflammatory reaction during the first weeks, which then turns into a granulation phase, followed by osteoclastic activity. The new bone in and around the bone block is formed by creeping substitution and development of lamellar bone. This process proceeds gradually and has not reached normal physiological strength until 1 year. Normal biological properties are not present for at least 2 years, and part of the block will still contain residual necrotic original bone. Mechanical strength will be reduced during the first year.
Particulated bone graft can be both cortical and cancellous. Particulation can be done with a bone mill or the bone can be cut into pieces with bone scissors. Cancellous particulated bone has a larger surface area exposed to the surrounding tissue and vascular ingrowth may proceed faster than in bone block grafts. Compared to cortical graft it regains biological properties faster but it is also more exposed to resorption activities. The cancellous bone graft gradually increases in mechanical strength and it takes 1–2 years to reach normal mechanical strength, much like the bone block graft.
Onlay Grafting
Different methods for reconstruction of the atrophic maxilla can be used, depending on the actual situation. An atrophic alveolar ridge, with sufficient height but which is too thin, may be suitable for onlay grafting, where bone graft from either the hip or the mandible can be used for augmentation. Onlay grafting aims to widen the crest and make it possible for implant insertion. It is very important not to reduce the vertical height of the crest, since vertical augmentation may be very difficult to achieve.
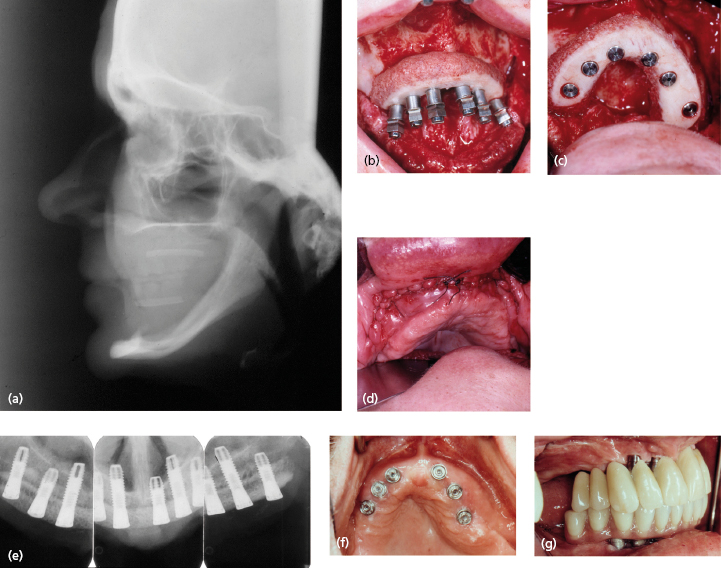
The first attempts to treat severely resorbed maxillae were made in the 1980s with large horseshoe-shaped bone blocks grafted to the maxillary ridge (Fig. 17.3). Technical difficulties with the technique made it unpredictable and there was a relatively high morbidity rate.
The buccal onlay grafting technique is useful in the posterior mandible as well as in the maxillary alveolar process. To achieve as good a result as possible it is advisable to make small perforations in the buccal cortical bone before attaching the graft with plate screws. If there is a discrepancy between the graft and the host bed it is also advisable to put bone graft material in the space to optimize the contact between bone graft and crest. The bone graft may be harvested from the mandibular angle, chin region, iliac crest or cranial sites. The most important issues in this procedure are to achieve rigid fixation of the bone graft and to close the covering soft tissue in such a way as to prevent microorganisms from the oral cavity entering the grafted area. The flap covering the bone graft should have a relaxed position and not be forced into a position by use of a strong suture. If this is not achieved, the graft may be totally destroyed due to wound dehiscence and compromised vascular blood supply.
A large onlay graft was the initial method of choice for reconstruction of the resorbed edentulous maxilla. The bone graft was obtained from the iliac bone beneath the iliac crest not involving the arch of the crest (Fig. 17.3a, b). The horseshoe-shaped bone graft was modeled to fit on to the exposed upper jaw crest (Fig. 17.3b). The remaining, exposed crest of the upper jaw was ground to fit the graft better and the cortex was perforated with a small round drill to form a better vascular bed for the grafted bone. After modeling of the bone graft to fit on to the crest, implants could be inserted into the graft and retained in the residual crestal bone in a one-stage procedure; alternatively the graft could be attached to the crest with plate screws in a two-stage procedure, thus allowing the graft to become more vascularized before implant insertion. The choice of a one- or two-stage concept depends, of course, on the amount of available bone volume. More residual bone allows for a better and safer implant stability and is therefore more suited for one-stage procedures. Large onlay block grafts have been shown to achieve a good result in long-term follow-up with one-stage implant surgery and also with a two-stage surgical technique.
Long-term clinical and radiographic follow-up studies have shown very good success and survival rates with onlay grafts with only minor drawbacks.
With all autogenous bone grafts, healing follows the same principles, according to Wolf’s law. The bone graft has to be functionally stimulated in order not to be resorbed. So a bone graft without functional stimulation by chewing through implants will resorb more or less completely. This functional stimulation is very well achieved by the implants. One should always allow for some remodeling resorption where excess bone graft material will disappear.
Bone graft will always adapt to functional load and stimulation. Thus in the horseshoe-shaped iliac bone grafts with excess volume outside the implants, functional remodeling, especially in a buccal–lingual direction was clearly evident. In patients with a retrognathic position at the upper jaw this resorption of 2–3 mm was negative since the retrognathic look of the maxilla was still noticeable even after implant surgery.
A technical problem of onlay grafting for small and larger surgical procedures is that the additional bone material has to be covered by a vital, vascularized flap, which must not be stretched or damaged. Careful closure of the incision without communication with the oral cavity is another important factor for a successful result. Big bone blocks for treatment of edentulous maxillae are especially vulnerable since there is so much foreign material to be incorporated within the tissue. Therefore it is of utmost importance to have as thick a flap as possible, with good vascularization to form a tension-free cover over the bone graft material (Fig. 17.3d).
The onlay bone graft can be attached to the residual crest with either the implants (one-/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


